Abstract
B-cell chronic lymphocytic leukemia (B-CLL) is a clinically variable disease where mutations in DNA damage response genes ATM or TP53 affect the response to standard therapeutic agents. The in vitro cytotoxicity of a novel cyclin-dependent kinase inhibitor, CYC202, was evaluated in 26 B-CLLs, 11 with mutations in either the ATM or TP53 genes, and compared with that induced by ionizing radiation and fludarabine. CYC202 induced apoptosis within 24 hours of treatment in all 26 analyzed tumor samples independently of ATM and TP53 gene status, whereas 6 of 26 B-CLLs, mostly ATM mutant, showed marked in vitro resistance to fludarabine-induced apoptosis. Compared with B-CLLs, normal T and B lymphocytes treated with CYC202 displayed reduced and delayed apoptosis. Using global gene expression profiling, we found that CYC202 caused a significant down-regulation of genes involved in regulation of transcription, translation, survival, and DNA repair. Furthermore, induction of apoptosis by CYC202 was preceded by inhibition of RNA polymerase II phosphorylation, leading to down-regulation of several prosurvival proteins. We conclude that CYC202 is a potent inducer of apoptosis in B-CLL regardless of the functional status of the p53 pathway, and may be considered as a therapeutic agent to improve the outcome of resistant B-CLL tumors.
Introduction
B-cell chronic lymphocytic leukemia (B-CLL) is the most common leukemia of adults in the Western world and remains incurable with current chemotherapy. B-CLL cells have a characteristic phenotype typified by expression of CD5, CD19, and CD23 and low expression of surface immunoglobulins.1 Tumor cells are believed to accumulate primarily due to defects in apoptosis rather than uncontrolled proliferation, and this model is supported by the observation that most B-CLL cells remain in G0-G1 and demonstrate prolonged cell survival in vivo. The clinical course of the disease is remarkably variable, remaining stable for extended periods in some patients, while in others progression is much more rapid. The standard treatments for B-CLL include chlorambucil and purine analogs such as fludarabine. However, it has been difficult to demonstrate an improvement in overall survival following the introduction of fludarabine, and disease relapse is inevitable in virtually all patients treated with chemotherapy.2
TP53 is a critical tumor suppressor gene involved in the induction of apoptosis and onset of cell cycle arrest following DNA damage. We have reported previously that up to 30% of B-CLL tumors have a defect in the p53 pathway that result from mutations in either the ATM or TP53 gene.3,4 Most current anticancer treatments exert their effects through DNA damage and subsequent activation of the p53-dependent apoptotic pathway, and as such tumors that acquire mutations of genes in the p53 pathway are often associated with resistance to treatment.5 It is not surprising, therefore, that there is considerable interest in the development of novel treatments that may bypass these genetic lesions and indirectly activate apoptotic effector mechanisms.
Cyclin-dependent kinases (CDKs) are serine/threonine kinases that play a crucial regulatory role in the cell cycle and transcription by phosphorylation of transcription factors and tumor suppressor proteins involved in DNA replication and cell division.6-8 CDKs are, therefore, attractive therapeutic targets for cancer therapy. Recently, a pure R-enantiomer of the CDK inhibitor roscovitine, CYC202, emerged as a potent inducer of apoptosis in a variety of tumor cells, and phase 1 clinical studies in healthy volunteers have been completed.8-10 CYC202 is currently in phase 2a clinical trials in combination therapy with capecitabine for breast cancer and with gemcitabine/cisplatin for non–small cell lung cancer,7 while roscovitine was recently shown to be capable of inducing apoptosis in B-CLL cells in vitro.11
Given the greater potency of CYC202 over roscovitine against several key kinases,9 as well as its successful application in clinical trials, in this study we tested the efficacy of CYC202 to induce apoptosis in B-CLL cells with particular emphasis on tumors with a defective p53 pathway. In addition, we compared the in vitro ability of CYC202 to induce B-CLL apoptosis to the cytotoxic activities of fludarabine and ionizing radiation (IR). Finally, we addressed the apoptotic mechanism of CYC202 in B-CLL by analyzing global transcriptional responses to the drug.
Materials and methods
B-CLL tumors
Peripheral blood samples were collected from 26 patients with an age range of 52 to 93 years after obtaining informed consent. Approval for this study was obtained from the Local Research Ethics Committee (LREC). Based on the Binet classification, 9 patients had stage A; 7, stage B; and 10, stage C disease. Of the tumors, 15 showed no evidence of ATM or TP53 mutations, whereas 7 were ATM mutant and 4 had mutations within the TP53 gene.4,12 There were 12 tumors that exhibited unmutated immunoglobulin VH genes, thought to reflect aggressive disease, while the remaining 11 had mutated VH genes (Table 1).
Comparison among ATM/TP53 gene status, drug response, and clinical stage in 26 B-CLL tumors
B-CLL tumor . | ATM and TP53 status . | VH gene status . | Disease stage . | Response to fludarabine in vitro . |
|---|---|---|---|---|
| 9206TR | ATM wild type | N | A | Resistant* |
| 9348AA | ATM wild type | M | A | Resistant |
| 8375AE | ATM mutant | UM | C | Resistant |
| 9439MS | ATM mutant | UM | B | Resistant |
| 8944MK | ATM mutant | UM | B | Resistant |
| 9292TT | ATM mutant | UM | C | Resistant |
| 6692MM | TP53 mutant | M | C | Sensitive |
| 6032RB | TP53 mutant | UM | C | Sensitive |
| 5266BP | TP53 mutant | UM | C | Sensitive |
| 9283PA | TP53 mutant | M | A | Sensitive |
| MB | ATM mutant | UM | C | Sensitive |
| SS | ATM wild type | N | B | Sensitive |
| 8992JF | ATM wild type | M | A | Sensitive |
| 8998GN | ATM wild type | M | B | Sensitive |
| 9375JM | ATM wild type | M | B | Sensitive |
| 8815DH | ATM wild type | M | C | Sensitive |
| 9277BL | ATM mutant | UM | C | Sensitive |
| 9355EM | ATM wild type | M | C | Sensitive |
| 9264JM | ATM mutant | M | A | Sensitive |
| 9447TQ | ATM wild type | UM | A | Sensitive |
| 8955ML | ATM wild type | UM | A | Sensitive |
| 28SW | ATM wild type | UM | B | Sensitive |
| 102JK | ATM wild type | M | A | Sensitive |
| 111AL | ATM wild type | N | A | Sensitive |
| 119BS | ATM wild type | M | C | Sensitive |
| 9236PA | ATM wild type | UM | B | Sensitive |
B-CLL tumor . | ATM and TP53 status . | VH gene status . | Disease stage . | Response to fludarabine in vitro . |
|---|---|---|---|---|
| 9206TR | ATM wild type | N | A | Resistant* |
| 9348AA | ATM wild type | M | A | Resistant |
| 8375AE | ATM mutant | UM | C | Resistant |
| 9439MS | ATM mutant | UM | B | Resistant |
| 8944MK | ATM mutant | UM | B | Resistant |
| 9292TT | ATM mutant | UM | C | Resistant |
| 6692MM | TP53 mutant | M | C | Sensitive |
| 6032RB | TP53 mutant | UM | C | Sensitive |
| 5266BP | TP53 mutant | UM | C | Sensitive |
| 9283PA | TP53 mutant | M | A | Sensitive |
| MB | ATM mutant | UM | C | Sensitive |
| SS | ATM wild type | N | B | Sensitive |
| 8992JF | ATM wild type | M | A | Sensitive |
| 8998GN | ATM wild type | M | B | Sensitive |
| 9375JM | ATM wild type | M | B | Sensitive |
| 8815DH | ATM wild type | M | C | Sensitive |
| 9277BL | ATM mutant | UM | C | Sensitive |
| 9355EM | ATM wild type | M | C | Sensitive |
| 9264JM | ATM mutant | M | A | Sensitive |
| 9447TQ | ATM wild type | UM | A | Sensitive |
| 8955ML | ATM wild type | UM | A | Sensitive |
| 28SW | ATM wild type | UM | B | Sensitive |
| 102JK | ATM wild type | M | A | Sensitive |
| 111AL | ATM wild type | N | A | Sensitive |
| 119BS | ATM wild type | M | C | Sensitive |
| 9236PA | ATM wild type | UM | B | Sensitive |
The response to CYC20 in vitro was sensitive in all tumors.
N indicates not known; M, mutated; and UM, unmutated.
Less than 40% of cells apoptotic at 72 hours
Separation of B-CLL cells and normal lymphocytes
Mononuclear cells from B-CLL patients were separated by density centrifugation of whole blood4 and cultured in RPMI containing 1% bovine serum albumin (BSA; Sigma, Gillingham, United Kingdom) at a density of 1 × 106 cells/mL. Analysis of 9 representative B-CLL samples revealed 90% to 95% cells positive for CD5. In order to avoid any possible effect of positive selection on responses to the drugs, we enriched T cells from 3 healthy donors and B cells from 5 healthy donors by depletion of non–T and non–B-cell types, respectively, using RosetteSep B- or T-cell enrichment antibody cocktails (StemCell Technologies, London, United Kingdom). We obtained a minimum of 65% of cells positive for CD19 and minimum of 85% of cells positive for CD3.
Induction of apoptosis in vitro
Each tumor sample was divided into 2 aliquots, and 1 aliquot was irradiated with 5 grays (Gy) using a Precisa 217 with source-emitting gamma-type rays (Pantatron, Gosport, Hampshire, United Kingdom). The remaining cells were either left untreated or incubated with 20 μM fludarabine and/or with CYC202 at a concentration between 1 and 25 μg/mL for various lengths of time up to 72 hours. For wash-off experiments, cells were incubated in the presence of CYC202 for a variable period of time, washed, and replated, and cell viability was determined at 24, 48, and 72 hours. An annexin V apoptosis kit (BD Pharmingen, Oxford, United Kingdom) and a Coulter Epics XL-MCL flow cytometer (Beckman Coulter, Fullerton, CA) were used to measure viability and apoptosis in B-CLLs, and in control T and B lymphocytes treated with drugs. B-CLL tumors were considered sensitive if they exhibited more than 40% apoptotic cells after 72 hours of incubation with a drug. For each experiment, the mean proportion of apoptotic cells and viable cells was calculated, along with the 95% confidence interval for the mean. Differences between means were tested using the Student t test and one-way analysis of variance (ANOVA).
Western blotting
Cell lysates from B-CLL samples and T or B cells from different donors pooled together were incubated with CYC202 for various lengths of time and subjected to standard Western blotting procedures.4 Primary antibodies against myeloid cell leukemia-1 (Mcl-1) and xeroderma pigmentosum complementation group A (XPA) were purchased from BD Pharmingen; p21WAF, B-cell lymphoma-2 (Bcl-2), nuclear factor κB (NFκB), tumor necrosis factor receptor-associated factor 5 (TRAF5), poly(adenosine diphosphate–ribose) polymerase 1 (PARP1) n20, and proliferating cell nuclear antigen (PCNA), from Santa Cruz (Autogen Bioclear, Calne, United Kingdom); procaspases-3 and -7 and cleaved caspase-3, from Cell Signaling Technology (Beverly, MA); heat shock protein 70 (HSP70), from Calbiochem (La Jolla, CA); and actin, from Sigma-Aldrich (Dorset, United Kingdom). Sheep polyclonal antibody against p53 was donated by D. P. Lane (University of Dundee, United Kingdom); anti-RNA polymerase II (pol II) and anti-RNA pol II phospho-serine 2 were obtained from Covance Research Products (Cambridge Bioscience, Cambridge, United Kingdom). Immobilized antigens were detected using an enhanced chemiluminescence (ECL) detection system (Amersham Biosciences, Chalfont St Giles, United Kingdom), and protein levels were compared by densitometry.
Microarray analysis
Microarray analysis was performed on 5 B-CLL tumors (3 ATM mutant and 2 ATM wild type) before and 4 hours after incubation with 5 μg/mL CYC202. For microarray analysis, extraction of total RNA, first- and second-strand cDNA synthesis, in vitro transcription, and hybridization to U95Av2 GeneChips were performed as previously described.12
Expression values were obtained for all 10 hybridizations using Affymetrix Microarray Suite 5.0 software (Affymetrix, Santa Clara, CA). Data quality was assessed using MAS5.0 report files and GeneSpring 5.1 (Silicon Genetics, San Carlos, CA). For analysis with GeneSpring 5.1 software, raw data were exported from MAS5.0 and values were normalized to the median signal value for each array. For comparison on the basis of drug response, additional normalization was performed to the mean level of gene expression in the untreated samples. The U95Av2 GeneChip contains 12 627 transcripts, including control bacterial genes. Filtering of the data to produce a list of informative genes was performed as previously described.12 As an alternative method, scanned images of microarray chips were analyzed using probe level quantile normalization.13 Subsequently, robust multiarray analysis14 on the raw cell intensity files (CEL) was performed using the Affymetrix package of the Bioconductor (http://www.bioconductor.org) project. Differentially expressed probe sets were identified using significance analysis of microarrays (SAM).15,16 Finally, hierarchic clustering of genes was performed using dChip and default settings (http://www.dchip.org).
Results
CYC202 is a potent inducer of apoptosis in vitro in B-CLL tumors
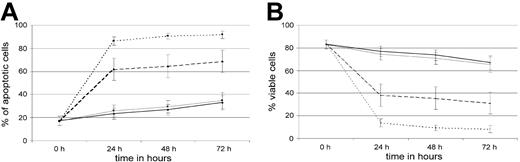
In order to establish conditions required for optimal killing, B-CLL cells were initially exposed to increasing doses of CYC202 for 4, 8, 16, 24, 48, and 72 hours and cellular viability and apoptosis assessed at each time point (Figure 1). Treatment with 1 μg/mL had little effect on induction of apoptosis and cell viability in any of the samples, whereas 2.5 μg/mL affected most but not all of the samples. In contrast, within 24 hours of the start of treatment with CYC202 at 5 μg/mL, there was a dramatic induction of apoptosis accompanied by loss of viability, and by 48 hours of treatment most B-CLL cells were undergoing apoptosis. Little dose-dependency was observed with concentrations higher than 5 μg/mL. We found that the first signs of apoptosis were detectable between 4 and 8 hours of treatment with 5 μg/mL CYC202, and the proportion of viable cells greatly diminished by 16 hours (data not shown).
To determine whether B-CLL cells treated with CYC202 for different times could escape the effects of the drug if left to recover in drug-free culture following CYC202 exposure, we performed wash-off experiments. We treated the cells of 3 B-CLL tumors with 5 μg/mL CYC202 for 30 minutes, and 1, 2, 3, 4, 6, and 8 hours, then washed off the drug and continued to incubate the cells before analyzing the induction of apoptosis at 24, 48, and 72 hours. Exposure to CYC202 for fewer than 6 hours with subsequent recovery in culture did not induce measurable cytotoxic effects, whereas with exposure times of 6 hours and more, a large increase in apoptosis was seen despite a recovery period after drug exposure (data not shown). These results are consistent with our detection of early apoptotic cells in B-CLL cultures treated for 8 hours and indicate that a minimum time of 6 to 8 hours of exposure to the drug is necessary to irreversibly engage the apoptotic machinery of the cell.
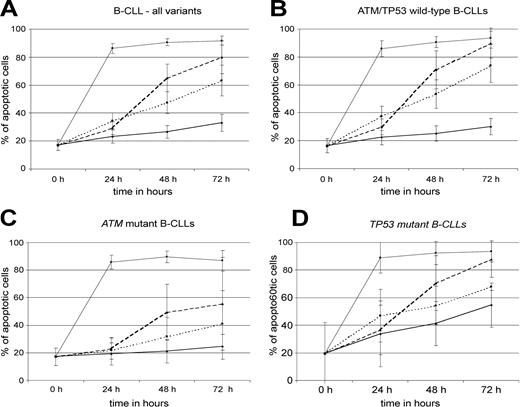
Subsequently, 26 B-CLL samples, including those with a range of ATM and TP53 mutations, were analyzed following incubation with CYC202 and the results compared with induction of apoptosis and killing of the same tumors by IR and fludarabine (Figure 2). Analysis of all 26 B-CLL samples at 24 hours revealed an average of 83.9% (95% CI, 78.6-89.2) apoptotic cells following treatment with 5 μg/mL CYC202 (Table 2; Figure 2A), while untreated B-CLL cells showed 23.3% (95% CI, 18.7-27.9) apoptotic cells at the same time point (P < .001). When tumors were divided by genotype, the 15 ATM/TP53 wild-type tumors showed 82.5% (95% CI, 73.5-91.5) apoptotic cells following incubation with CYC202 for 24 hours, and ATM mutant tumors and TP53 mutant tumors under the same conditions revealed 84.2% (95% CI, 77.4-91.0) and 88.6% (95% CI, 77.6-99.6) of cells in apoptosis, respectively (Table 2; Figure 2B-D). Indeed, CYC202-related apoptosis did not differ significantly between 3 genetic B-CLL variants at any time point (P = .735, P = .550, and P = .052 at 24, 48, and 72 hours, respectively). Thus, none of the 3 genotypes was resistant to induction of apoptosis by CYC202 in vitro.
Effect of CYC202 (5 μg/mL), fludarabine (20 μM), or irradiation (5 Gy) on apoptosis in 26 B-CLL tumors
. | . | % apoptotic cells, mean (95% CI) . | . | . | . | |||
|---|---|---|---|---|---|---|---|---|
| Genotype . | No. . | No drug . | CYC202 . | Fludarabine . | Irradiation . | |||
| After 24 hours | ||||||||
| All types | 26 | 23.3 (18.7-27.9) | 83.9 (78.6-89.2) | 28.7* (24.3-33.1) | 33.5* (27.6-39.3) | |||
| ATM/TP53 wt | 15 | 22.5 (17.3-27.7) | 82.5 (73.5-91.5) | 29.3* (23.5-35.1) | 36.3* (29.1-43.5) | |||
| ATM mut | 7 | 19.0 (11.1-26.9) | 84.2 (77.4-91.0) | 22.9* (15.2-30.6) | 21.7* (12.9-30.5) | |||
| TP53 mut | 4 | 33.8 (9.9-57.7) | 88.6 (77.6-99.6) | 36.7† (18.5-54.9) | 46.8‡ (27.2-66.4) | |||
| After 48 hours | ||||||||
| All types | 26 | 25.8 (20.8-30.8) | 87.5 (83.1-91.9) | 64.2* (53.9-74.5) | 47.0* (39.2-54.8) | |||
| ATM/TP53 wt | 15 | 24.1 (18.2-30.0) | 87.6 (80.9-94.3) | 69.0‡ (54.8-83.2) | 52.8* (42.7-63.0) | |||
| ATM mut | 7 | 20.7 (12.2-29.2) | 84.5 (75.4-93.6) | 48.4† (28.2-68.6) | 31.4* (17.7-45.2) | |||
| TP53 mut | 4 | 41.3 (25.2-57.4) | 92.3 (83.8-100) | 73.6 (47.8-99.4) | 54.3‡ (40.2-68.3) | |||
| After 72 hours | ||||||||
| All types | 22 | 31.7 (25.3-38.1) | 89.3 (84.0-94.6) | 79.0 (67.1-90.8) | 62.2* (51.1-73.3) | |||
| ATM/TP53 wt | 12 | 28.8 (22.8-34.9) | 92.8 (88.1-97.5) | 89.1 (78.2-99.9) | 73.4‡ (61.2-85.6) | |||
| ATM mut | 6 | 22.4 (14.4-30.4) | 79.7 (62.3-97.1) | 53.9 (20.3-87.6) | 39.0‡ (16.1-61.9) | |||
| TP53 mut | 4 | 54.4 (38.5-70.4) | 93.4 (85.8-100) | 87.6 (74.5-100) | 67.5‡ (64.9-70.0) | |||
. | . | % apoptotic cells, mean (95% CI) . | . | . | . | |||
|---|---|---|---|---|---|---|---|---|
| Genotype . | No. . | No drug . | CYC202 . | Fludarabine . | Irradiation . | |||
| After 24 hours | ||||||||
| All types | 26 | 23.3 (18.7-27.9) | 83.9 (78.6-89.2) | 28.7* (24.3-33.1) | 33.5* (27.6-39.3) | |||
| ATM/TP53 wt | 15 | 22.5 (17.3-27.7) | 82.5 (73.5-91.5) | 29.3* (23.5-35.1) | 36.3* (29.1-43.5) | |||
| ATM mut | 7 | 19.0 (11.1-26.9) | 84.2 (77.4-91.0) | 22.9* (15.2-30.6) | 21.7* (12.9-30.5) | |||
| TP53 mut | 4 | 33.8 (9.9-57.7) | 88.6 (77.6-99.6) | 36.7† (18.5-54.9) | 46.8‡ (27.2-66.4) | |||
| After 48 hours | ||||||||
| All types | 26 | 25.8 (20.8-30.8) | 87.5 (83.1-91.9) | 64.2* (53.9-74.5) | 47.0* (39.2-54.8) | |||
| ATM/TP53 wt | 15 | 24.1 (18.2-30.0) | 87.6 (80.9-94.3) | 69.0‡ (54.8-83.2) | 52.8* (42.7-63.0) | |||
| ATM mut | 7 | 20.7 (12.2-29.2) | 84.5 (75.4-93.6) | 48.4† (28.2-68.6) | 31.4* (17.7-45.2) | |||
| TP53 mut | 4 | 41.3 (25.2-57.4) | 92.3 (83.8-100) | 73.6 (47.8-99.4) | 54.3‡ (40.2-68.3) | |||
| After 72 hours | ||||||||
| All types | 22 | 31.7 (25.3-38.1) | 89.3 (84.0-94.6) | 79.0 (67.1-90.8) | 62.2* (51.1-73.3) | |||
| ATM/TP53 wt | 12 | 28.8 (22.8-34.9) | 92.8 (88.1-97.5) | 89.1 (78.2-99.9) | 73.4‡ (61.2-85.6) | |||
| ATM mut | 6 | 22.4 (14.4-30.4) | 79.7 (62.3-97.1) | 53.9 (20.3-87.6) | 39.0‡ (16.1-61.9) | |||
| TP53 mut | 4 | 54.4 (38.5-70.4) | 93.4 (85.8-100) | 87.6 (74.5-100) | 67.5‡ (64.9-70.0) | |||
wt indicates wild type; mut, mutant.
Footnote symbols in “Fludarabine” and “Irradiation” indicate results of comparisons with CYC202 at each time point; no symbol indicates no significant difference.
P < .001
P < .01
P < .05
Effect of CYC202 dose on apoptosis and survival of B-CLL cells in vitro. Dose response of B-CLL tumor cells to CYC202 shown by annexin V assay. Percentage of (A) apoptotic and (B) viable cells following 0, 24, 48, and 72 hours of treatment. ♦ and bold solid line indicate no drug (n = 26); ▪ and thin solid line, 1 μg/mL (n = 24); ▴ and dashed line, 2.5 μg/mL (n = 19); and • and dotted line, 5 μg/mL (n = 26) CYC202. Graphs represent mean proportion of apoptotic cells at each time point, and error bars represent 95% confidence intervals.
Effect of CYC202 dose on apoptosis and survival of B-CLL cells in vitro. Dose response of B-CLL tumor cells to CYC202 shown by annexin V assay. Percentage of (A) apoptotic and (B) viable cells following 0, 24, 48, and 72 hours of treatment. ♦ and bold solid line indicate no drug (n = 26); ▪ and thin solid line, 1 μg/mL (n = 24); ▴ and dashed line, 2.5 μg/mL (n = 19); and • and dotted line, 5 μg/mL (n = 26) CYC202. Graphs represent mean proportion of apoptotic cells at each time point, and error bars represent 95% confidence intervals.
Effect of different treatments on apoptosis and survival of B-CLL cells in vitro. Response of B-CLL tumor cells to different treatments shown by annexin V assay at 0, 24, 48, and 72 hours. Cells received no treatment (♦ and bold solid line), 5 Gy gamma ionizing radiation (• and dotted line), 20 μM fludarabine (▴ and dashed line), or 5 μg/mL CYC202 (▪ and thin solid line). Percentage of apoptotic cells in (A) all samples (n = 26), (B) ATM/TP53 wild-type B-CLLs (n = 15), (C) ATM mutant B-CLLs (n = 7), and (D) TP53 mutant B-CLLs (n = 4). Graphs represent mean proportion of apoptotic cells at each time point, and error bars represent 95% confidence intervals.
Effect of different treatments on apoptosis and survival of B-CLL cells in vitro. Response of B-CLL tumor cells to different treatments shown by annexin V assay at 0, 24, 48, and 72 hours. Cells received no treatment (♦ and bold solid line), 5 Gy gamma ionizing radiation (• and dotted line), 20 μM fludarabine (▴ and dashed line), or 5 μg/mL CYC202 (▪ and thin solid line). Percentage of apoptotic cells in (A) all samples (n = 26), (B) ATM/TP53 wild-type B-CLLs (n = 15), (C) ATM mutant B-CLLs (n = 7), and (D) TP53 mutant B-CLLs (n = 4). Graphs represent mean proportion of apoptotic cells at each time point, and error bars represent 95% confidence intervals.
Compared with CYC202 treatment, cells treated with 20 μM fludarabine showed a delayed induction of apoptosis in B-CLL cells (Figure 2A; Table 2). Little apoptosis and loss of viability above background was observed within the first 24 hours of treatment by fludarabine in all 3 genetic subtypes (Figure 2B-D; Table 2). Consequently, the level of fludarabine-induced apoptosis at 24 hours was significantly lower compared with the CYC202-induced apoptosis. We observed that irrespective of genotype in the group of 26 B-CLL tumors, 28.7% of B-CLL cells (95% CI, 24.3-33.1) had undergone apoptosis after 24 hours of treatment with fludarabine, compared with 83.9% of cells following treatment with CYC202 (95% CI, 78.6-89.2) (P < .001). At 48 hours, the induction of apoptosis in fludarabine-treated cells remained significantly lower than with CYC202 (64.2% vs 87.5%, P = .001) (Table 2), whereas at 72 hours the difference was no longer significant (79.0% vs 89.3, P = .001). Interestingly, 6 of 26 B-CLL tumors showed a poor response to fludarabine in vitro, with less than 40% of apoptotic cells at 72 hours (Table 1). Of these, 4 had mutations within the ATM gene. Indeed, when the 3 genetic B-CLL phenotypes were compared for their response to fludarabine it emerged that at 72 hours, fludarabine-induced apoptosis was significantly lower in ATM mutant tumors than in the wild-type B-CLLs (53.9% vs 89.1%; P = .016). TP53 mutant and wild-type tumors showed no differences in the levels of fludarabine-induced apoptosis at the same time point (87.6% vs 89.1%; P = .992).
In contrast to the effects of CYC202, and similar to fludarabine, B-CLL cells showed a modest induction of apoptosis 24 hours following IR in all 3 genetic subtypes. IR-induced apoptosis became prominent only 48 to 72 hours following exposure to IR (Table 2). Irrespective of genotype, in the group of 26 B-CLL tumors IR induced significantly less apoptosis than incubation with CYC202 (Figure 2) at 24 hours (33.5% vs 83.9%, P < .001), 48 hours (47.0% vs 87.5%, P < .001), and 72 hours (62.2% vs 89.3, P = .001). Again, IR apoptosis was significantly lower in ATM mutant B-CLLs than in the wild-type tumors at all 3 time points (21.7% vs 36.3% at 24 hours [P = .048]; 31.4% vs 52.8% at 48 hours [P = .038]; and 39% vs 73.4% at 72 hours [P = .008]).
Taken together, our data suggested that CYC202 was able to induce high levels of apoptosis and killing in all B-CLL samples, including those shown to be defective in irradiation and fludarabine-induced apoptosis. Over the time course studied, CYC202 was capable of inducing apoptosis and killing B-CLL cells in vitro more rapidly than fludarabine, regardless of ATM/TP53 gene status.
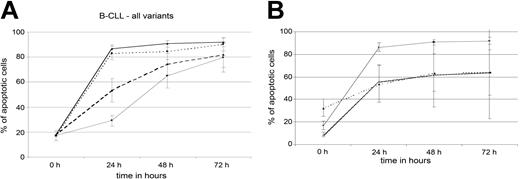
To study the potential synergism of the 3 treatment modalities on induction of apoptosis, 21 tumors were subjected to combined treatments involving IR plus fludarabine, IR plus CYC202, and fludarabine plus CYC202. Consistent with the lack of complete overlap in the mechanisms of killing by fludarabine and ionizing radiation, increased response rates upon irradiation were observed in 18 of 21 tumors treated with fludarabine over a 24-hour time period (Figure 3A). In contrast, neither irradiation nor fludarabine enhanced the apoptosis induced by CYC202 treatment (not shown), indicating the potent activity of CYC202 as a single agent. Given the rapid and robust induction of apoptosis by CYC202, it is likely that the effects of fludarabine and IR were masked by the much greater cytotoxicity of CYC202, especially at earlier time points.
Effect of CYC202 on induction of apoptosis in normal B and T lymphocytes
Roscovotine was shown to exhibit a differential induction of apoptosis between B-CLL and normal peripheral mononuclear cells.11 To determine the effects of CYC202 treatment on separate populations of normal B and T lymphocytes, B cells from 5 control individuals and T cells from 3 control individuals were isolated and treated with the drug at a concentration range of 1 to 20 μg/mL. In contrast to the effects of CYC202 on B-CLL cells, normal B and T lymphocytes showed delayed and reduced toxicity in response to CYC202. Accordingly, after 24 hours of treatment with 5 μg/mL CYC202, levels of apoptosis had increased from 32.5% (95% CI, 24.9-40.1) to 53.8% (95% CI, 37.5-70.1) in B cells and from 9.1% to 55.7% (95% CI, 40.6-70.8) in T cells (Figure 3B). These results compare with a much higher induction of apoptosis of 83.9% (95% CI, 78.6-89.2) in B-CLL cells treated with the same dose of CYC202 for 24 hours (P < .001 compared with T cells; P < .001 compared with B cells) (Figure 3B). The cytotoxicity of CYC202 against normal B cells reached comparable levels with that observed among B-CLLs only when 20 μg/mL was used to treat the B cells (not shown). Therefore, our data indicate that at a concentration of 5 μg/mL CYC202 possesses a significant degree of selective cytotoxicity toward B-CLL cells.
Mechanism of B-CLL killing by CYC202
Effect of CYC202 on apoptotic pathways and effector caspases. Most therapeutic agents induce apoptosis by up-regulation of the p53 protein and its responsive genes, activation of effector procaspases, and cleavage of substrates such as PARP1.5,17 To elucidate the common mechanism of killing by CYC202 between wild-type, ATM mutant, and TP53 mutant B-CLLs, we first examined the activation of the p53 pathway and downstream effector caspases in B-CLL cells of these 3 genetic subtypes following incubation with CYC202. Interestingly, although Western blotting revealed a discrete increase in the levels of p53 protein over the period of 24 hours of treatment with CYC202 in ATM/TP53 wild-type tumors, there was no evidence of up-regulation of the p53-responsive protein p21 (Figure 4A). As expected, there was no sign of CYC202-induced up-regulation of p53, or p21WAF in tumors with either ATM or TP53 mutations. On the contrary, both types of mutant tumors displayed decreases in the levels of p53 protein over time that become barely detectable by 18 to 24 hours of incubation with CYC202 (Figure 4A). Consistent with induction of apoptosis, PARP1, a target for degradation by activated effector caspase-3, was cleaved by 4 to 24 hours of CYC202 treatment in representative tumors of all 3 B-CLL subtypes (Figure 4B). Furthermore, direct caspase-3 activation was confirmed in all 3 B-CLL subtypes by the cleavage of procaspase-3 and the concomitant appearance of active caspase-3. Cleavage and disappearance of procaspase-7 was also detected and indicated activation of caspase-7 (Figure 4B). We concluded that the mechanism of CYC202-induced killing includes activation of apoptosis independently of p53.
Additive effect of drugs and irradiation on apoptosis of B-CLL cells and CYC202-induced apoptosis in normal lymphocytes. (A) Apoptosis in B-CLL cells analyzed by annexin V assay at 0, 24, 48, and 72 hours of treatment with either 20 μM fludarabine (n = 25) or 5 μg/mL CYC202 (n = 21), with or without 5 Gy ionizing radiation (IR). ♦ and bold solid line indicate CYC202 alone; ▪ and thin solid line, fludarabine alone; ▴ and dashed line, fludarabine plus IR; and • and dotted line, CYC202 plus IR. (B) Effects of incubation with 5 μg/mL CYC202 on apoptosis of normal B cells (▴ and dotted line), normal T cells (♦ and bold solid line), and B-CLL cells (▪ and thin solid line). Graphs represent mean proportion of apoptotic cells at each time point, and error bars represent 95% confidence intervals.
Additive effect of drugs and irradiation on apoptosis of B-CLL cells and CYC202-induced apoptosis in normal lymphocytes. (A) Apoptosis in B-CLL cells analyzed by annexin V assay at 0, 24, 48, and 72 hours of treatment with either 20 μM fludarabine (n = 25) or 5 μg/mL CYC202 (n = 21), with or without 5 Gy ionizing radiation (IR). ♦ and bold solid line indicate CYC202 alone; ▪ and thin solid line, fludarabine alone; ▴ and dashed line, fludarabine plus IR; and • and dotted line, CYC202 plus IR. (B) Effects of incubation with 5 μg/mL CYC202 on apoptosis of normal B cells (▴ and dotted line), normal T cells (♦ and bold solid line), and B-CLL cells (▪ and thin solid line). Graphs represent mean proportion of apoptotic cells at each time point, and error bars represent 95% confidence intervals.
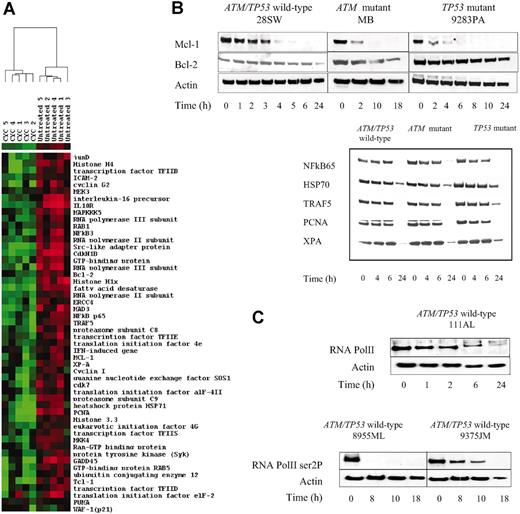
Effect of CYC202 on transcription. Given the efficient killing within 24 hours of incubation with CYC202, the absence of p53 activation on Western blotting, and the noncycling nature of B-CLL cells,2,4,12 it appeared that the mechanism of action of CYC202 in B-CLL might extend beyond cell cycle inhibition. We speculated that one of the possible mechanisms of CYC202-dependent killing could involve a selective down-regulation of transcription, as an inhibitory effect of CYC202 on transcription has been previously implicated.8 In order to test the impact of CYC202 on transcription in B-CLL cells, we undertook global gene expression profiling using U95Av2 Affymetrix microarray chips in 5 representative samples before and 4 hours after exposure to CYC202. Gene expression results for CYC202-treated samples were compared with baseline gene expression for corresponding untreated samples. Following filtration of uninformative genes and statistical testing, we identified 547 genes that were down-regulated by more than 1.5-fold and 135 genes that were up-regulated by more than 1.5-fold following exposure to CYC202. While the up-regulated genes coded for proteins involved in diverse cellular functions, the down-regulated genes pointed to possible proapoptotic activities of CYC202 in B-CLL. Firstly, a spectrum of genes involved in initiation of transcription and translation was clearly down-regulated after exposure to CYC202. These included TFIIB, TFIID, TFIIS, TFIIE beta, RNA polymerase II and III, and elongation initiation factors eiF-2 alpha, gamma, and eiF-4. We also found that genes involved in DNA repair (XPA, XPC, and ERCC4), as well as genes encoding histones 1, 3, and 4, were clearly down-regulated after exposure to CYC202 (Figure 5A). Genes with antiapoptotic properties involved in the support of cellular survival, such as MCL1, BCL2, TCL1, Mad3, and TRAF5; several members of the heat shock family; genes encoding adhesion molecules; components of the NFκB pathway; and the family of interferon cytokines and receptors were also down-regulated in response to CYC202. Furthermore, CYC202 decreased the expression of transcripts encoding proteasome subunits 8 and 9, genes regulating proteasome function (ubiquitin-conjugating enzyme 12), genes involved in nuclear transport (GTPase and GTP-binding proteins), as well as genes involved in cell cycle progression (CDK1 and CDK7). Finally, CYC202 also down-regulated the expression of kinases implicated in proliferative/antiapoptotic responses, including mitogen-activated protein (MAP) kinases (mitogen-activated protein kinase kinase 3 [MKK3] and MKK4 and MAP kinase kinase kinase 5 [MAPKKK5]) and their downstream effectors as well as the protein spleen tyrosine kinase (Syk, Figure 5A). The profile of CYC202 transcriptional responses was remarkably different from those that we have previously observed following exposure to ionizing radiation in the same set of B-CLL tumors.12 In contrast to IR-induced signals and consistent with the p53-independent nature of CYC202 transcriptional responses, CYC202 did not induce in ATM/TP53 wild-type tumors significant changes in the mRNA levels of p53-responsive genes such as p21WAF, PUMA (Figure 5A), Mdm2, and ferrodoxin reductase. In addition, down-regulation of prosurvival factors Mcl-1, genes encoding heat shock proteins, and NFκB appeared to be entirely specific to the CYC202 effect, as these genes were found to be up-regulated following IR in wild-type B-CLL tumors.12
Effect of CYC202 on protein expression in B-CLL. (A) Western blotting showing effects of incubation with 5 μg/mL CYC202 on the expression of p21WAF and p53 proteins in representative ATM/TP53 wild-type, ATM mutant, and TP53 mutant B-CLL cells. p53-actin ratio was determined by densitometry and is given above the Western blot. (B) Effect of the same treatment on the cleavage of PARP1, procaspase-3, and procaspase-7. Arrows indicate cleaved products of PARP1 and caspase-3. ATM/TP53 wild-type cells were treated with CYC202 for 0, 1, 2, 3, 4, 5, 6, and 24 hours; ATM mutant cells, for 0, 2, 10, and 18 hours; and TP53 mutant cells, for 0, 2, 4, 6, 8, 10, and 24 hours. Actin was used as a loading control.
Effect of CYC202 on protein expression in B-CLL. (A) Western blotting showing effects of incubation with 5 μg/mL CYC202 on the expression of p21WAF and p53 proteins in representative ATM/TP53 wild-type, ATM mutant, and TP53 mutant B-CLL cells. p53-actin ratio was determined by densitometry and is given above the Western blot. (B) Effect of the same treatment on the cleavage of PARP1, procaspase-3, and procaspase-7. Arrows indicate cleaved products of PARP1 and caspase-3. ATM/TP53 wild-type cells were treated with CYC202 for 0, 1, 2, 3, 4, 5, 6, and 24 hours; ATM mutant cells, for 0, 2, 10, and 18 hours; and TP53 mutant cells, for 0, 2, 4, 6, 8, 10, and 24 hours. Actin was used as a loading control.
We next used Western blotting to confirm the differential expression of key responders to CYC202 in representative ATM/TP53 wild-type, ATM mutant, and TP53 mutant tumors. Consistent with transcriptional changes, the levels of irradiation-inducible repair proteins PCNA and XPA were reduced by 24 hours of CYC202 treatment (Figure 5B). We then tested the expression of several antiapoptotic proteins, including Mcl-1, a prosurvival protein of the Bcl-2 family important for the regulation of apoptosis in lymphoid cells.18 We observed a rapid reduction in Mcl-1 protein levels as early as 2 hours of incubation for all tumor subtypes, followed by dramatic down-regulation and complete disappearance of the protein by 6 hours of CYC202 treatment (Figure 5B). The levels of prosurvival proteins Bcl-2 and HSP70, whose mRNA was also down-regulated in response to CYC202, remained largely unchanged within 24 hours of treatment. This is likely to reflect the differences in the half-lives of these proteins (0.5-3 hours for Mcl-1 vs 10-14 hours for Bcl-2).19 The levels of other prosurvival proteins, NFκB and TRAF 5, decreased at a slower rate. The control group of tumors treated with dimethyl sulfoxide (DMSO) showed no alterations in expression of the Mcl-1 protein, nor was cleavage of PARP1 observed (not shown), indicating that our culture conditions alone did not induce down-regulation of these proteins. Therefore, we confirmed that CYC202 induces down-regulation of various genes involved in DNA repair, transcription, and cellular survival.
Effect of CYC202 on transcription and protein levels. Microarray analysis showing changes in expression of 52 selected genes in 5 B-CLL tumors following treatment with 5 μg/mL CYC202 for 4 hours. The cluster was visualized using TREEVIEW (http://www.microarrays.org/software.html). Columns represent individual B-CLL samples and rows correspond to genes. Color changes within a row indicate expression levels relative to the average of the same population: red = up-regulation, green = down-regulation. (B) Western blotting showing differential reduction in expression of antiapoptotic proteins, Mcl-1, Bcl-2, NFκB, HSP70, and TRAF 5, as well as proteins involved in repair (PCNA and XPA), in representative tumors of all 3 B-CLL subtypes following treatment with CYC202 for up to 24 hours. (C) Effect of CYC202 on RNA pol II in B-CLL. Western blotting with a phospho-specific antibody to serine 2 of the carboxy-terminal domain of RNA pol II showing down-regulation of RNA pol II phosphorylation after CYC202 treatment with 5 μg/mL of 2 ATM/TP53 wild-type B-CLL tumors (bottom panel). Western blotting showing down-regulation of total RNA pol II protein levels by 24 hours of CYC202 treatment in a representative ATM/TP53 wild-type B-CLL tumor (top panel).
Effect of CYC202 on transcription and protein levels. Microarray analysis showing changes in expression of 52 selected genes in 5 B-CLL tumors following treatment with 5 μg/mL CYC202 for 4 hours. The cluster was visualized using TREEVIEW (http://www.microarrays.org/software.html). Columns represent individual B-CLL samples and rows correspond to genes. Color changes within a row indicate expression levels relative to the average of the same population: red = up-regulation, green = down-regulation. (B) Western blotting showing differential reduction in expression of antiapoptotic proteins, Mcl-1, Bcl-2, NFκB, HSP70, and TRAF 5, as well as proteins involved in repair (PCNA and XPA), in representative tumors of all 3 B-CLL subtypes following treatment with CYC202 for up to 24 hours. (C) Effect of CYC202 on RNA pol II in B-CLL. Western blotting with a phospho-specific antibody to serine 2 of the carboxy-terminal domain of RNA pol II showing down-regulation of RNA pol II phosphorylation after CYC202 treatment with 5 μg/mL of 2 ATM/TP53 wild-type B-CLL tumors (bottom panel). Western blotting showing down-regulation of total RNA pol II protein levels by 24 hours of CYC202 treatment in a representative ATM/TP53 wild-type B-CLL tumor (top panel).
To establish the mechanism by which CYC202 mediates down-regulation of transcription, we asked whether CYC202 affected not only the level but also the activation of RNA polymerase II. We analyzed the level of total RNA pol II protein as well as that of RNA pol II phosphorylated at serine 2 of the carboxy-terminal domain (CTD), an essential modification for the elongation phase of transcription.20 Notably, we found that not only were total protein levels lowered, but the levels of serine 2 phosphorylated protein were also significantly reduced in B-CLL tumor samples by 8 hours of CYC202 treatment (Figure 5C). Our results, therefore, indicate that in B-CLL cells CYC202-mediated down-regulation of transcription may involve a direct inhibition of the CDK9/cyclin T kinase that is responsible for phosphorylation and regulation of RNA pol II protein during the transition into productive elongation.20
Similar to B-CLL cells, in normal B and T lymphocytes down-regulation of RNA pol II serine 2 phosphorylation took place between 2 and 6 hours of incubation with CYC202 (Figure 6). However, unlike B-CLL cells, normal B and T cells exhibited an increase in the protein levels of NFκB, HSP70, and XPA within the first 24 hours of incubation with CYC202. Furthermore, prosurvival protein Mcl-1 was undetectable both before and after exposure to the drug in T cells and remained expressed at low levels in B cells. Consistent with delayed induction of apoptosis, cleaved caspase-3 was first detected in both B and T lymphocytes after 24 hours of incubation (Figure 6). We conclude that the kinetics of protein responses to CYC202 differ between normal and malignant lymphocytes.
Discussion
In this study, we have demonstrated that the novel CDK inhibitor CYC202 rapidly induces apoptosis in vitro in B-CLL tumor cells irrespective of the integrity of the p53 pathway by a mechanism that involves down-regulation of transcription and cell survival. We showed that induction of apoptosis by CYC202 in B-CLL is rapid, faster than apoptosis induced by fludarabine under the same conditions and also faster than induction of apoptosis previously reported for roscovitine.11
ATM/TP53 wild-type tumors, ATM mutant, and TP53 mutant B-CLLs responded equally to CYC202, and no single B-CLL tumor regardless of ATM/TP53 and VH status was resistant to CYC202. In contrast, we found that 6 tumors were resistant to fludarabine in vitro and 4 of those carried mutations in the ATM gene. Interestingly, all 4 TP53 mutant tumors in our study were sensitive to fludarabine. Although it is difficult to draw definitive conclusions from the observations made on a limited number of B-CLL tumors with a genetic defect in the p53 pathway, possible reasons for the differential response to fludarabine between ATM mutant and TP53 mutant tumors observed in our study might relate to the complexity of fludarabine-induced apoptosis. It has been reported that fludarabine induces p53 transcription,21 but activation of p53 might be only one aspect of fludarabine-induced apoptosis. Furthermore, although ATM and TP53 operate in the same DNA damage response pathway, their roles are not completely congruent12 and it is possible that some fludarabine-induced responses require ATM but not p53 function. Given its impact on the p53 transcription, it was recently suggested that early treatment with fludarabine might lead to the selection of resistant B-CLL subclones carrying mutations in the p53 pathway.21 In this respect, we show here that CYC202 has an entirely different mechanism of action in B-CLL and it does not induce ATM/p53-dependent transcription. It is unlikely, therefore, that treatment with CYC202 would select for subclones with mutations in the p53 pathway.
Effect of CYC202 on protein levels in normal T and B lymphocytes. Western blotting showing the levels of phosphorylated RNA pol II and proteins NFκB, HSP70, Mcl-1, XPA, cleaved caspases-3, and actin in pooled normal T and B lymphocytes following incubation with CYC202 for various lengths of time up to 24 hours.
Effect of CYC202 on protein levels in normal T and B lymphocytes. Western blotting showing the levels of phosphorylated RNA pol II and proteins NFκB, HSP70, Mcl-1, XPA, cleaved caspases-3, and actin in pooled normal T and B lymphocytes following incubation with CYC202 for various lengths of time up to 24 hours.
It has been reported previously that CYC202 demonstrates potent inhibitory activity against CDK2–cyclin E, a kinase required for the progression of cells from the G1 to the S phase of the cell cycle.9 However, the primarily noncycling nature of B-CLL cells was strongly suggestive of an additional mechanism of activity for this drug. In searching for this mechanism, we found that a large number of genes were down-regulated in response to the drug. Down-regulation of transcription has therefore emerged as a likely mechanism of B-CLL killing by CYC202. During transcription, positive elongation factor b (P-TEFb; CDK9/cyclin T1), transcription factor IIH (TFIIH; CDK7/cyclin H), and CDK8/cyclin C all phosphorylate the carboxy-terminal domain (CTD) of RNA polymerase II. However, only CDK9 is known to phosphorylate the CTD target residue serine 2, and this essential modification must occur before transcriptional elongation can proceed.22 It has been suggested that agents that inhibit the phosphorylation and activation of kinases CDK9 and CDK7 as well as the CTD of RNA pol II act as transcriptional repressors.23 Consistent with the role of CYC202 as a transcriptional repressor, we observed a rapid reduction in phosphorylation of serine 2 of RNA pol II in B-CLL cells treated with this drug, and found that this modification, together with down-regulation of transcription, preceded the induction of apoptosis in B-CLL tumor cells.
The most interesting aspect of CYC202 function is its ability to suppress multiple prosurvival mechanisms. We found that the reduction in protein levels of Bcl-2 family member Mcl-1 temporally preceded activation of caspases-3 and -7. Therefore, Mcl-1 down-regulation may be an initiating event in the induction of apoptosis by CYC202 in B-CLL cells as previously reported for other cell types.18,24-26 Although occurring later and at a lower rate, down-regulation of other prosurvival proteins such as NFκB family members and TRAF5 might also support cellular killing. Indeed, we previously observed that high levels of TRAF5 were associated with a defective DNA damage response in acute lymphoblastic leukemia (ALL) cells.27
Overall, the likely sequence of events following incubation of B-CLL cells with CYC202 would include: (a) inhibition of transcription by down-regulation of both RNA pol II phosphorylation and transcription-regulating genes, (b) disappearance of short-lived prosurvival proteins, and (c) activation of mitochondria and effector caspases.
Importantly, we found that CYC202 exhibits some selective cytotoxicity toward B-CLL cells. The precise mechanism of this selective cytotoxicity is not entirely clear. We observed different kinetics of key protein responders to CYC202 between B-CLLs and normal lymphocytes. In particular, baseline expression of Mcl-1 was higher in B-CLL cells than in normal B cells, and, consistent with a previous report,28 Mcl-1 was undetectable in untreated T cells. Interestingly, Mcl-1 levels remained unchanged in normal B lymphocytes during incubation with CYC202, despite clear evidence of apoptosis at 24 hours. Therefore, it is possible that down-regulation of RNA pol II serine 2 phosphorylation does not have the same dramatic effect on transcription in normal lymphocytes as it does in B-CLL cells. Alternately, the spectrum of genes down-regulated by CYC202 may differ between B-CLL cells and normal lymphocytes. It has been previously shown that in contrast to flavopiridol, roscovitine does not cause global down-regulation of gene transcription.29 Additional studies will be required to determine whether differences in global transcription between normal and malignant lymphocytes treated with CYC202 can further highlight the nature of differential cytotoxicity toward B-CLL cells. Given that apoptosis in B-CLL can be induced following a minimum of 6 hours of incubation with CYC202, it is possible to envisage that manipulation of the dose and interval between the administration of CYC202 in vivo could further differentiate the responses between B-CLL cells and normal lymphocytes. In support of this notion is the relatively low toxicity of CYC202 that has already been reported in a clinical setting.9,10
Although this study concerned the impact of CYC202 on transcription, it is possible that cell cycle inhibition, although not essential in noncycling B-CLL cells in the periphery, may be important in proliferative B-CLL centers in bone marrow and lymph nodes, in cell populations that were inaccessible in this study.
In summary, here we show that CYC202 is a potent inducer of apoptosis in B-CLL, including those with aggressive disease due to mutations in either the ATM or TP53 genes. No B-CLL tumors appeared to be resistant to CYC202 in vitro, and our data support its potential efficacy in leukemias that are refractory to the DNA-damaging agent fludarabine. Compared with fludarabine, CYC202 exhibits more rapid apoptotic response and does not activate the p53 pathway. In addition, CYC202 has a less prominent effect on normal lymphocytes. We believe, therefore, that CYC202 has a role in treatment for B-CLL patients with aggressive disease, and in this context a phase 2 clinical trial in refractory B-CLL is currently under way.
Prepublished online as Blood First Edition Paper, February 3, 2005; DOI 10.1182/blood-2004-07-2713.
Supported by Cancer Research UK and the Leukaemia Research Fund, UK.
The authors D.M., A.G.-B., and D.P.L. are employed by Cyclacel Ltd, whose potential product, CYC202, was studied in the present work and supplied to the authors at no cost.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 U.S.C. section 1734.
We would like to acknowledge Paul Biggs for isolating the B-CLL cells from patient samples and Dr Grant Stewart for help with protein extraction from normal B cells.



This feature is available to Subscribers Only
Sign In or Create an Account Close Modal