Comment on Hegde et al, page 496
Patients with aggressive non-Hodgkin lymphoma (NHL) are at risk for leptomeningeal disease. Hegde and colleagues shed light on who is at risk and how we detect occult disease.
Leptomeningeal disease from aggressive lymphoma is most often a fatal complication. Clinical paradigms exist to predict who will develop this complication, but they are inaccurate and not widely followed. Moreover, prophylactic intrathecal therapy for high-risk patients is cumbersome and invasive. Finally, the sensitivity of cytology is only between 40% to 80%,1,2 so many patients who already have leptomeningeal spread at diagnosis of systemic non-Hodgkin lymphoma (NHL) are missed and often only receive ineffective prophylactic dosing rather than treatment.
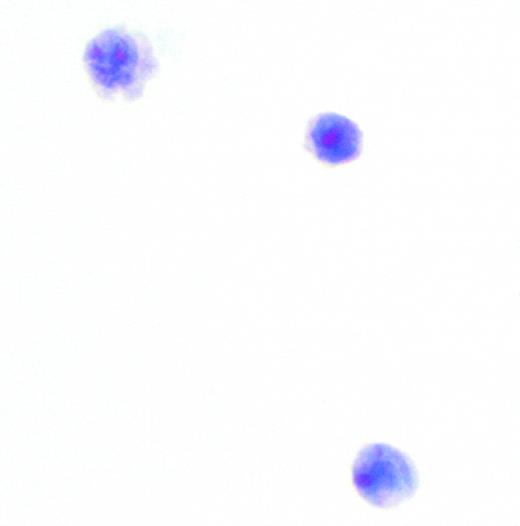
In this issue, Hegde and colleagues suggest that occult leptomeningeal disease at presentation and at relapse can be detected in high-risk patients using multicolor flow cytometry. In the newly diagnosed cohort, 11 of 51 (22%) of patients had a positive cerebrospinal fluid (CSF) by flow, yet only 1 was detected by routine cytology. The CSF fluid in these samples contained a median of only 0.002 × 109/L (2/μL) white blood cells (WBCs), and only 7% of the cells were characterized as malignant. Patients at high risk, but with negative cytology, received 12 prophylactic intrathecal therapies in addition to chemotherapy without blood-brain penetration, while the 10 with flow-positive occult disease and the 1 with a positive cytology received an intensive treatment beginning with therapy twice weekly and concluding with maintenance. In the 10 patients with follow-up at the National Institutes of Health (NIH), 7 received intrathecal via lumbar puncture and 3, via Ommaya reservoir.
Despite this very aggressive strategy, 5 (45%) relapsed in the central nervous system and died. In contrast, in patients at increased risk of central nervous system involvement, but with negative flow cytometry, the relapse risk was only 8% (3/40). Additionally, all 3 patients with relapsed systemic disease and positive CSF flow cytometry died.
This study demonstrates that flow cytometry is more sensitive than cytology in detecting occult leptomeningeal disease at diagnosis of systemic NHL with high-risk features. Importantly, Hegde et al demonstrate that 2 or more extranodal sites are the prime determinant in predicting occult or overt leptomeningeal disease, a factor commensurate with the biology of the disease. However, are these results widely applicable and should all patients deemed to be at risk have CSF sent for flow cytometry? It is certainly notable that 45% of the patients in this study had HIV, although only 64% of those with positive CSF fluid had HIV. Consequently, a prospective multi-institutional study in both HIV-positive and -negative individuals would prove that this approach can be generalized. It would also help answer the question as to whether aggressive intrathecal therapy can be more efficacious in those with flow-positive CSF if given via Ommaya or if agents with longer half-lives such as rituximab or liposomal cytarabine are used.FIG1 ▪

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal