Abstract
Indoleamine-2,3-dioxygenase (IDO) and tryptophanyl-tRNA-synthetase (TTS) are interferon-γ (IFN-γ)–inducible enzymes that are responsible for tryptophan degradation and for its use in protein synthesis, respectively. IFN-γ–induced IDO has immunomodulatory properties in murine and human models. A concomitant increase of TTS has been postulated to protect the IDO-expressing cells from tryptophan catabolism. IDO can be induced in dendritic cells (DCs) by recombinant soluble cytotoxic T lymphocyte antigen-4 (CTLA-4-Fc). We investigated the effects of CTLA-4-Fc on IDO and TTS mRNA expression in human peripheral blood mononuclear cells (PBMCs) and isolated leukocyte subsets. CTLA-4-Fc exposure induced increased IDO and TTS expression in unseparated PBMCs, as well as in monocyte-derived mature DCs. CD4+ T cells isolated from CTLA-4-Fc–treated PBMCs showed increased IDO and TTS compared with untreated cells. CD8+ T cells from CTLA-4-Fc–treated PBMCs expressed increased levels of TTS but not IDO. Pretreatment of PBMCs with CTLA-4-Fc inhibited the activation of CD4+ T cells induced by influenza A virus (Flu) or phytohemagglutinin A (PHA), but had no effect on CD8+ T cells. This is the first report of IDO and TTS regulation by the CTLA-4-B7 system in human CD4+ and CD8+ T cells, and raises the possibility that these 2 tryptophan-modulating enzymes provide an important mechanism for regulating immune responses.
Introduction
Indoleamine 2,3-dioxygenase (IDO) and tryptophanyl-tRNA-synthetase (TTS) are cytoplasmic enzymes involved in tryptophan (Trp) catabolism and use, respectively, and are both induced by interferon-γ (IFN-γ).1-8 IDO catalyzes the first step reaction of tryptophan catabolism, the conversion of tryptophan to N-formylkynurenine, and subsequently kynurenine.1-3 TTS is the ubiquitous enzyme responsible for the association of tryptophan with its specific tRNA, with the resulting Trp-tRNA complex used for protein synthesis.4-8 Therefore, IFN-γ exerts a dual effect on Trp metabolism by increasing the rate of degradation of Trp in the IDO pathway, and by enhancing the accumulation of this amino acid into Trp-tRNA complexes available for protein synthesis.
IDO is strongly expressed in macrophages and dendritic cells (DCs),9-12 and has been shown to be responsible for down-modulating T-cell activation and proliferation, through depletion of Trp from the microenvironment.9-15 Murine studies have also suggested that products of tryptophan catabolism (quinolinic acid and 3-hydroxyanthranilic acid) can induce apoptosis of T cells.16,17 In this context, regulation of TTS expression could serve as a mechanism for protecting IDO-expressing cells from Trp selfstarvation.18 The Trp-tRNA complex would provide a reservoir of the amino acid in a form that is protected from IDO-mediated degradation and directly available for the protein synthesis.18
Cytotoxic T lymphocyte antigen-4 (CTLA-4) is transiently expressed on T cells after activation, and can bind both B7.1 (CD80) and B7.2 (CD86) on antigen-presenting cells (APCs), with higher affinity than CD28.19-21 CTLA-4 is a negative regulator of T-cell activation, but the mechanisms underlying its inhibitory activity are still not fully understood.20-22 Competition with CD28 for binding to B7 molecules and induction of a direct inhibitory signal by CTLA-4 are among the suggested mechanisms.20-22 Recombinant soluble forms of CTLA-4 (CTLA-4-Fc) have been shown to induce IDO expression in murine23,24 and, more recently, human DCs.25 CTLA-4 bound B7 molecules on DCs and triggered IFN-γ production, resulting in the induction of IDO espression.23,24 Thus, CTLA-4 expressed on activated T cells can stimulate IDO in DCs, providing feedback control of T-cell activation itself.24
Defects in the immunoregulatory mechanism initiated by IDO have been suggested to be involved in (1) development of autoimmune conditions, such as multiple sclerosis and autoimmune diabetes26,27 ; (2) failure of immune surveillance of tumor cells28 ; (3) rejection of semiallogenic fetuses29-34 ; and (4) the dementia seen in some patients with acquired immunodeficiency syndrome (AIDS).35-39 Recent studies demonstrating the involvement of CTLA-4 in the control of autoimmune conditions40-44 and allograft rejection,44,45 as well as evidence that CTLA-4 blockade can enhance antitumor responses,46 also support the functional correlation between CTLA-4 and IDO.
In the present study, we used a recombinant soluble form of human CTLA-4 (CTLA-4-Fc) to determine whether its binding to B7 molecules would induce immunoregulatory gene transcription in human peripheral blood mononuclear cells (PBMCs). We found that IFN-γ and IDO as well as TTS are among the genes that are up-regulated by CTLA-4-Fc. We uniquely showed that CTLA-4–induced IDO and TTS expression occurred in CD4+ T cells as well as in DCs, and that treatment of human PBMCs with CTLA-4-Fc prevented CD4+ T-cell activation through an IDO-dependent mechanism.
Materials and methods
Isolation of PBMCs
PBMCs were isolated by density centrifugation (Ficoll-Hypaque; Pharmacia, Uppsala, Sweden) from citrate-anticoagulated peripheral blood obtained from healthy donors, under an NIH institutional review board (IRB)–approved protocol developed by the Department of Transfusion Medicine, NIH, Bethesda, MD. Cells were cultured in RPMI medium (Invitrogen, Gaithersburg, MD) with 10% fetal bovine serum (Sigma, St Louis, MO).
Purification of T and B cells
CD4+, CD8+, and CD19+ cells were purified from PBMCs by positive selection with anti-CD4, anti-CD8, or anti-CD19 beads (Miltenyi Biotech, Auburn, CA). The purity of CD4+, CD8+, and CD19+ cells after purification (determined by flow cytometry) was more than 97%, more than 98%, and more than 95%, respectively.
Generation of monocyte-derived DCs
Elutriated monocytes were provided by the Department of Transfusion Medicine, NIH. Immature DCs (iDCs) were generated from monocytes cultured in RPMI medium (Invitrogen, Gaithersburg, MD) with 10% fetal bovine serum (Sigma) in the presence of a combination of granulocytemacrophage colony-stimulating factor (GM-CSF), interleukin-4 (IL-4), and tumor necrosis factor α (TNF-α) (Immunex, Thousand Oaks, CA). Cultures were initiated with 20 ng/mL GM-CSF and 20 ng/mL IL-4. On the third day of culture, half of the medium was changed and 40 ng/mL GM-CSF was added. On the sixth day of culture, half of the medium was changed and 90 ng/mL GM-CSF and 40 ng/mL TNF-α were added. Mature DCs (mDCs) were generated by activation of iDCs by treatment with 50 ng/mL soluble CD40 ligand (CD40L; Immunex) for 24 hours.
Treatment of cells with CTLA-4-Fc, CD28-Fc, or recombinant human IFN-γ
Unseparated PBMCs, isolated CD4+, CD8+, and CD19+ cells, monocytes, and monocyte-derived iDCs and mDCs were cultured in RPMI medium (Invitrogen, Gaithersburg, MD) with 10% fetal bovine serum (Sigma) in the absence or presence of 4 μg/mL CTLA-4-Fc or 4 μg/mL CD28-Fc (R&D Systems, Minneapolis, MN). In some experiments, PBMCs were cultured with CTLA-4-Fc before leukocyte subset separation. In other experiments, cell fractionation was performed before culture with CTLA-4-Fc. Experiments with recombinant human interferon-γ (rhIFN-γ; Biogen, Cambridge, MA) were performed using a final concentration of 4 μg/mL rhIFN-γ. Incubation time varied depending on the analysis performed.
Blocking of B7.1, B7.2, and IFN-γ with specific monoclonal antibodies
Antihuman B7.1 (CD80) and/or antihuman B7.2 (CD86) (R&D Systems) monoclonal antibodies (mAbs) were added to PBMCs cultured in the absence or presence of CTLA-4-Fc. The final concentration was 5 μg/mL of one or each mAb. The same procedure was used for blocking with anti–IFN-γ mAb (R&D Systems), used at a final concentration of 5 μg/mL.
RNA extraction and reverse transcription
Total RNA was extracted from unseparated PBMCs; isolated CD4+, CD8+, and CD19+ cells; monocytes; and monocyte-derived iDCs and mDCs using the guanidium thiocyanate-phenol-chloroform method, modified for TRIzol (Invitrogen, Carlsbad, CA).
Real-time PCR
cDNA quantification for indoleamine 2,3 dioxygenase (IDO), interferon-γ (IFN-γ), TTS, and β-actin was obtained with a real-time polymerase chain reaction (PCR) technique. Real-time PCR was conducted with the ABI Prism 7900HT (Applied Biosystems, Foster City, CA). All reactions were performed using a SYBR green PCR mix (Qiagen, Valencia, CA), according to the following thermal profile: denaturation at 95°C for 15 seconds, annealing at 60°C for 15 seconds, and extension at 72°C for 15 seconds (data collection was performed during the extension step). The primer sequences were designed using the Primer Express Software v2.0 provided with the ABI Prism 7900HT (IDO forward, 5′-AGTCCGTGAGTTTGTCCTTTCAA-3′ and reverse, 5′-TTTCACACAGGCGTCATAAGCT-3′; IFN-γ forward, 5′-TCATCCAAGTGATGGCTGAACT-3′ and reverse 5′-CGAAACAGCATCTGACTCCTTGT-3′; TTS forward, 5′-GAAAGGCATTTTCGGCTTCA-3′ and reverse, 5′-CAGCCTGGATGGCAGGAA-3′; and β-actin forward, 5′-CTGGAACGGTGAAGGTGACA-3′ and reverse, 5′-CGGCCACATTGTGAACTTTG-3′). All reactions were performed in triplicate. Data analysis was performed with the SDS2.1 software, provided with the ABI Prism 7900HT. The threshold level was determined by the software according to the optimization of the baseline and the standard curve. Standards were obtained by amplification of a control sample in a PCR reaction, using the same primers, reagents, and conditions optimized for the real-time analysis. Arbitrary quantity values were assigned to the resulting standard and 4-fold serial dilutions were made to obtain an 8-point standard curve. Results are presented as ratios between the target gene mRNA and the β-actin mRNA.
Tryptophan and kynurenine concentration measurement by HPLC
Unseparated human PBMCs from 2 different donors were cultured in RPMI medium (Invitrogen, Gaithersburg, MD) with 10% fetal bovine serum (Sigma) under the following conditions: (1) untreated control; (2) CTLA-4-Fc (4 μg/mL); and (3) and rhIFN-γ (4 μg/mL). After 24 hours of culture, supernatants were collected for high-performance liquid chromatography (HPLC), and CD4+ T cells were isolated from PBMCs. CD4+ cells were then isolated from the untreated and the CTLA-4-Fc–treated PBMCs, and cultured, respectively, in the absence and presence of CTLA-4-Fc (4 μg/mL). After 24 hours of culture, supernatants were collected for HPLC. Detection of tryptophan and kynurenine was performed by HPLC as previously described.47
CD4+ and CD8+ T-cell activation assay
Unseparated human PBMCs from 3 different donors were cultured in 24-well plates (106 cells/well) in RPMI medium (Invitrogen, Gaithersburg, MD) with 10% fetal bovine serum (Sigma) in the absence or presence of CTLA-4-Fc (4 μg/mL) for 48 hours. Control experiments were performed with a combination of anti-B7.1 and anti-B7.2 mAbs (5 μg/mL). After 48 hours of culture, T-cell activation was obtained by addition of phytohemagglutinin A (PHA) at a final concentration of 1 μg/mL, or of infectious influenza A virus (Flu; hemagglutinin A titer of 1:8192) at a 1:400 dilution to the culture wells. Experiments with PHA activation were also performed with preincubation with 1 mM 1-methyl-tryptophan (1-MT), an IDO inhibitor, to test whether the CTLA-4-Fc effect on T-cell activation involved tryptophan catabolism. Cells were prepared for cytofluorimetric analysis 24 hours after Flu or PHA treatment. Supernatants from the PBMC cultures were collected for measurement of interleukin-2 (IL-2) production by enzyme-linked immunosorbent assay (ELISA).
Membrane CD4, CD8, CD69, and CD38 detection by flow cytometry
The cells were washed twice in phosphate-buffered saline (PBS). Membrane antigen expression was determined by incubating cells for 20 minutes at room temperature with allophycocyanin-conjugated mouse immunoglobulin G (IgG1) antihuman CD4 monoclonal antibody (mAb), cyanin 5.5–conjugated mouse IgG1 antihuman CD8 mAb, phycoerythrin-conjugated mouse IgG1 antihuman CD38 mAb, fluorescein isothiocyanate–conjugated mouse IgG1 antihuman CD69 mAb (Becton Dickinson, Franklin Lakes, NJ), or with control isotype-matched antibodies (at 5 μg/mL each) in PBS containing 2% mouse serum (Sigma). Cells were acquired on FACSCalibur flow cytometer (Becton Dickinson), using CellQuest software (Becton Dickinson). Samples were gated on viable cells by forward and side light scatter, and a minimum of 50 000 live cell events was acquired for each sample. Acquired data were analyzed using CellQuest software (Becton Dickinson).
Analysis of IL-2 production by ELISA
IL-2 production was measured in supernatants from cell cultures using the commercial IL-2 ELISA kit (R&D Systems), according to the manufacturer's instructions
Statistical analysis
Intrasample difference between treated and untreated cells was assessed using a paired Student t test. All results are shown as mean values ± SEM
Results
Monocyte-derived mDCs increase IDO and TTS expression after CTLA-4-Fc treatment
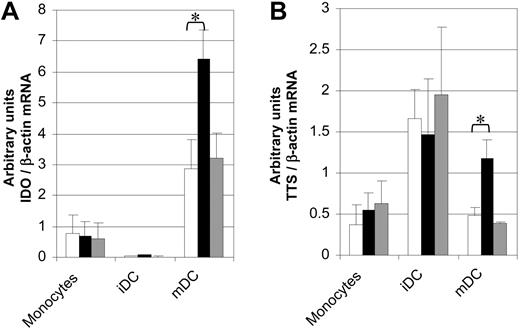
We tested the effect of CTLA-4-Fc exposure on elutriated monocytes and monocyte-derived DCs by analyzing IDO and TTS mRNA expression in the absence or presence of CTLA-4-Fc or CD28-Fc. The results showed that (1) mature DCs (mDCs) expressed higher baseline level of IDO mRNA compared with monocytes and immature DCs (iDCs) (Figure 1A); (2) in the presence of CTLA-4-Fc, only mDCs showed an increase in IDO expression (Figure 1A); (3) the TTS mRNA level was increased in mDCs exposed to CTLA-4-Fc compared with untreated mDCs (Figure 1B); (4) no change of TTS mRNA expression was induced by CTLA-4-Fc in monocytes (Figure 1B); (5) iDCs exhibited a relatively high basal level of TTS, which was not increased by CTLA-4-Fc (Figure 1B); and (6) IDO and TTS expression in monocytes, iDCs, and mDCs were not affected by CD28-Fc treatment. Thus, only mDCs exhibited CTLA-4-Fc–induced increases in IDO and TTS mRNA expression.
IDO and TTS mRNA expression and effect of CTLA-4-Fc and CD28-Fc in monocytes and DCs. (A) IDO mRNA expression in monocytes and monocyte-derived iDCs and mDCs after 12 hours of culture in the absence or presence of CTLA-4-Fc or CD28-Fc. (B) TTS mRNA expression in monocytes and monocyte-derived iDCs and mDCs after 12 hours of culture in the absence or presence of CTLA-4-Fc or CD28-Fc. □ represents media alone; ▪, CTLA-4-Fc; ▦, CD28-Fc. *P values less than .05 are based on 5 independent experiments. Mean values plus standard errors are shown.
IDO and TTS mRNA expression and effect of CTLA-4-Fc and CD28-Fc in monocytes and DCs. (A) IDO mRNA expression in monocytes and monocyte-derived iDCs and mDCs after 12 hours of culture in the absence or presence of CTLA-4-Fc or CD28-Fc. (B) TTS mRNA expression in monocytes and monocyte-derived iDCs and mDCs after 12 hours of culture in the absence or presence of CTLA-4-Fc or CD28-Fc. □ represents media alone; ▪, CTLA-4-Fc; ▦, CD28-Fc. *P values less than .05 are based on 5 independent experiments. Mean values plus standard errors are shown.
IDO and IFN-γ mRNA expression in human PBMCs are increased by treatment with CTLA-4-Fc
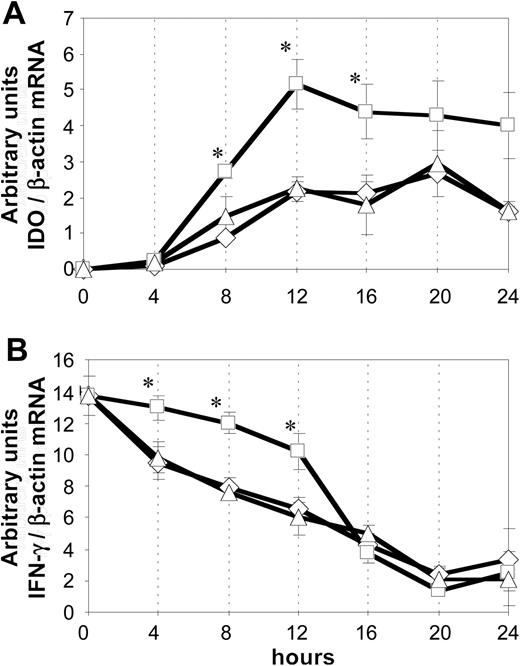
Unseparated human PBMCs were cultured for 24 hours in the absence or presence of CTLA-4-Fc or CD28-Fc (4 μg/mL). IDO and IFN-γ mRNA expression were analyzed at 4-hour intervals by quantitative real-time PCR. The results, shown in Figure 2, indicate that (1) CTLA-4-Fc induced a significant increase in IDO mRNA expression after 8, 12, and 16 hours compared with untreated cells (P = .022, P = .001, P = .002, respectively); (2) IDO mRNA expression increased during the first 12 hours of treatment (P values: 4 hours vs 8 hours = .002; 8 hours vs 12 hours = .009); (3) IFN-γ mRNA expression was higher in CTLA-4-Fc–treated PBMCs than in the untreated cells at 4, 8, and 12 hours (P = .012, P = .001, and P = .003, respectively); and (4) treatment with CD28-Fc did not affect IDO or IFN-γ mRNA expression. Thus, both IDO (Figure 2A) and IFN-γ (Figure 2B) mRNA were increased by CTLA-4-Fc but not CD28-Fc.
Kinetics of IDO and IFN-γ mRNA expression by human PBMCs after CTLA-4-Fc and CD28-Fc treatment. IDO (A) and IFN-γ (B) mRNA expression were analyzed using real-time PCR on untreated PBMCs (▵) and PBMCs treated with CTLA-4-Fc (□) or CD28-Fc (⋄). *P values less than .05 are based on 5 independent experiments. Mean values plus standard errors are shown.
Kinetics of IDO and IFN-γ mRNA expression by human PBMCs after CTLA-4-Fc and CD28-Fc treatment. IDO (A) and IFN-γ (B) mRNA expression were analyzed using real-time PCR on untreated PBMCs (▵) and PBMCs treated with CTLA-4-Fc (□) or CD28-Fc (⋄). *P values less than .05 are based on 5 independent experiments. Mean values plus standard errors are shown.
CTLA-4-Fc effects on PBMCs are dependent on binding to B7.1 and B7.2
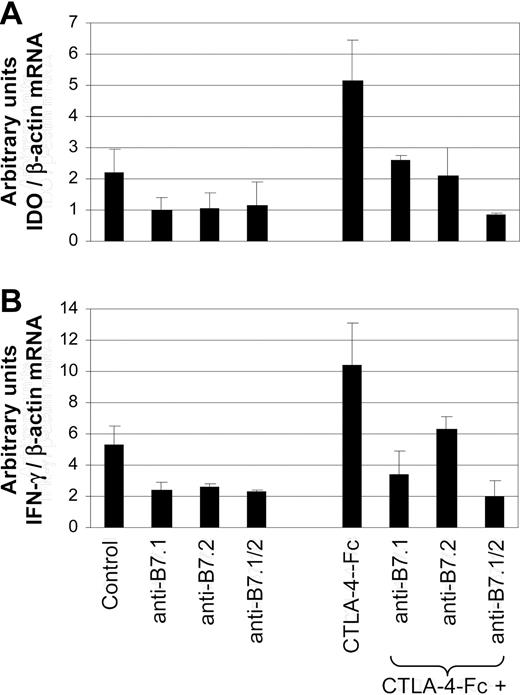
Because the costimulatory molecules B7.1 and B7.2 are the natural ligands for CTLA-4, we investigated whether the effect of CTLA-4-Fc on IDO and IFN-γ expression was dependent on its binding to these costimulatory molecules. Unseparated human PBMCs were cultured in the absence or presence of CTLA-4-Fc (4 μg/mL). Monoclonal antibodies specific for B7.1 and/or B7.2 were added to both untreated and CTLA-4-Fc–treated cells (5 μg/mL each). IDO and IFN-γ mRNA expression were analyzed after 12 hours by quantitative real-time PCR. The results indicated that incubation with anti-B7.1 and/or anti-B7.2 antibodies inhibited the overexpression of both IDO (Figure 3A) and IFN-γ (Figure 3B) induced by CTLA-4-Fc (P < .05). Furthermore, incubation with anti-B7.1 and/or anti-B7.2 mAb, even in the absence of CTLA-4-Fc, significantly reduced both IDO and IFN-γ mRNA expression compared with untreated PBMCs (P < .05).
Blocking the effect of CTLA-4-Fc on human PBMCs by anti-B7 mAb. IDO (A) and IFN-γ (B) mRNA expression in human PBMCs after 12-hour incubation with CTLA-4-Fc or mAb anti-B7.1, anti-B7.2, or both anti-B7.1 and anti-B7.2. The last 3 bars on the right of each panel represent simultaneous treatment of PBMCs with CTLA-4-Fc and mAb anti-B7.1 and/or anti-B7.2. P values, indicated in the text, are based on 10 independent experiments. Mean values plus standard errors are shown.
Blocking the effect of CTLA-4-Fc on human PBMCs by anti-B7 mAb. IDO (A) and IFN-γ (B) mRNA expression in human PBMCs after 12-hour incubation with CTLA-4-Fc or mAb anti-B7.1, anti-B7.2, or both anti-B7.1 and anti-B7.2. The last 3 bars on the right of each panel represent simultaneous treatment of PBMCs with CTLA-4-Fc and mAb anti-B7.1 and/or anti-B7.2. P values, indicated in the text, are based on 10 independent experiments. Mean values plus standard errors are shown.
IDO and tryptophanyl-tRNA-synthetase overexpression in human PBMCs is dependent on IFN-γ
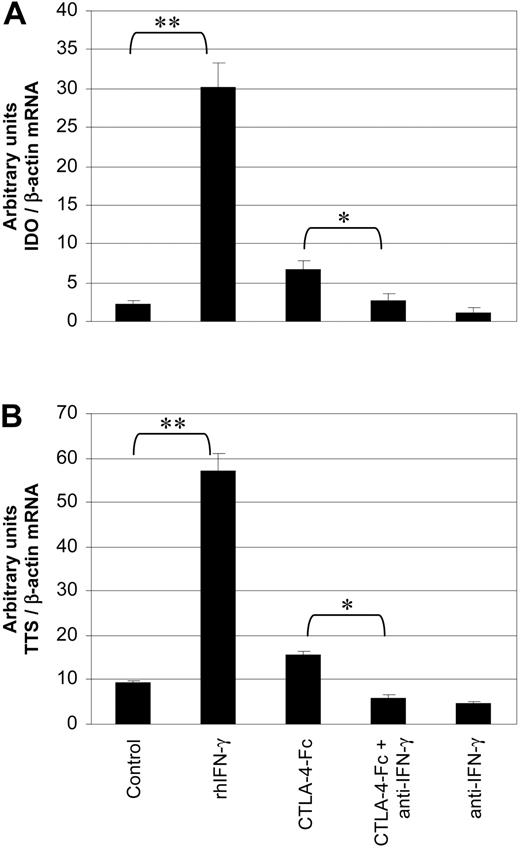
Unseparated PBMCs were cultured under the following conditions: (1) untreated control; (2) rhIFN-γ (4 μg/mL); (3) CTLA-4-Fc (4 μg/mL); (4) CTLA-4-Fc (4 μg/mL) plus anti–IFN-γ mAb (5 μg/mL); and (5) anti–IFN-γ mAb (5 μg/mL). IDO and TTS mRNA expression were analyzed after 12 hours by real-time PCR. Treatment with rhIFN-γ induced a 10-fold increase of IDO (Figure 4A) and a 6-fold increase of TTS (Figure 4B) mRNA expression (P < .005, for both IDO and TTS). The addition of anti–IFN-γ mAb significantly inhibited the CTLA-4-Fc–induced increase of IDO and TTS mRNA expression (P = .015 and P = .018, respectively). These results demonstrate that (1) CTLA-4-Fc and rhIFN-γ increase both IDO and TTS expression; (2) rhIFN-γ is more effective than CTLA-4-Fc for inducing IDO and TTS mRNA; and (3) CTLA-4-Fc–induced IDO and TTS expression are both IFN-γ dependent.
IDO and TTS expression and up-regulation in human PBMCs are dependent on IFN-γ. IDO (A) and TTS (B) mRNA expression in human PBMCs after 12 hours of culture under different conditions: (1) untreated control; (2) rhIFN-γ; (3) CTLA-4-Fc; (4) CTLA-4-Fc plus anti–IFN-γ mAb; and (5) anti–IFN-γ mAb. *P values less than .05 and **P values less than .005 are based on 4 independent experiments. Mean values plus standard errors are shown.
IDO and TTS expression and up-regulation in human PBMCs are dependent on IFN-γ. IDO (A) and TTS (B) mRNA expression in human PBMCs after 12 hours of culture under different conditions: (1) untreated control; (2) rhIFN-γ; (3) CTLA-4-Fc; (4) CTLA-4-Fc plus anti–IFN-γ mAb; and (5) anti–IFN-γ mAb. *P values less than .05 and **P values less than .005 are based on 4 independent experiments. Mean values plus standard errors are shown.
CD4+ T cells express IDO mRNA and respond to CTLA-4-Fc only when cultured as unseparated PBMCs
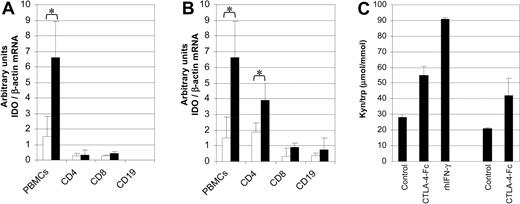
To determine which cells among PBMCs are responsible for IDO expression and up-regulation, and whether culture of isolated leukocytes with CTLA-4-Fc would result in IDO gene expression, we cultured unseparated PBMCs as well as isolated CD4+ (enriched for CD4+ T lymphocytes), CD8+ (enriched for CD8+ T lymphocytes), and CD19+ (enriched for B lymphocytes) cells in the absence or presence of CTLA-4-Fc. IDO mRNA expression was analyzed after 12 hours by quantitative real-time PCR. Whereas unseparated PBMCs responded to CTLA-4-Fc by enhancing IDO mRNA expression, CD4+ T cells, CD8+ T cells, and B cells did not express appreciable levels of IDO mRNA when cultured in the absence or presence of CTLA-4-Fc (Figure 5A). To test the role of cell-cell interaction in IDO expression and CTLA-4-Fc responsiveness of different cell types, we cultured unseparated PBMCs in the absence or presence of CTLA-4-Fc. These PBMCs were then separated into CD4+ T cells, CD8+ T cells, and B cells, and were tested separately for IDO mRNA expression. The results, shown in Figure 5B, indicate that CD4+ T cells showed baseline IDO levels comparable with unseparated PBMCs. Exposure of PBMCs to CTLA-4-Fc induced a 2-fold increase of IDO mRNA expression in CD4+ T cells. CD8+ T cells and B cells expressed low basal IDO levels and did not respond to CTLA-4-Fc by increasing IDO mRNA expression. The results of these experiments suggest that CTLA-4-Fc–induced expression of IDO by CD4+ T cells requires accessory function provided by one or more cell types contained in the unseparated PBMCs.
Effect of CTLA-4-Fc on IDO mRNA expression and tryptophan catabolism in different cell types. (A) IDO mRNA expression was analyzed in isolated CD4+, CD8+, and CD19+ cells, and unseparated human PBMCs after 12 hours of culture in the absence or presence of CTLA-4-Fc. (B) Unseparated PBMCs were cultured in the absence or presence of CTLA-4-Fc for 12 hours. These PBMCs were then separated into CD4+, CD8+, and CD19+ cells and were analyzed for IDO mRNA expression. For panels A and B, □ indicates control; ▪, CTLA-4-Fc. *P values less than .05 are based on 5 independent experiments. (C) Kyn/Trp ratio was analyzed by HPLC on supernatants collected from unseparated PBMCs cultured in the presence or absence of CTLA-4-Fc or rhIFN-γ; CD4+ T cells were isolated from untreated and CTLA-4-Fc–treated PBMCs and cultured for 24 hours in the same conditions; kyn/Trp ratio was then measured on collected supernatants. Mean values obtained from experiments using cells from 2 separate donors are presented. Mean values plus standard errors are shown.
Effect of CTLA-4-Fc on IDO mRNA expression and tryptophan catabolism in different cell types. (A) IDO mRNA expression was analyzed in isolated CD4+, CD8+, and CD19+ cells, and unseparated human PBMCs after 12 hours of culture in the absence or presence of CTLA-4-Fc. (B) Unseparated PBMCs were cultured in the absence or presence of CTLA-4-Fc for 12 hours. These PBMCs were then separated into CD4+, CD8+, and CD19+ cells and were analyzed for IDO mRNA expression. For panels A and B, □ indicates control; ▪, CTLA-4-Fc. *P values less than .05 are based on 5 independent experiments. (C) Kyn/Trp ratio was analyzed by HPLC on supernatants collected from unseparated PBMCs cultured in the presence or absence of CTLA-4-Fc or rhIFN-γ; CD4+ T cells were isolated from untreated and CTLA-4-Fc–treated PBMCs and cultured for 24 hours in the same conditions; kyn/Trp ratio was then measured on collected supernatants. Mean values obtained from experiments using cells from 2 separate donors are presented. Mean values plus standard errors are shown.
Kynurenine-to-tryptophan ratio is increased in supernatants from CD4+ T cells isolated from CTLA-4-Fc–exposed PBMCs
To determine the functional activity of IDO expressed in PBMCs and, in particular, CD4+ T cells after CTLA-4-Fc exposure, we analyzed the kynurenine-to-tryptophan (kyn/Trp) ratio in supernatants collected from different cell cultures. Unseparated PBMCs from 2 different donors were cultured in control medium or in the presence of CTLA-4-Fc; incubation with rhIFN-γ served as positive control. The supernatants were collected after 24 hours of culture and the kyn/Trp ratio was analyzed by HPLC. The kyn/Trp ratio was increased in CTLA-4-Fc–treated compared with untreated samples (55.2 vs 28.2 μmol/mmol), and in rhIFN-γ–treated (91.0 μmol/mmol) compared with both CTLA-4-Fc–treated and untreated samples (Figure 5C, left bars).
Because CD4+ T cells showed IDO mRNA expression only when cultured as unseparated PBMCs (Figure 5A-B), we analyzed IDO functional activity (kyn/Trp) in CD4+ T cells isolated from untreated and CTLA-4-Fc–treated PBMCs from each donor. Therefore, CD4+ T cells isolated from the untreated PBMCs were cultured for an additional 24 hours in control medium. Similarly, CD4+ T cells isolated from the CTLA-4-Fc–treated PBMCs were cultured for an additional 24 hours in the presence of CTLA-4-Fc. Supernatants were then collected and the kyn/Trp ratio was analyzed. The kyn/Trp ratio showed an increase of approximately 2-fold in CTLA-4-Fc–treated compared with untreated CD4+ T cells (42.3 vs 20.9 μmol/mmol, Figure 5C, right bars), confirming that IDO expressed by CD4+ T cells in our study has functional enzymatic activity.
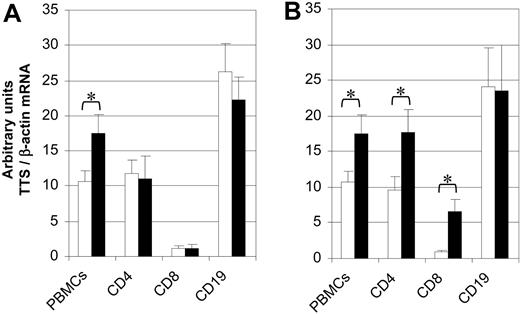
CD4+ and CD8+ T cells increase TTS mRNA expression in response to CTLA-4-Fc when cultured as unseparated PBMCs
As noted in “Introduction,” TTS combines tryptophan with its specific tRNA. TTS expression is induced by IFN-γ, and has been suggested to protect the IDO-expressing cell from tryptophan starvation.18 TTS mRNA expression was evaluated using quantitative real-time PCR in unseparated PBMCs, isolated CD4+ T cells, CD8+ T cells, and B cells cultured for 12 hours in the absence or presence of CTLA-4-Fc. The results, shown in Figure 6A, demonstrate that only unseparated PBMCs showed increased TTS mRNA after exposure to CTLA-4-Fc (P = .041). High basal levels of TTS mRNA, which were not increased upon CTLA-4-Fc exposure, were observed on isolated CD4+ T cells and B cells. Basal level of TTS mRNA on CD8+ T cells was lower and did not increase after culture with CTLA-4-Fc. The same experiment was repeated on CD4+ T cells, CD8+ T cells, and B cells isolated from PBMCs after 12 hours of culture with CTLA-4-Fc. The results, shown in Figure 6B, are summarized as follows: (1) B cells expressed high baseline level of TTS, but did not increase TTS mRNA in response to CTLA-4-Fc; (2) CD4+ T cells expressed baseline TTS mRNA levels comparable with unseparated PBMCs and showed a similar 2-fold increase in response to CTLA-4-Fc exposure; and (3) CD8+ T cells expressed low TTS mRNA levels compared with unseparated PBMCs, but showed a 7-fold increased expression after CTLA-4-Fc exposure. These results suggest that CTLA-4-Fc–induced expression of TTS by CD4+ T cells, similar to CTLA-4-Fc–induced IDO expression, requires the presence of other cells contained in the unseparated PBMCs.
Effect of CTLA-4-Fc on TTS mRNA expression in different cell types. (A) TTS mRNA expression was analyzed in isolated CD4+, CD8+, and CD19+ cells, and unseparated human PBMCs after 12 hours of culture in the absence or presence of CTLA-4-Fc. (B) Unseparated PBMCs were cultured in the absence or presence of CTLA-4-Fc for 12 hours. These PBMCs were then separated into CD4+, CD8+, and CD19+ cells and were analyzed for TTS mRNA expression. □ indicates control; ▪, CTLA-4-Fc. *P values less than .05 are based on 5 independent experiments. Mean values plus standard errors are shown.
Effect of CTLA-4-Fc on TTS mRNA expression in different cell types. (A) TTS mRNA expression was analyzed in isolated CD4+, CD8+, and CD19+ cells, and unseparated human PBMCs after 12 hours of culture in the absence or presence of CTLA-4-Fc. (B) Unseparated PBMCs were cultured in the absence or presence of CTLA-4-Fc for 12 hours. These PBMCs were then separated into CD4+, CD8+, and CD19+ cells and were analyzed for TTS mRNA expression. □ indicates control; ▪, CTLA-4-Fc. *P values less than .05 are based on 5 independent experiments. Mean values plus standard errors are shown.
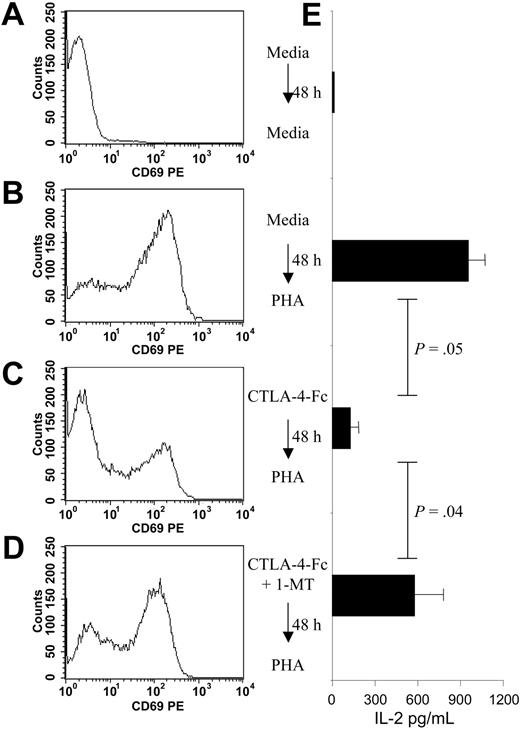
Tryptophan catabolism induced by CTLA-4-Fc treatment of unseparated PBMCs prevents CD4+ T-cell activation
IDO overexpression was reported to be associated with the blocking of T-cell activation and proliferation.9-15 Therefore, we pretreated PBMCs with CTLA-4-Fc and assessed the surface expression of the T-cell activation markers CD69 and CD38 on CD4+ and CD8+ T cells, following activation with infectious influenza A virus (Flu) or with phytohemagglutinin A (PHA). The results are summarized in Table 1. CTLA-4-Fc treatment did not affect the percentage of CD4+ and CD8+ cells (data not shown). Unactivated PBMCs showed a low percentage of CD4+/CD69+ cells (2.5% ± 1.9%) and of CD8+/CD69+ cells (1.9% ± 1.1%). Activation with Flu or PHA significantly increased the percentage of CD4+/CD69+ cells (control: 2.5% ± 1.9%; Flu: 12.5% ± 0.4%; PHA: 23.5% ± 1.6%), and of CD8+/CD69+ cells (control: 1.9% ± 1.1%; Flu: 5.4% ± 0.6%; PHA: 15.8% ± 3.5%). Pretreatment of PBMCs with CTLA-4-Fc for 48 hours significantly inhibited the increase of CD4+/CD69+ cells induced by Flu (5% ± 1.5% vs 12.5% ± 0.4%) or PHA (11.3% ± 2.4% vs 23.5% ± 1.6%), but did not show any effect on CD8+/CD69+ cells (Flu: 5.2% ± 0.3% vs 5.4% ± 0.6%; PHA: 14.0% ± 4.1% vs 15.8% ± 3.5%). No significant differences between CTLA-4-Fc–treated and untreated cells were observed when CD4+/CD38+ and CD8+/CD38+ cells were analyzed. We performed the same experiment using a combination of anti-B7.1 and anti-B7.2 mAbs instead of CTLA-4-Fc to exclude the possibility that the inhibitory effect of CTLA-4-Fc was due to blocking of the B7-CD28 interactions. Pretreatment with anti-B7 mAb had no effect on CD69 expression on CD4+ T cells after Flu or PHA activation of PBMCs (data not shown). To test whether the inhibitory effect of CTLA-4-Fc was due to IDO activation, we preincubated PBMCs with CTLA-4-Fc in the presence of 1-methyl-tryptophan (1-MT), an inhibitory molecule for IDO, and activated these PBMCs with PHA (1 μg/mL) after 48 hours. As shown in Figure 7 and summarized in Table 1, inhibition of IDO activity with 1-MT prevented the negative effect of CTLA-4-Fc on CD4+ T-cell activation, measured as percentage of CD4+/CD69+ cells (21.3% ± 2.6% vs 11.3% ± 2.4%). IDO inhibition with 1-MT could not be performed in experiments with Flu activation, because the final concentration of NaOH (0.02 N) used to dissolve 1-MT interfered with Flu-induced CD4+ T-cell activation. The PHA results indicate that CTLA-4-Fc–induced tryptophan catabolism can inhibit virus- and mitogen-induced CD4+ T-cell activation, without affecting CD8+ T cells.
Effect of CTLA-4-Fc treatment of PBMCs on T-cell activation by influenza A virus and PHA
Treatment/activation . | CD4+CD38+, % . | CD4+CD69+, % . | CD8+CD38+, % . | CD8+CD69+, % . | IL-2, pg/mL . |
|---|---|---|---|---|---|
| None/none | 16.9 ± 6.8 | 2.5 ± 1.9* | 6.7 ± 0.8 | 1.9 ± 1.1* | 6.5 ± 2.4* |
| None/Flu | 18.7 ± 7.9 | 12.5 ± 0.4* | 7.3 ± 2.0 | 5.4 ± 0.6* | 22.3 ± 6.5* |
| CTLA-4/Flu | 23.0 ± 9.7 | 5 ± 1.5* | 8 ± 2.6 | 5.2 ± 0.3 | 5.1 ± 2.5* |
| None/PHA | 21.3 ± 9.3 | 23.5 ± 1.6* | 14.5 ± 0.5 | 15.8 ± 3.5* | 958 ± 91* |
| CTLA-4/PHA | 27.5 ± 5.7 | 11.3 ± 2.4* | 14.7 ± 1.5 | 14.0 ± 4.1 | 135 ± 41* |
| CTLA-4 + 1-MT/PHA | 25.3 ± 4.2 | 21.3 ± 2.6* | 13.8 ± 3.0 | 15.2 ± 3.9 | 580 ± 193* |
Treatment/activation . | CD4+CD38+, % . | CD4+CD69+, % . | CD8+CD38+, % . | CD8+CD69+, % . | IL-2, pg/mL . |
|---|---|---|---|---|---|
| None/none | 16.9 ± 6.8 | 2.5 ± 1.9* | 6.7 ± 0.8 | 1.9 ± 1.1* | 6.5 ± 2.4* |
| None/Flu | 18.7 ± 7.9 | 12.5 ± 0.4* | 7.3 ± 2.0 | 5.4 ± 0.6* | 22.3 ± 6.5* |
| CTLA-4/Flu | 23.0 ± 9.7 | 5 ± 1.5* | 8 ± 2.6 | 5.2 ± 0.3 | 5.1 ± 2.5* |
| None/PHA | 21.3 ± 9.3 | 23.5 ± 1.6* | 14.5 ± 0.5 | 15.8 ± 3.5* | 958 ± 91* |
| CTLA-4/PHA | 27.5 ± 5.7 | 11.3 ± 2.4* | 14.7 ± 1.5 | 14.0 ± 4.1 | 135 ± 41* |
| CTLA-4 + 1-MT/PHA | 25.3 ± 4.2 | 21.3 ± 2.6* | 13.8 ± 3.0 | 15.2 ± 3.9 | 580 ± 193* |
Mean values ± SEM are shown.
Statistically significant difference (P < .05).
CTLA-4-Fc inhibits PHA-induced IL-2 production and CD4+ T-cell activation by an IDO-dependent mechanism. CD69 expression on gated CD4+ T cells from PBMCs in 4 different conditions: (A) no pretreatment and no activation; (B) no pretreatment and subsequent PHA activation; (C) CTLA-4-Fc pretreatment and subsequent PHA activation; and (D) CTLA-4-Fc + 1-MT pretreatment and subsequent PHA activation. A single representative experiment is shown. (E) IL-2 production using the 4 different conditions mentioned in panels A-D. Mean values obtained from experiments using cells from 3 separate donors are presented. Mean values plus standard errors are shown.
CTLA-4-Fc inhibits PHA-induced IL-2 production and CD4+ T-cell activation by an IDO-dependent mechanism. CD69 expression on gated CD4+ T cells from PBMCs in 4 different conditions: (A) no pretreatment and no activation; (B) no pretreatment and subsequent PHA activation; (C) CTLA-4-Fc pretreatment and subsequent PHA activation; and (D) CTLA-4-Fc + 1-MT pretreatment and subsequent PHA activation. A single representative experiment is shown. (E) IL-2 production using the 4 different conditions mentioned in panels A-D. Mean values obtained from experiments using cells from 3 separate donors are presented. Mean values plus standard errors are shown.
Tryptophan catabolism induced by CTLA-4-Fc treatment of unseparated PBMCs prevents IL-2 production
To evaluate the functional effect of CTLA-4-Fc–induced tryptophan catabolism on cell activation, we analyzed IL-2 production in supernatants from PBMCs cultured for 48 hours with CTLA-4-Fc and then activated with Flu or PHA. The results, summarized in Figure 7E and at the bottom of Table 1, showed that (1) both Flu and PHA induced a significant increase of IL-2 production compared with control (control: 6.5 ± 2.4 pg/mL; Flu: 22.3 ± 6.5 pg/mL; PHA: 958 ± 91 pg/mL); (2) pretreatment with CTLA-4-Fc completely inhibited Flu-induced IL-2 production (22.3 ± 6.5 vs 5.1 ± 2.5); (3) CTLA-4-Fc pretreatment reduced PHA-induced IL-2 production by 7-fold (958 ± 91 vs 135 ± 41); and (4) addition of 1-MT to the CTLA-4-Fc–treated cells partially restored PHA-induced IL-2 production (580 ± 163 vs 135 ± 41), interfering with the inhibitory effect of CTLA-4-Fc.
Discussion
Indoleamine 2,3 dioxygenase (IDO) up-regulation by CTLA-4 and IFN-γ results in the inhibition of T-cell activation and proliferation by tryptophan starvation.9-15 The binding of CTLA-4 to B7 costimulatory molecules was recently shown to induce IDO expression in murine and human DCs.23-25 We cultured human monocytes and monocyte-derived DCs with CTLA-4-Fc to confirm the recent report of induced IDO expression.25 Monocytes and immature DCs expressed low basal IDO mRNA levels, whereas mature DCs showed higher IDO levels, which were increased upon CTLA-4-Fc exposure. We also cultured human PBMCs with CTLA-4-Fc, and demonstrated that the binding of CTLA-4 to the costimulatory molecules B7.1 and B7.2 induced IFN-γ production, which subsequently induced IDO expression. The expression of IDO in an enzymatically active form was also confirmed by the elevated kyn/Trp ratio in supernatants from CTLA-4-Fc–treated PBMCs.
The culture of isolated CD4+ T cells, CD8+ T cells, and B cells resulted in low basal levels of IDO mRNA expression, which was not increased by CTLA-4-Fc. However, when these lymphocyte subsets were positively selected after exposure of PBMCs to CTLA-4-Fc, only CD4+ T cells expressed increased IDO at levels comparable with the unseparated PBMCs. The enzymatic activity of IDO expressed in CD4+ T cells was demonstrated by the production of kynurenine by those cells (kyn/Trp ratio, Figure 5C). Our finding that CTLA-4–induced IDO expression occurs in CD4+ T cells only when cultured as unseparated PBMCs suggests that interaction with other cell types is essential for CD4+ T cells to maintain a high baseline IDO level and to respond to CTLA-4-Fc by increasing IDO expression. Since activated human CD4+ T cells express B7.1 and B7.2, as well as major histocompatibility complex (MHC) class II,48-50 they may acquire some functional characteristics of APCs, including the ability to express IDO when exposed to CTLA-4-Fc. Recent studies using B7 knock-out mice showed that the expression of costimulatory molecules on CD4+ T cells is responsible for down-modulating responses to alloantigens, and that this effect is dependent on CTLA-4-B7 interactions between T cells.51 Our data provide the first report demonstrating that CD4+ T cells can express IDO when exposed to CTLA-4-Fc, suggesting that the immunomodulatory effect of B7 expression on CD4+ T cells may involve tryptophan catabolism.
Tryptophan is an essential amino acid that is required by all cells to synthesize proteins. The depletion of tryptophan in the microenvironment, which results from IDO overexpression, affects T-cell activity without exerting negative effects on the IDO-expressing cells (DCs or macrophages).12,15 It is not known why IDO-expressing cells themselves are not susceptible to tryptophan depletion. One possibility is that activated T lymphocytes have a higher rate of protein synthesis compared with DCs, which could result in a higher sensitivity to IDO-induced tryptophan depletion. It was reported that activated T lymphocytes have increased capacity to synthesize aminoacyl-tRNA with several different amino acids.52,53 An alternative, but not mutually exclusive, mechanism is that IDO-expressing cells are in some way protected against tryptophan starvation. It has been suggested that IDO-expressing cells avoid the negative effects of tryptophan depletion by increasing the expression of TTS.18 Tryptophanyl-tRNA-synthetase is the only aminoacyl-tRNA-synthetase whose expression is induced by IFN-γ.4-8 This unique property makes TTS a prime candidate for protecting the IDO-expressing cells from tryptophan starvation.18 Overexpression of TTS in the APCs could permit the production of a pool of Trp-tRNA, providing a reservoir for this essential amino acid that would be protected from degradation by IDO and available for protein synthesis. We investigated the effects of CTLA-4-Fc exposure on the expression of TTS mRNA in different cell types. Our results showed that human PBMCs overexpressed TTS when exposed to CTLA-4-Fc. Isolated CD4+ T cells, CD8+ T cells, and B cells expressed relatively high constitutive levels of TTS, which were not increased when these isolated populations were exposed to CTLA-4-Fc. However, when leukocyte populations were sorted after CTLA-4-Fc treatment of PBMCs, CD4+ T cells and CD8+ T cells showed increased TTS expression. Monocytes and DCs expressed very low levels of TTS compared with lymphocytes, which is consistent with the lymphocytes having a higher rate of protein synthesis than DCs.52,53 However, when treated with CTLA-4-Fc, only mDCs increased TTS expression. When cultured as unseparated PBMCs, CD8+ T cells appeared to be distinct from CD4+ T cells in that they exhibited lower basal levels of both IDO and TTS, and CTLA-4-Fc exposure resulted in increased TTS but not IDO expression only in the CD8+ T cells. This characteristic of CD8+ T cells might make them less susceptible than CD4+ T cells to CTLA-4–induced tryptophan starvation.
The mechanism by which IDO inhibits T-cell activity is considered to be tryptophan starvation.9-15 Because we demonstrated differences in CTLA-4-Fc–induced IDO and TTS expression in CD4+ and CD8+ T cells cultured as unseparated PBMCs, we tested the effect of viral- and mitogen-induced T-cell activation on these 2 T-cell subsets. We exposed PBMCs to Flu or PHA, and analyzed the surface expression of the activation markers CD69 and CD38 on CD4+ and CD8+ T cells. The percentage of CD4+/CD69+ cells was increased after Flu or PHA exposure. Pretreatment of PBMCs with CTLA-4-Fc for 48 hours before activation inhibited overexpression of CD69 by CD4+ T cells. This effect was not observed when anti-B7.1 and anti-B7.2 mAbs were used instead of CTLA-4-Fc, indicating that the inhibitory effect was due to an active function of CTLA-4, and not simply to the blocking of B7 molecules. In addition, IL-2 production induced by Flu or PHA in unseparated PBMCs was strongly inhibited by pretreatment with CTLA-4-Fc. The involvement of IDO in the down-modulatory effect of CTLA-4-Fc was demonstrated by the restoration of mitogen-induced CD4+ T-cell activation and IL-2 production by blocking IDO activity with 1-MT. Moreover, both Flu and PHA induced a statistically significant increase in the percentage of CD8+/CD69+ cells, which was not affected by pretreatment with CTLA-4-Fc, suggesting that CD4+ T cells might be more susceptible to CTLA-4–induced tryptophan starvation than CD8+ T cells. It is noteworthy that in PBMCs treated with CTLA-4-Fc, only CD8+ T cells showed low IDO mRNA but increased TTS expression. This exception to the IDO-TTS parallelism that we observed in other cell types could partially explain why CD8+ T-cell activation by Flu was not affected by CTLA-4-Fc exposure.
In summary, we demonstrate that CTLA-4-Fc molecules interact with B7.1 and B7.2, resulting in increased expression of IFN-γ and IDO in human mDCs and CD4+ T cells, but not in other populations of blood leukocytes. We uniquely demonstrate a CTLA-4-Fc–induced concomitant increased expression of IDO and TTS, raising the possibility of a mechanism for protecting IDO-expressing/producing cells from self-destruction by tryptophan starvation. Furthermore, we show that only CD8+ T cells increased TTS but not IDO mRNA when PBMCs are treated with CTLA-4-Fc. This finding suggests that CD8+ T cells may be more protected than CD4+ T cells under condition of CTLA-4–induced tryptophan starvation. This particular feature of CD8+ T cells is consistent with our findings that virus- and mitogen-induced activation of CD4+ but not CD8+ T cells is impaired by treatment of PBMCs with CTLA-4-Fc, and supports the hypothesis18 that TTS function is a counterbalance that protects the cell against the detrimental effect of IDO-dependent tryptophan catabolism. It will be of interest to determine whether certain pathologic conditions can reduce the TTS expression, resulting in an enzymatic imbalance that would favor tryptophan catabolism and CD4+ T-cell hyporesponsiveness.
Prepublished online as Blood First Edition Paper, October 5, 2004; DOI 10.1182/blood-2004-06-2089.
Supported by the Intramural Research Program, CCR, NCI, NIH, and by the Austrian Federal Ministry of Social Affairs and Generations.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 U.S.C. section 1734.
The authors thank Dr J. S. Shaw, Experimental Immunology Branch, CCR, NCI, NIH, for reviewing the manuscript and for helpful suggestions.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal