Abstract
Doxorubicin-based immunochemotherapy, with interferon, has been shown to improve survival in patients with advanced follicular lymphoma. High-dose chemotherapy with stem-cell support is effective in follicular lymphoma in relapse but remains controversial as a first-line therapy. In a randomized study using a purged autologous stem-cell support, we compared these 2 approaches in patients with advanced follicular lymphoma. Newly diagnosed advanced follicular lymphoma patients (172 patients) were randomly assigned either to an immunochemotherapy regimen (cyclophosphamide, doxorubicin, teniposide, prednisone, and interferon) or to a high-dose therapy followed by purged autologous stem-cell transplantation. Compared with the patients who received chemotherapy and interferon, patients treated with high-dose therapy had a higher response rate (69% vs 81%, P = .045) and a longer median event-free survival (not reached vs 45 months). This did not translate into a better survival rate due to an excess of secondary malignancies after transplantation. The Follicular Lymphoma Prognostic Index identified a subgroup of patients with a significantly higher event-free survival rate after high-dose therapy. Autologous stem-cell transplantation cannot be considered as the standard first-line treatment of follicular lymphoma for patients younger than 60 years old with a high tumor burden.
Introduction
Follicular lymphomas are a subgroup of B-cell non-Hodgkin lymphomas, accounting for 15% to 30% of newly diagnosed lymphomas.1-3 Median survival varies from 5 to 10 years depending on the prognostic factors at diagnosis and response to first-line therapy.4-6 Whatever the treatment, no plateau appears on survival curves, and virtually all patients relapse; follicular lymphomas are ultimately progressive, and fatal.2,3,5 No reference first-line treatment is clearly defined. One of the most active therapies is still doxorubicin-based chemotherapy with or without interferon.7-9 New therapeutic approaches including purine analogs and anti-CD20 monoclonal antibody are promising and are progressively included in the management of these lymphomas.2,3,10-13 The role of high-dose therapy (HDT) as a salvage treatment for patients with relapsing follicular lymphoma is demonstrated by some authors; several reports have shown the superiority of HDT followed by autologous stem-cell transplantation, purged or unpurged, compared with conventional chemotherapy in terms of no relapse and overall survival.14-18 Only a few reports have been published showing HDT results as a first-line treatment for poor-risk patients with follicular lymphoma, and the results remain controversial.19-26 These data prompted the French Groupe Ouest-Est des Leucémies et Autres Maladies du Sang (GOELAMS) to conduct a prospective randomized trial using patients with newly diagnosed follicular lymphoma with a high tumor burden. A combined doxorubicin-based chemotherapy associated with interferon was compared to front-line HDT followed by purged autologous stem-cell transplantation.
Patients and methods
Patients
This multicenter trial enrolled patients 18 to 60 years old with previously untreated histologically proven follicular lymphoma, classified according to the Working-Formulation criteria of the National Cancer Institute (B, C, or D lymphoma)27 and reviewed according to the Revised European-American Lymphoma classification (REAL) of the International Lymphoma Study Group (grades 1 to 3 center follicle lymphoma).28 Patients with transformed lymphoma were excluded. One pathologist centrally reviewed all the diagnostic slides. Another inclusion criterion was an Ann Arbor stage of II to IV and a high tumor burden defined according to the GELF (Groupe d'Etude des Lymphomes Folliculaires) criteria6,8 —that is, the presence of at least one adverse risk factor: B symptoms (more than 10% body mass lost in the previous 6 months, fever higher than 38°C during at least 2 weeks, drenching night sweats); a single lymph node larger than 7 cm, or involvement of at least 3 nodal sites larger than 3 cm; massive splenomegaly (costal overflow greater than 5 cm or a scan image of 20 cm along the main axis); lactate dehydrogenase (LDH) or β2 microglobulin levels higher than normal values; an Eastern Cooperative Oncology Group (ECOG) performance status of 2; compressive symptoms or serous effusions; a measurable disease; the absence of underlying organ dysfunction precluding the use of anthracycline or high-dose chemotherapy; and the absence of infection with the human immunodeficiency virus. The recently described Follicular Lymphoma International Prognostic Index (FLIPI) (ie, a maximum of 5 possible adverse prognostic factors regarding age, tumor stage, number of involved node sites, LDH concentration, and hemoglobin level) was not defined at the onset of the protocol. All necessary data were available and the FLIPI was calculated retrospectively at the time of analysis.5 The trial was approved by the ethics committee of the Région Centre, Tours, France, and all patients provided written informed consent in accordance with the Helsinki Declaration.
Staging, assessment of response, and follow-up
At diagnosis, in addition to a background review, physical examination, routine laboratory tests, and bone marrow biopsy, all patients were evaluated for abdominal and thoracic involvement using computed tomography imaging or ultrasonography. The procedures used to evaluate responses were the same as those used for staging at diagnosis. Follow-up procedures included a physical examination every 3 months for the first 2 years, every 6 months for the next 2 years, and annually thereafter. Thoracic and abdominal computed tomography was performed every 6 months during the first 2 years, and annually thereafter. Marrow examinations were planned at the end of treatment, 6 and 12 months later, and annually thereafter. Molecular analyses were not routinely conducted and were not taken into account during the staging or evaluation procedures. The report of the international workshop to standardize response criteria for non-Hodgkin lymphomas29 was not published at the time of study design, and responses were as follows. A complete response (CR) was defined by the disappearance of all documented disease. A very good partial response (VGPR) was defined by a reduction of at least 80% in the largest diameter of all measurable lesions with or without the persistence of bone marrow involvement, defined by the sole presence of paratrabecullar lymphomatous nodules. A partial response (PR) was defined by a reduction of at least 50% in the largest diameter of every measurable lesion, even if bone marrow involvement persisted. In each group, the treatment was considered a failure if the disease continued to progress before the end of the treatment program and, in the HDT group, if they did not have at least a partial response before grafting. Such patients were offered a salvage therapy, which varied among the centers. The frequency and severity of adverse effects was recorded according to the World Health Organization (WHO) classification.30
Treatments
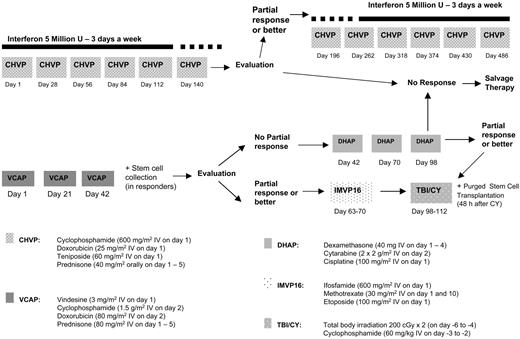
In the standard chemotherapy arm, the CHVP (cyclophosphamide, low-dose doxorubicin, teniposide, and prednisone) regimen consisted of cyclophosphamide (600 mg/m2), doxorubicin (25 mg/m2), and teniposide (60 mg/m2), all administered intravenously on day 1, and prednisone (40 mg/m2), administered orally on days 1 to 5.4,12 Treatment consisted of a 6-course induction phase administered monthly, followed, for responders and patients presenting a stable disease, by a maintenance phase that consisted of 1 cycle every 2 months for 1 year. Concomitant subcutaneous interferon alfa-2b was administered at 5 × 106 3 times a week for 18 months.
In the HDT arm, patients received the VCAP (cyclophosphamide, high-dose doxorubicin, prednisone, and vincristine) regimen as a first-line therapy combining vindesine (3 mg/m2) on day 1, cyclophosphamide (1500 mg/m2) on day 2, doxorubicin (80 mg/m2) on day 2, and prednisolone (50 mg/m2) on days 1 to 5, every 3 weeks.19,31,32 Patients in CR, VGPR, or PR after the second or third VCAP cycle continued on to stem-cell harvesting and received, before transplantation, one course of IMVP16 (ifosfamide, methotrexate, and VP-16), which combined ifosfamide (1.5 g/m2) and VP16 (100 mg/m2) on days 1 through 3, and methotrexate (30 mg/m2) on days 1 and 10. Patients with less than PR after the VCAP cycles received, as salvage therapy, 2 to 3 courses of DHAP (dexamethasone, high-dose cytarabine, and cisplatin) combining cisplatine (100 mg/m2) on day 1, cytarabine (4 g/m2) on day 2, and dexamethasone (40 mg/m2) on days 1 through 4. If at least a PR was obtained after DHAP, stem cells were harvested or patients were considered as failures. Stem cell purging was offered to all patients in the 25 recruiting centers if the collected grafts were more than 1 × 108 mononuclear cells/kg. Purging was performed according to the local center's procedures, immunological purging with immunomagnetic beads, or CD34+ cell selection. As previously described,19 the immunomagnetic purging technique was completed using the Max SEP system (Baxter Immunotherapy Division, Munich, Germany) and 5 monoclonal antibodies (anti-CD19, anti-CD20, anti-CD22, anti-CD23, and anti-CD37). Selection of CD34+ cells was performed according to the manufacturer's instructions (Ceprate SC Stem Cell Concentration System; Cellpro, Bothell, WA)19 and the collected cells were cryopreserved after purging. If the graft did not contain at least 1 × 104 ganulocyte-macrophage colony-forming units (CFU-GMs) for marrow and more than 2 × 104 for peripheral blood stem cells, the procedure was considered to have failed, patients were not given transplants, and patients then received treatment according to the local investigator's decision. The conditioning regimen started 4 to 6 weeks after the IMVP16 or the last DHAP cycle in responding patients and included cyclophosphamide (60 mg/kg body weight) infused on each of 2 consecutive days after total body irradiation, administered in fractionated doses (200 cGy) twice daily on 3 consecutive days in all patients. Stem cells were reinfused within 48 hours of the completion of the conditioning regimen (Figure 1).
Statistical analysis
Randomization was carried out centrally and was stratified according to each center. Statistical analysis was performed with SPSS software version 11.5 (SPSS, Chicago, IL). Overall survival and event-free survivals were calculated according to the Kaplan-Meier method.33 Survival was measured from the time of randomization to death from any cause or the date of last contact. Event-free survival (EFS) was calculated from the time of randomization; progression, the absence of at least a partial response on the intermediate evaluation, relapse, and death in remission were considered events. The log-rank test was used to compare survival in the 2 groups. The analysis was performed on an intention-to-treat basis. Multivariate analysis of survival was performed with the use of the Cox model. Potential interactions between treatment and risk factors were also assessed in the model. The trial was designed to detect an absolute difference in EFS of 25% at 3 years, with an α value of.05 and a β value of .2. Assuming an EFS rate at 5 years of 50% in the conventional group and 75% in the HDT group, this design required the randomization of 130 patients. Secondary endpoints were the response rate at the end of treatment, the overall survival rate, and the incidence of adverse effects.
Results
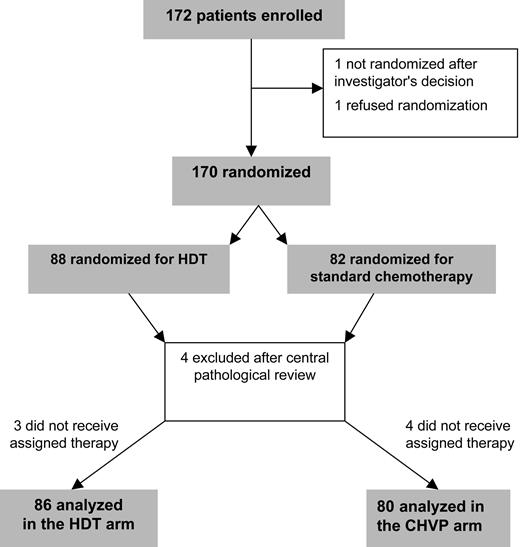
Between April 1994 and May 2001, 172 consecutive patients were enrolled in 25 centers. Six patients were found to be ineligible; 4 after the centralized pathological review, 1 after the investigator's decision, and 1 who refused to be submitted to randomization. Of the remaining 166 patients, 80 were assigned to the conventional therapy group and 86 to the HDT group; 7 patients did not receive the assigned treatment (Figure 2). Patient characteristics were similar in the 2 groups (Table 1), except that there were more women and B symptoms and fewer grade 3 follicular histologies in the conventional therapy group than in the HDT group (59% vs 40%, P = .017; 35% vs 16%, P = .009; and 3% vs 15%, P = .03, respectively).
Initial characteristics of the patients according to the treatment group CHVP versus HDT
Characteristics . | CHVP . | HDT . | P . |
|---|---|---|---|
| B symptoms present, no. | 28 | 14 | .009 |
| Sex, M/F, no. | 47/33 | 38/48 | .017 |
| Histology, no. | .03 | ||
| Grade I | 40 | 28 | |
| Grade II | 38 | 50 | |
| Grade III | 2 | 8 | |
| Ann Arbor stage, no. | .1 | ||
| II | 6 | 4 | |
| III | 22 | 8 | |
| IV | 52 | 64 | |
| Performance status grade, no. | .11 | ||
| 0 | 44 | 39 | |
| 1 | 35 | 38 | |
| 2 or greater | 1 | 9 | |
| Median age, y (range) | 50 (29-61) | 51 (32-60) | .15 |
| Serum LDH greater than normal, no. | 32 | 24 | .41 |
| FLIPI, no. | .4 | ||
| Low | 23 | 26 | |
| Intermediate | 31 | 40 | |
| High | 26 | 20 | |
| Mass greater than 10 cm, no. | 28 | 25 | .77 |
Characteristics . | CHVP . | HDT . | P . |
|---|---|---|---|
| B symptoms present, no. | 28 | 14 | .009 |
| Sex, M/F, no. | 47/33 | 38/48 | .017 |
| Histology, no. | .03 | ||
| Grade I | 40 | 28 | |
| Grade II | 38 | 50 | |
| Grade III | 2 | 8 | |
| Ann Arbor stage, no. | .1 | ||
| II | 6 | 4 | |
| III | 22 | 8 | |
| IV | 52 | 64 | |
| Performance status grade, no. | .11 | ||
| 0 | 44 | 39 | |
| 1 | 35 | 38 | |
| 2 or greater | 1 | 9 | |
| Median age, y (range) | 50 (29-61) | 51 (32-60) | .15 |
| Serum LDH greater than normal, no. | 32 | 24 | .41 |
| FLIPI, no. | .4 | ||
| Low | 23 | 26 | |
| Intermediate | 31 | 40 | |
| High | 26 | 20 | |
| Mass greater than 10 cm, no. | 28 | 25 | .77 |
For CHVP, n = 80; for HDT, n = 86.
CHVP indicates cyclophosphamide, doxorubicin, etoposide, prednisone; HDT, high-dose therapy; and FLIPI, Follicular Lymphoma Prognostic Index.
Feasibility of the treatment
Overall, 83.5% of the patients completed the assigned treatment; 77% of those in the reference chemotherapy group and 90% of those in the HDT group. In the reference group, interferon was discontinued before the end of induction for 5 patients; the dose of interferon was reduced because of mild intolerance for 12 patients during the first 3 months and for 13 additional patients during the following 3 months. In the HDT group, hematopoietic stem-cell collection was performed in 77 patients after VCAP + IMVP16 or DHAP regimens (65 peripheral blood stem-cell collection primed with GM-CSF [colony-stimulating factor] or 12 bone marrow harvest). Purging was performed in all but 9 patients, immunologic purging with immunomagnetic beads in 10 cases, and CD34+ cell selection in the 58 remaining cases. The main reason for not completing the treatment was the lack of an early response or disease progression (combined incidence, 21% in the reference chemotherapy group and 6% in the HDT group). There was no early death related to the treatment in either group; 2 assigned patients did not receive grafts due to the absence of a sufficient graft; 4 cases of severe treatment-related effects precluding further therapy were observed in the HDT group, and 1 in the CHVP group.
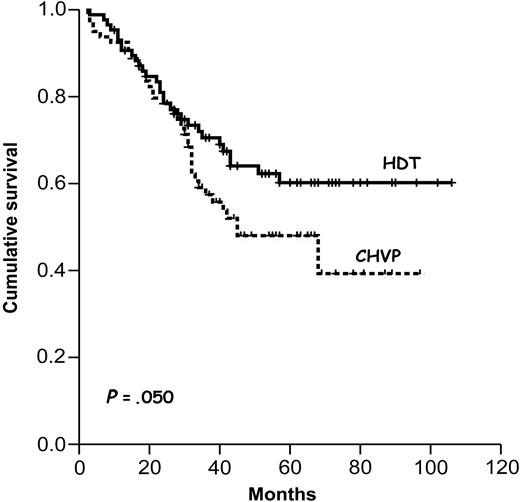
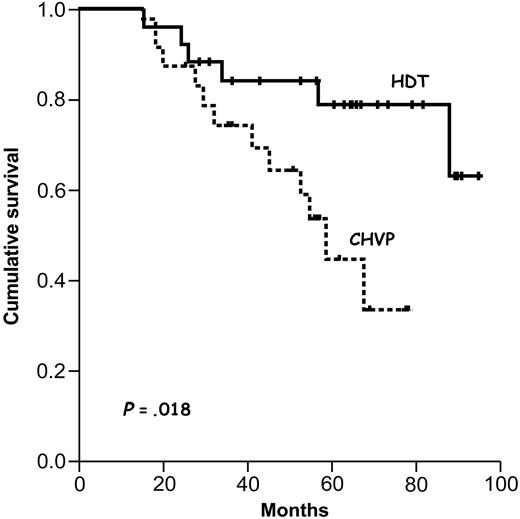
Event-free survival according to treatment group. HDT indicates high-dose therapy group; CHVP, standard chemotherapy group.
Event-free survival according to treatment group. HDT indicates high-dose therapy group; CHVP, standard chemotherapy group.
Response to treatment
The overall response rates (CR + VGPR + PR) were 84% after the CHVP induction chemotherapy phase (the first 6 monthly cycles), 81% after the 3 VCAP cycles, and 90% after the salvage DHAP therapy. The overall response rates at the end of the treatment were 69% in the reference chemotherapy group (after the completion of the 12 cycles) and 81% in the HDT group (after the transplantation procedure); the rates of CR + VGPR were 81% and 55%, respectively (P = .045). After a median follow-up of 5 years for the entire cohort, longer median EFS was observed after HDT (not reached vs 45 months).
Survival
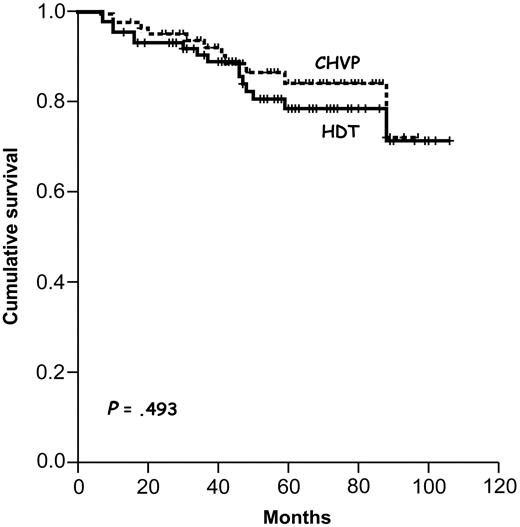
The estimated (± SD) overall and EFS rates were 82% ± 7% and 51% ± 5%, respectively. According to the intention-to-treat analysis, the EFS rates at 5 years differed significantly between the reference chemotherapy and HDT groups (48% ± 7% vs 60% ± 6%, P = .050; Figure 3); the overall 5-year survival rate did not differ significantly between groups (Figure 4, Table2). Among patients with a poor risk according to FLIPI (>2), high-dose treatment yielded significantly higher rates of EFS (67% ± 9% vs 20% ± 10%, P = .018; Figure 5) but not of overall survival (82% ± 6% vs 73% ± 7%, P = .15). For patients with a good or intermediate risk (≤2), the rates of overall survival and EFS were similar in the 2 groups (Table 2). The multivariate analysis showed that overall survival was independently affected by older age (P = .001), and to a lesser extent, by an elevated initial LDH level (P = .09) and poor FLIPI (P = .055). Event-free survival was independently affected by older age (P = .001), the type of treatment (P = .050), and FLIPI (P = .025). Overall, 25 patients died, 16 in the HDT group and 9 in the reference chemotherapy group. Lymphoma was the main cause of death (72%), and 7 patients, all in the HDT group, died of secondary malignancies.
Overall survival according to treatment group. HDT indicates high-dose therapy group; CHVP, standard chemotherapy group.
Overall survival according to treatment group. HDT indicates high-dose therapy group; CHVP, standard chemotherapy group.
Five-year event-free and overall survival of patients treated in the protocol: CHVP vs HDT
Parameter . | Total no. of patients . | Event-free survival, % . | P . | Overall survival, % . | P . |
|---|---|---|---|---|---|
| CHVP | 80 | 48 | .050 | 84 | .49 |
| HDT | 86 | 60 | 78 | ||
| Age | .28 | .060 | |||
| 40 y and younger | 23 | 58 | 73 | ||
| Greater than 40 y | 143 | 52 | 85 | ||
| ECOG status | .13 | .11 | |||
| 0-1 | 156 | 56 | 80 | ||
| 2 or greater | 10 | 75 | 100 | ||
| Lymph node areas | .037 | .19 | |||
| 4 | 83 | 61 | 84 | ||
| More than 4 | 73 | 45 | 78 | ||
| LDH | .19 | .09 | |||
| Normal | 110 | 62 | 85 | ||
| Normal or higher | 56 | 51 | 72 | ||
| Hb level | .38 | .41 | |||
| Less than 12 | 48 | 50 | 79 | ||
| 12 or greater | 118 | 66 | 85 | ||
| Stage | .92 | .82 | |||
| I-II | 10 | 53 | 75 | ||
| III-IV | 156 | 60 | 81 | ||
| FLIPI | .047 | .11 | |||
| Good | 37 | 67 | 92 | ||
| Intermediate | 79 | 64 | 76 | ||
| Poor | 50 | 37 | 75 | ||
| Good + intermediate | 116 | 56 | .025 | 78 | .055 |
| FLIPI | |||||
| Good + intermediate | 116 | .30 | .14 | ||
| CHVP | 56 | 50 | 87 | ||
| HDT | 60 | 58 | 77 | ||
| Poor | 50 | .018 | .15 | ||
| CHVP | 24 | 20 | 73 | ||
| HDT | 26 | 67 | 82 | ||
| HDT, purged grafts | 61 | .019 | .014 | ||
| CD34+ selection | 53 | 69 | 84 | ||
| B-ceil depletion | 8 | 27 | 42 |
Parameter . | Total no. of patients . | Event-free survival, % . | P . | Overall survival, % . | P . |
|---|---|---|---|---|---|
| CHVP | 80 | 48 | .050 | 84 | .49 |
| HDT | 86 | 60 | 78 | ||
| Age | .28 | .060 | |||
| 40 y and younger | 23 | 58 | 73 | ||
| Greater than 40 y | 143 | 52 | 85 | ||
| ECOG status | .13 | .11 | |||
| 0-1 | 156 | 56 | 80 | ||
| 2 or greater | 10 | 75 | 100 | ||
| Lymph node areas | .037 | .19 | |||
| 4 | 83 | 61 | 84 | ||
| More than 4 | 73 | 45 | 78 | ||
| LDH | .19 | .09 | |||
| Normal | 110 | 62 | 85 | ||
| Normal or higher | 56 | 51 | 72 | ||
| Hb level | .38 | .41 | |||
| Less than 12 | 48 | 50 | 79 | ||
| 12 or greater | 118 | 66 | 85 | ||
| Stage | .92 | .82 | |||
| I-II | 10 | 53 | 75 | ||
| III-IV | 156 | 60 | 81 | ||
| FLIPI | .047 | .11 | |||
| Good | 37 | 67 | 92 | ||
| Intermediate | 79 | 64 | 76 | ||
| Poor | 50 | 37 | 75 | ||
| Good + intermediate | 116 | 56 | .025 | 78 | .055 |
| FLIPI | |||||
| Good + intermediate | 116 | .30 | .14 | ||
| CHVP | 56 | 50 | 87 | ||
| HDT | 60 | 58 | 77 | ||
| Poor | 50 | .018 | .15 | ||
| CHVP | 24 | 20 | 73 | ||
| HDT | 26 | 67 | 82 | ||
| HDT, purged grafts | 61 | .019 | .014 | ||
| CD34+ selection | 53 | 69 | 84 | ||
| B-ceil depletion | 8 | 27 | 42 |
CHVP indicates cyclophosphmide, doxorubicine, vepesise, prednisone; HDT, high-dose therapy; and FLIPI, Follicular Lymphoma Prognostic Index.
Relapse and progression
Eighty-seven patients had progressive disease during the treatment or relapse (54 of 80 in the chemotherapy group and 33 of 86 in the HDT group; P = .045). The patients with progressive or relapsing disease received various salvage regimens with or without allogeneic or autologous stem-cell transplantation. The 5-year survival rate among these patients was 49% ± 10% in the HDT group and 75% ± 7% in the reference chemotherapy group (P = .07); 16 patients were autografted after a salvage regimen and 12 second CRs were obtained in this later group. In the HDT group, the CD34+ selection technique yielded better event-free and overall survival rates at 5 years as opposed to the negative purging method (69% ± 7% vs 27% ± 17%, P = .019; and 84% ± 9% vs 42% ± 17%, P = .014, respectively) (Table 2).
Event-free survival according to treatment arm and patients with a poor FLIPI score. HDT indicates high-dose therapy group; CHVP, standard chemotherapy group.
Event-free survival according to treatment arm and patients with a poor FLIPI score. HDT indicates high-dose therapy group; CHVP, standard chemotherapy group.
Adverse events
The median duration of hospitalization after the first course of chemotherapy was 1 day (range, 1 to 16 days) for CHVP and 4 days (range, 1 to 25 days) for VCAP. The median duration of hospitalization was 1 day for each of the subsequent courses of CHVP (range, 1 to 15 days), 3 days for the second course of VCAP (range, 1 to 17 days); 4 days for the course with ifosfamide, methotrexate, and vepeside (range, 3 to 11 days) and 5 days for the courses of DHAP (range, 4 to 18 days). Grades 3 to 4 hematologic toxicity was observed for 3 patients during the first 6 CHVP cycles, and 1 patient required platelets and red blood cell transfusions. No secondary malignancies were observed in the chemotherapy arm. After total body irradiation and high-dose cyclophosphamide, all patients had neutrophil counts of more than 0.5 × 109/L after a median of 11 days (range, 6 to 31 days) and a platelet count of more than 20 × 109/L after a median of 14 days (range, 7 to 54 days). The median hospitalization duration after this regimen was 24 days (range, 18 to 63 days). Fifteen patients had severe infections or septicemias, and 2 had interstitial pneumonitis. There was 1 grade-4 nonhematologic adverse event, 1 case of hemorrhagic cystitis, and 26 cases of mucositis, which was the most frequent grade-3 adverse event. There were 10 secondary cancers after autografting, 3 leukemias, 3 myelodysplasias, 2 breast cancers, 1 renal cancer, and 1 prostate cancer, of which 3 occurred in CR patients, and 7 were fatal. These secondary cancers occurred between 12 and 45 months after grafting and had an actuarial risk of 18.6% at 5 years. Age, sex, type of stem cells, and relapses after autografting did not influence the occurrence of secondary malignancies. Four leukemias or myelodysplasias occurred after purging with B-cell depletion (8 cases) and the other 2 after CD34+ selection (53 cases), with a P value of .021.
Discussion
Follicular lymphoma, although often associated with a prolonged course, is ultimately a fatal illness.1,5 If new therapeutic approaches including purine analogs and anti-CD20 monoclonal antibody are promising,10-12 one of the best treatments showing a prolongation of overall survival in patients with a high tumor burden was doxorubicin-based conventional chemotherapy associated with interferon.9 The place of autologous stem-cell transplantation in the therapeutic strategy of follicular lymphomas has not been clearly determined.2,3,34 A recent study of 89 patients indicates a considerable benefit in disease-free (P = .0037) and overall survival (P = .079) of autologous stem-cell transplantation compared with conventional chemotherapy in relapsing patients with follicular lymphoma, with a median follow-up of 6 years.16 However, few phase 2 studies of autologous transplantation as the first-line therapy of follicular lymphoma have been reported. Horning et al23 compared 37 patients treated with purged autologous marrow after a maximum response to conventional chemotherapy and 61 matched historical controls, most in CR or unconfirmed CR after conventional chemotherapy. With a median follow-up of 6.5 years, the estimated 10-year survival rate was 86% in the group who received transplants and 62% in the conventional treatment group (P = .074).23 Two large phase 3 trials have tested the value of autologous transplantation in first-line therapy in patients with follicular lymphoma.25,26 A German study is comparing a combined treatment of mitoxantrone, chlorambucil, and prednisone, followed by interferon maintenance with autologous stem-cell transplantation after a cyclophosphamide total body irradiation (TBI) conditioning regimen in patients with low-grade lymphoma. In patients who underwent autologous transplantation, the 5-year progression-free survival rate was 64.7%, and in the interferon maintenance arm, it was 33.3% (P < .0001). As expected, acute toxicity was higher in the autologous stem-cell transplantation (ASCT) group, but early mortality was below 2.5% in both study arms. In this randomized, multicenter trial, high-dose radiochemotherapy followed by ASCT significantly improved PFS compared with interferon in patients with follicular lymphoma when administered in combination at first remission. No difference was seen in overall survival but the follow-up was too short and data remained blinded for further analysis.26 The GELF 94 trial compared the same immunochemotherapy associating CHVP and interferon with 4 courses of CHOP (cyclophosphamide, doxorubicin, vincristine, prednisone) followed by cyclophosphamide and VP16 plus TBI and autologous stem-cell transplantation. Inclusion criteria were the same as in the GOELAMS trial: 401 patients were randomized and 71% of the patients in the HDT arm were given transplants with a median follow-up of 56 months; at 7 years, EFS was comparable (45% versus 36%) but overall survival was superior in the HDT arm (86% versus 74%).25 The GOELAMS study described here compared a very active conventional chemotherapy,8,9 which might be considered as a reference treatment, to autologous stem-cell transplantation with purged stem cells after TBI conditioning regimen.24 The results of the HDT arm were comparable to our previous pilot study19 and to those of intensive therapy phase 2 trials yet to be published.20-22 We showed that HDT is superior to conventional immunochemotherapy in terms of EFS but not in terms of overall survival. The patients who received the most benefit from the intensive procedure were those with an initial poor FLIPI. The program appeared feasible, with more than 90% of the patients randomized in the HDT arm actually receiving grafts. Despite the use of fractionated TBI containing the conditioning regimen, which is known to increase treatment-related mortality, no patients died during stem-cell transplantation. The Dana-Farber group initially reported a correlation between the outcome of transplantation and an optimal purging of stem-cell product.18 In a more recent publication,35 patients whose bone marrow was negative by polymerase chain reaction (PCR) for Bcl2/immunoglobulin H (IgH) rearrangement after purging experienced longer freedom from recurrence than those whose marrow remained PCR+; the 8-year freedom from relapse progression was 83% for PCR- and 14% for PCR+ patients. More recently, van Besien et al reported on 904 patients of the Autologous Blood and Marrow Transplant Registry/International Bone Marrow Transplant Registry (ABMTR/IBMTR) undergoing transplantation for follicular lymphoma;36 131 patients (14%) received purged autologous and 597 (67%) received unpurged autologous transplants; 5-year recurrence rates were 43% and 58% after purged and unpurged autotransplantations, and purged autotransplantations exhibited a 26% lower recurrence rate than unpurged ones. A multivariable analysis found an effect of stem-cell purging on recurrence rates (for early as well as for late relapses) and overall survival. Due to missing data, the PCR data in our multicenter study could not be evaluated. However, it appeared that the purging technique could play a role with a significant advantage, in terms of relapse, in favor of the CD34+ selection. McQuaker et al37 and Voso et al38,39 have shown the absence of t(14;18) PCR+ cells in purified CD34+ peripheral blood stem cells, and Gribben et al reported that the purging technique could influence the efficiency of this procedure.40
We observed a high rate of secondary malignancies, including myelodysplastic syndromes, acute leukemias, and other secondary tumors in the HDT arm. The 5-year incidence of these secondary cancers has been estimated to be 8% to 14%.17,34,41-43 The incidence excess in the transplantation arm was not described in the GELA (Groupe d'Etude des Lymphomes de l'Adulte) phase 3 trials, but was already reported in the German Low-Grade Lymphoma Study Group.26,44 It is unclear whether this increased risk of secondary tumors might counteract the benefit of autologous transplantation if we wait for a sufficient follow-up after the treatment ends.26 Some explanations could be argued: the use of a TBI-containing regimen, which has been shown to increase the incidence of secondary myelodysplastic syndromes or leukemias,34,43 the use of systematic cell purging, or a combination of both factors. At the time of this publication, in terms of overall survival, secondary cancers are responsible for the lack of benefit from autologous stem-cell transplantation. The improvement in the EFS rate, however, suggests a potential benefit for ASCT as a first-line therapy for a subgroup of patients with specific adverse prognostic factors such as a poor FLIPI at diagnosis and absence of a clinical or molecular complete remission after conventional first-line chemotherapy.
In conclusion, autologous stem-cell transplantation with ex vivo purging cannot be considered as the standard first-line treatment of follicular lymphoma for patients younger than 60 years old with high humor burden as defined in our study. In the future, other approaches have to be combined with autologous stem-cell transplantation to decrease the risk of relapse, such as improving the conditioning regimen with radioimmunoconjugates, or using rituximab as in vivo purging in place of ex vivo manipulations. We must always consider the increasing potential risk of secondary malignancies associated with these emerging tools.
Appendix
The Groupe Ouest-Est des Leucémies et des Autres Maladies du Sang (Comité Lymphome) included the following centers and principal investigators in France (no. of patients included in the protocol):
Besançon: Dr Deconinck, Dr Cahn (19); Tours: Dr Colombat, Dr Delain, Dr Cartron (16); Angers: Dr Foussard, Dr Ifrah, Dr François (15); Nantes CHU: Dr Milpied, Dr Rapp, Dr Mahé (14); La Roche-Sur-Yon: Dr Maisonneuve (12); Brest: Dr Berthou, Dr Sensebe, Dr Escoffre-Barbe (11); Poitiers: Dr Delwail (10); Montpellier: Dr Legouffe, Dr Rossi (10); Grenoble: Dr Gressin, Dr Sotto (10); Reims: Dr Vilque (9); Amiens: Dr Desablens, Dr Garidi (7); Saint-Etienne: Dr Jaubert (5); Nantes: Catherine de Sienne, Dr Ramée (4); Nice CAC: Dr Thyss (3); Nantes CAC: Dr A. Lemevel (3); Paris, Hôpital Européen Georges Pompidou: Dr Jenabian, Dr Le Maignan, Dr Andrieu, Dr Colonna (2); Orléans: Dr Lucas (2); Clermont-Ferrand: Dr Travade (2); Blois (1); Le Mans (1); Mulhouse (1); Rennes (1); Saint-Nazaire (1); Vannes (1); and Vendome (1).
Prepublished online as Blood First Edition Paper, February 1, 2005; DOI 10.1182/blood-2004-10-3920.
Supported in part by grants of the French Ministère de la Santé et de la Solidarité Sociale and the Schering-Plough Company.
A list of the members of the Groupe Ouest-Est des Leucémies et des Autres Maladies du Sang (GOELAMS) participating in the study appears in the “Appendix.”
Presented in oral sessions at the 43rd annual meeting of the American Society of Hematology, Orlando, FL, December 10, 2001; and the 45th annual meeting of the American Society of Hematology, San Diego, CA, December 9, 2003.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 U.S.C. section 1734.
We would like to thank Dr Paul Kretchmer (kretchmer@sfedit.net) at San Francisco Edit for his assistance in editing this manuscript. All authors participated in designing and performing the research; P.M. centralized the pathological review; E.D., P.B., R.D., and P.C. controlled and analyzed data; E.D. and P.C. wrote the paper; and all authors checked the final version of the manuscript. This study was designed by the GOELAMS lymphoma committee. The data were collected by the principal investigator at each participating center, checked for accuracy by the GOELAMS research assistants, and sent to the centralized database in Tours. The French Ministère de la Santé et de la Solidarité Sociale and the Schering-Plough Company had no role in designing the protocol, collecting, analyzing, or interpreting the data, or writing this article.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal