Abstract
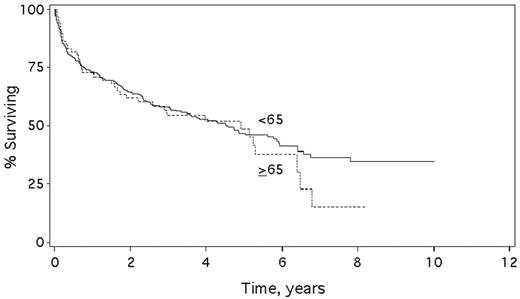
Over the past 10 years, HDM/SCT has been employed for treatment of patients with AL amyloidosis. Although peri-transplant mortality is greater than for other hematologic diseases, HDM/SCT leads to durable hematologic complete responses (CR), improvements in organ function, and extended survival in a substantial proportion of patients (Skinner et al., Ann. Int. Med. 2004). In that study, the proportion of patients eligible for HDM/SCT was lower for patients >65 years of age than for younger patients (34.3% vs. 68.4%), but the hematologic complete response (CR) rate and survival appeared to be no different. Here, we update these results and present a detailed analysis of outcomes in patients >65 vs. those <65. Data were collected with IRB approval. Through 07/01/04, 349 patients began G-CSF mobilization, of which 66 (19%) were >65. The median age of the 66 patients was 68, range 65–80; 73% male; 18% ? and 82% ?, while for the 283 patients <65, the median age was 55, range 29–64; 57% male; 16% ? and 84% ?. The median number of involved organs was no different in the two groups, nor was the type of organ involvement or performance status. There was also no difference in the rate of serious complications during stem cell collection, as a similar fraction of patients in both groups did not proceed to transplant, 12.1% of patients >65 versus 10.3% of patients <65 (p=.659). Based on treatment protocol, only 19% of patients >65 received an IV dose of melphalan of 200 mg/m2 (the remainder being treated with 140 mg/m2 or less), vs. 64% of those <65 (p <.001). There was no difference in early transplant-related mortality (10.3% in patients >65 vs. 13.4% in patients <65, p=.665). There was also no difference in one year mortality (22.4% for those >65 vs. 20.9% for those <65, p=.859). There was a non-significant trend towards a lower rate of hematologic CR in the older patients (32% vs. 44%, p=0.155). However, the median survival after HDM/SCT was no different (see fig; 4.9 years for patients >65 vs. 4.6 years for those <65, p=0.42 by log-rank test). Thus, while fewer patients >65 meet eligibility requirements for HDM/SCT, for those who do, treatment-related mortality, hematologic CR rate, and survival are no different than for younger patients. These data strongly support the use of HDM/SCT for suitable patients with AL amyloidosis who are >65 years old.
Figure.
Author notes
Corresponding author

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal