Abstract
Deletions of derivative chromosome 9 [der(9)] can be identified by fluorescence in situ hybridization (FISH) in 10% to 15% of patients with chronic myeloid leukemia (CML). Patients with der(9) deletions have been reported to have an adverse outcome when treated with chemotherapy, interferon, and possibly imatinib mesylate. We investigated the frequency and prognostic significance of der(9) deletions among 352 patients with CML treated with imatinib mesylate at our institution, in whom a deletion status of der(9) was determined. Thirty-three patients (9%; 95% CI 0.07, 0.13) (30 in chronic phase, 3 in accelerated phase) had der(9) deletions. The rates of major (82% vs 79%, P = 0.82) and complete cytogenetic response (76% vs 66%, P = .33) with imatinib mesylate therapy were similar in patients with and without der(9) deletions, respectively. After a median follow-up of 28 months, there was no difference in overall survival (P = .30) or response duration (P = .49) in patients with and without deletions. In a multivariate analysis, der(9) deletions had no significant impact on response, survival, or response duration. We conclude that treatment with imatinib mesylate overcomes the adverse prognostic significance of der(9) deletions in patients with CML.
Introduction
Chronic myelogenous leukemia (CML) is characterized by the Philadelphia chromosome (Ph), t(9;22)(q34;q11.2).1,2 This results in the formation of the chimeric fusion gene BCR-ABL.3-7 This is translated into a constitutively activated protein tyrosine kinase that influences several signaling pathways, resulting in increased proliferation and reduced apoptosis.8 Clinically, CML is characterized by a bior triphasic course, with an initial chronic phase (CP)9,10 and a median survival of 4 to 6 years. Unless the disease can be eliminated, it progresses to the blastic phase (BP).9 Approximately two thirds of patients progress to the BP through an accelerated phase (AP). Despite the common molecular origin characterized by the presence of the Ph chromosome, the clinical course of CML is variable, with some patients progressing rapidly, while others may remain in CP for many years.9
Submicroscopic deletions of der(9) have been recently identified using fluorescence in situ hibridization (FISH) in 10% to 15% of patients with classic Ph+ CML,11-16 and in as many as 30% to 40% of patients with variant Ph translocations.11-14 These deletions are thought to occur at the same time as the Ph translocation rather than as a secondary event, and may involve the loss of sequences from chromosome 9, chromosome 22, or both.11,15,17,18 They are usually large, spanning several megabases, and are usually located in the regions flanking the BCR-ABL breakpoints on the der(9).11,12,15 Several studies have suggested that patients carrying der(9) deletions have an unfavorable prognosis when treated with hydroxyurea, interferon alpha (IFN-α), or bone marrow transplantation.11,14,19 Indeed, it has been suggested that the presence of der(9) deletions may be a more significant prognostic indicator than the Sokal or Hasford scoring systems.14
Imatinib mesylate (Gleevec; Novartis, Basel, Switzerland) is a specific Bcr-Abl tyrosine kinase inhibitor with significant clinical activity in patients with CML. A complete cytogenetic remission has been achieved in 40% to 60% of patients in CP after failing therapy with IFN-α, and in up to 80% to 90% of previously untreated patients.20,21 After a median follow-up of 18 months, nearly 40% of patients treated with imatinib mesylate had at least a 3-log reduction in the levels of BCR-ABL/ABL.22 In more advanced stages of CML, overall response rates are lower and response durations are shorter.23-26 Imatinib mesylate has been shown to overcome the prognostic significance of variables historically associated with poor prognosis, such as advanced age27 and variant Ph translocations.28 There are limited data regarding the prognosis of patients with der(9) deletions treated with imatinib. One recent report suggested that imatinib only partially overcomes the adverse prognostic impact of der(9) deletions.16
We performed this study to investigate the frequency of der(9) deletions among patients treated with imatinib, their clinical characteristics, and their outcome after imatinib therapy.
Patients, materials, and methods
Study group
From December 1998 to June 2003, 838 patients in different CML phases received imatinib at MD Anderson Cancer Center. Approval was obtained from the University of Texas M.D. Anderson Cancer Center institutional review board for these studies. Informed consent was provided according to the Declaration of Helsinki. The Vysis extra-signal (ES) probe (Vysis, Dowers Grove, IL), which is designed to detect the Ph chromosome and can identify der(9) deletions by FISH, was routinely used to evaluate patients prior to the start of therapy since May 2002. Thus, 352 patients were evaluable for the presence of der(9) deletions and constitute the basis for this analysis. The definitions of CP, AP, and BP, as well as the definition of IFN-α failure were the same used in published studies using imatinib.20,21,23,24 Briefly, patients were considered to be in AP if they had 15% or more blasts,30% or more blasts plus promyelocytes, 20% or more basophils, less than 100 × 109/L platelets unrelated to therapy, or cytogenetic clonal evolution. Blastic phase was defined as the presence of 30% or more blasts in the peripheral blood or bone marrow, or extramedullary blastic disease. All other patients were considered to be in CP. IFN-α failure was defined as follows: hematologic failure included hematologic resistance (failure to achieve complete hematologic response [CHR], as defined later, after 6 months or more of IFN-α) or relapse (disease recurrence after achieving CHR); cytogenetic failure included resistance (Ph of 65% or more after at least 12 months of IFN-α) or relapse (Ph increase greater than 30% documented on 2 occasions, or a single increase to 65% or more); and intolerance defined as grades 3 to 4 nonhematologic toxicity (according to the National Cancer Institute [NCI] Common Toxicity Criteria [CTC], version 2.0) not responding to adequate management.
Evaluation during treatment
Before the start of treatment, patients were evaluated with history and physical exam, complete blood cell count (CBC) with differential, and blood chemistry including total bilirubin, creatinine, and alanine aminotransferase. All patients had a pretreatment bone marrow evaluation for morphology, cytogenetic analysis, FISH, and real-time polymerase chain reaction (PCR). Cytogenetic analysis was performed by the G-banding technique. For chromosome analysis, at least 20 metaphases were analyzed, and bone marrow specimens were examined on direct or short-term (24-hour) cultures. After treatment was started, patients were evaluated with CBC and blood chemistry weekly during the first 1 to 3 months, then every 2 to 6 weeks. Bone marrow aspirations for morphology, cytogenetics (FISH when routine cytogenetic analysis is unanalyzable), and PCR were repeated every 3 to 4 months for the first year, and every 6 months thereafter. Patients were followed for survival at least every 3 months. Drug toxicity was evaluated at each visit and graded according to the NCI CTC.
Response criteria
Response criteria were as previously described.29 Briefly, a CHR was defined as a white blood cell count of less than 10 × 109/L, a platelet count of less than 450 × 109/L, no immature cells (blasts, promyelocytes, myelocytes) in the peripheral blood, and disappearance of all signs and symptoms related to leukemia (including palpable splenomegaly) lasting for at least 4 weeks. A CHR was further categorized by the best cytogenetic response as complete (0% Ph+), partial (1% to 34% Ph+), and minor (35% to 90% Ph+). A major cytogenetic response included complete plus partial cytogenetic responses (ie, Ph+ < 35%). Complete remission duration was considered from the time a complete cytogenetic response was first achieved to the time when the patient first lost complete cytogenetic remission status (ie, an increase to > 0% Ph+ cells). Survival was calculated from the time treatment began until death from any cause, or last follow-up.
FISH
Bone marrow cells were analyzed by FISH using the locus-specific identifier (LSI) BCR/ABL dual-color ES probe (Vysis) according to the manufacturer's instructions. This probe has been designed to reduce the rate of false-positive results by marking the argininosuccinate synthetase (ASS) gene, thus providing an extra signal on chromosome 9. In Ph+ cells, colabeling of the ABL and BCR probes renders a yellow signal, indicating the fusion (BCR-ABL) of the orange and the green probes, 2 orange signals corresponding to the nontranslocated ABL, and 1 green signal on the nontranslocated BCR gene. Ph+ cells with der(9) deletions will only show 1 orange and 1 green signal, in addition to the fusion signal.
Treatment and dose modifications
Patients in CP were treated with 400 mg (n = 160), 600 mg (n = 32), or 800 mg (n = 128) imatinib mesylate daily. All patients in AP received 600 mg imatinib mesylate daily. Overall, 160 patients received 400 mg daily; 64 patients, 600 mg daily; and 128 patients, 800 mg daily. Treatment interruptions and dose adjustments were as previously reported.20,23,30-32
Statistical considerations
Clinical and biologic characteristics were analyzed for their associations with survival using the log-rank test and multivariate Cox proportional hazards models. These characteristics included stage, dose, clinical features at the time of imatinib therapy was started, and der(9) deletions. Estimates of survival curves were calculated according to the Kaplan-Meier productlimit method33 from the time of treatment with imatinib. Survival times were compared by means of the log-rank test.34 Associations between categorical variables were assessed via cross-tabulation and Fisher exact test or the Mantel Haenszel test.35 Multivariate logistic regression analysis was used to assess the relationship between various predictors of interest and response. The Cox proportional hazards regression model36 was used to assess the relationship characteristics and survival. Goodness of fit was assessed by Martingale residual plots and likelihood ratio statistics. Univariate and multivariate Cox proportional hazard models were developed. Predictive variables in the Cox proportional hazards regression model were reviewed to assess the need for transformation based on smoothed Martingale residual plots. Predictive variables with P values of less than .10 for the univariate Cox proportional hazards model were included in a multivariate model. All computations were carried out on Dell PCs (Round Rock, TX) using the Windows NT operating system (Microsoft, Redmond, CA) in SAS (SAS Institute, Cary, NC) using standard SAS procedures.
Results
Because only 352 (42%) of 838 patients treated with imatinib at our institution during the study period were evaluable for the analysis, we first determined if patients who had been assessed for the presence of der(9) deletions constituted a representative cohort of the entire population. Table 1 summarizes the patient characteristics and outcome of treatment with imatinib mesylate for patients in CP, which represented the largest population, for both cohorts of patients. The pretreatment characteristics, cytogenetic response to imatinib mesylate, and overall survival were identical for patients with and without available information for der(9) deletions. This was also true for patients in transformation (data not shown). These results indicated that the study population was representative of the total population of patients with CML treated with imatinib mesylate in our institution.
Outcome after imatinib therapy for patients in whom der(9) deletions was assessed versus those in whom it was not assessed
. | Assessment of der(9) deletions . | . | . | |
|---|---|---|---|---|
. | Investigated . | Not investigated . | P . | |
| Median age, y (range) | 51 (15-84) | 52 (16-81) | .65 | |
| Hasford, % | ||||
| Low | 53 | 50 | .38 | |
| Intermediate | 39 | 46 | ||
| High | 8 | 5 | ||
| Interferon failure, no. | 168 | 235 | ||
| Complete cytogenetic remission, % | 56 | 55 | .95 | |
| 3-y survival, % | 90 | 87 | .5 | |
| Previously untreated, no. | 152 | 61 | ||
| Complete cytogenetic remission, % | 82 | 77 | .45 | |
| 3-y survival, % | 95 | 95 | .99 | |
. | Assessment of der(9) deletions . | . | . | |
|---|---|---|---|---|
. | Investigated . | Not investigated . | P . | |
| Median age, y (range) | 51 (15-84) | 52 (16-81) | .65 | |
| Hasford, % | ||||
| Low | 53 | 50 | .38 | |
| Intermediate | 39 | 46 | ||
| High | 8 | 5 | ||
| Interferon failure, no. | 168 | 235 | ||
| Complete cytogenetic remission, % | 56 | 55 | .95 | |
| 3-y survival, % | 90 | 87 | .5 | |
| Previously untreated, no. | 152 | 61 | ||
| Complete cytogenetic remission, % | 82 | 77 | .45 | |
| 3-y survival, % | 95 | 95 | .99 | |
Deletion of derivative chromosome 9
Bone marrow specimens from 352 patients treated with imatinib mesylate were analyzed by FISH for the presence of deletions of der(9). Thirty-three patients (9%; 95% CI 0.07-0.13) had the deletions: 30 (91%) were in CP (11 in late CP after IFN-α failure and 19 previously untreated), and 3 (9%) were in AP, a distribution similar to that of patients without deletions.
Clinical and laboratory characteristics according to deletions of der(9)
The characteristics of patients with and without deletions at the time imatinib mesylate therapy was started are presented in Table 2. Patients without deletions were older, while patients with deletions were more frequently anemic, although these differences were not statistically significant. There were no differences in other patient characteristics; this was reflected by the similar distribution of patients within Hasford risk groups. Since 2001, higher doses of imatinib mesylate have been investigated at our institution30,31 for patients in CP. A significantly higher percentage of patients with der(9) deletions (58%) were treated with higher doses of imatinib mesylate (800 mg) compared with those without der(9) deletions (34%; P = .026).
Clinical characteristics of patients with and without der(9) deletions
Covariate . | Chromosome 9 deletion (n = 33) . | Non-chromosome 9 deletion (n = 319) . | P . |
|---|---|---|---|
| Age, no. (%) | .079 | ||
| 60 y or older | 6 (18) | 109 (34) | |
| Sex | .20 | ||
| Male, no. (%) | 22 (67) | 175 (55) | |
| Albumin, g/L, median (range) | 4.1 (3.1-4.7) | 4 (2.5-5.3) | .47 |
| Bilirubin, μM/L, median (range) | 8.55 (1.71-22.23) | 8.55 (1.71-30.78) | .56 |
| Creatinine, μM, median (range) | 79.56 (53.04-123.76) | 79.56 (44.2-238.68) | .82 |
| Hemoglobin less than 12 g/L, no. (%) | 21 (64) | 145 (46) | .066 |
| Bone marrow basophils, median (range) | 2 (0-13) | 2 (0-40) | .67 |
| Bone marrow blasts 5% or greater, no. (%) | 6 (18) | 38 (12) | .28 |
| Platelets, no. (%) | .87 | ||
| 450 × 109/L to less than 700 × 109/L | 6 (18) | 53 (17) | |
| 700 × 109/L or more | 4 (12) | 33 (10) | |
| Peripheral blood basophils 7% or greater, no. (%) | 8 (24) | 55 (17) | .34 |
| Peripheral blood blasts present, no. (%) | 10 (30) | 93 (30) | .73 |
| Splenomegaly present, no. (%) | 11 (33) | 70 (22) | .19 |
| WBC 50 × 109/L, no. (%) | 8 (24) | 73 (23) | .94 |
| Ph+ at start of therapy less than 90%, no. (%) | 5 (15) | 36 (12) | .57 |
| Hepatomegaly present, no. (%) | 2 (6) | 11 (4) | .36 |
| Time from diagnosis to treatment, no. (%) | .69 | ||
| Less than 1 y | 20 (61) | 165 (52) | |
| 1-2 y | 7 (21) | 81 (25) | |
| 3 y or more | 6 (18) | 73 (23) | |
| Clonal evolution, no. (%) | 5 (15) | 36 (11) | .57 |
| Hasford risk group, no. (%) | .51 | ||
| Low | 21 (64) | 179 (57) | |
| Intermediate | 9 (27) | 115 (37) | |
| High | 3 (7) | 21 (7) | |
| Response to IFN-α therapy, no. (%) | .4 | ||
| Untreated | 20 (61) | 142 (45) | |
| Cytogenetic resistance | 7 (21) | 76 (24) | |
| Hematologic resistance | 1 (3) | 25 (8) | |
| Intolerant | 5 (15) | 75 (24) | |
| Stage, no. (%) | .20 | ||
| Chronic with prior therapy | 11 (33) | 157 (49) | |
| Chronic without prior therapy | 19 (58) | 133 (42) | |
| Accelerated | 3 (9) | 28 (9) | |
| Performance status, no. (%) | .82 | ||
| 2-4 | 10 (30) | 111 (64) | |
| Imatinib dose, no. (%) | .026 | ||
| 400 mg | 9 (27) | 151 (47) | |
| 600 mg | 5 (15) | 59 (19) | |
| 800 mg | 19 (58) | 109 (34) |
Covariate . | Chromosome 9 deletion (n = 33) . | Non-chromosome 9 deletion (n = 319) . | P . |
|---|---|---|---|
| Age, no. (%) | .079 | ||
| 60 y or older | 6 (18) | 109 (34) | |
| Sex | .20 | ||
| Male, no. (%) | 22 (67) | 175 (55) | |
| Albumin, g/L, median (range) | 4.1 (3.1-4.7) | 4 (2.5-5.3) | .47 |
| Bilirubin, μM/L, median (range) | 8.55 (1.71-22.23) | 8.55 (1.71-30.78) | .56 |
| Creatinine, μM, median (range) | 79.56 (53.04-123.76) | 79.56 (44.2-238.68) | .82 |
| Hemoglobin less than 12 g/L, no. (%) | 21 (64) | 145 (46) | .066 |
| Bone marrow basophils, median (range) | 2 (0-13) | 2 (0-40) | .67 |
| Bone marrow blasts 5% or greater, no. (%) | 6 (18) | 38 (12) | .28 |
| Platelets, no. (%) | .87 | ||
| 450 × 109/L to less than 700 × 109/L | 6 (18) | 53 (17) | |
| 700 × 109/L or more | 4 (12) | 33 (10) | |
| Peripheral blood basophils 7% or greater, no. (%) | 8 (24) | 55 (17) | .34 |
| Peripheral blood blasts present, no. (%) | 10 (30) | 93 (30) | .73 |
| Splenomegaly present, no. (%) | 11 (33) | 70 (22) | .19 |
| WBC 50 × 109/L, no. (%) | 8 (24) | 73 (23) | .94 |
| Ph+ at start of therapy less than 90%, no. (%) | 5 (15) | 36 (12) | .57 |
| Hepatomegaly present, no. (%) | 2 (6) | 11 (4) | .36 |
| Time from diagnosis to treatment, no. (%) | .69 | ||
| Less than 1 y | 20 (61) | 165 (52) | |
| 1-2 y | 7 (21) | 81 (25) | |
| 3 y or more | 6 (18) | 73 (23) | |
| Clonal evolution, no. (%) | 5 (15) | 36 (11) | .57 |
| Hasford risk group, no. (%) | .51 | ||
| Low | 21 (64) | 179 (57) | |
| Intermediate | 9 (27) | 115 (37) | |
| High | 3 (7) | 21 (7) | |
| Response to IFN-α therapy, no. (%) | .4 | ||
| Untreated | 20 (61) | 142 (45) | |
| Cytogenetic resistance | 7 (21) | 76 (24) | |
| Hematologic resistance | 1 (3) | 25 (8) | |
| Intolerant | 5 (15) | 75 (24) | |
| Stage, no. (%) | .20 | ||
| Chronic with prior therapy | 11 (33) | 157 (49) | |
| Chronic without prior therapy | 19 (58) | 133 (42) | |
| Accelerated | 3 (9) | 28 (9) | |
| Performance status, no. (%) | .82 | ||
| 2-4 | 10 (30) | 111 (64) | |
| Imatinib dose, no. (%) | .026 | ||
| 400 mg | 9 (27) | 151 (47) | |
| 600 mg | 5 (15) | 59 (19) | |
| 800 mg | 19 (58) | 109 (34) |
Response to imatinib mesylate therapy
The response to imatinib mesylate is shown in Table 3 according to stage and prior therapy. A complete cytogenetic response was achieved in 126 (83%) of 151 previously untreated patients who received imatinib mesylate in CP and in 93 (55%) of 168 of patients in CP who had failed prior to IFN-α therapy. Among 31 patients in AP, 30 (97%) achieved CHR, and 20 (65%) a major cytogenetic response. Twenty-seven (82%) of the 33 (95% CI 0.65-0.93) patients with der(9) deletions achieved a major cytogenetic response; this was complete in 25 (76%) patients (95% CI 0.58-0.89). This was comparable to the rates observed in patients without deletions: major cytogenetic response in 251 (79%) patients (95% CI 0.74-0.83; P = .82), and complete cytogenetic response in 210 (66%) patients (95% CI 0.61-0.71; P = 0.33). Among patients with and without deletions who had failed IFN-α–based therapies, the rates of major (73% vs 68%, P = 1.0) or complete (55% vs 64%, P = .75) cytogenetic responses were similar with imatinib mesylate. The same was true for previously untreated patients: major cytogenetic response rates were 95% versus 95% (P = 1.0); complete cytogenetic response rates were 95% versus 82% (P = .20). For patients in AP, 2 of the 3 patients with der(9) deletions achieved a major cytogenetic response, a rate similar to that observed in patients without deletions (18 [64%] of 28; P = 1.0).
Response to imatinib by CML phase and deletion of der(9) status
. | No. (%) . | . | . | . | ||
|---|---|---|---|---|---|---|
| . | . | Der(9) deletions . | . | . | ||
| Disease stage and cytogenetic response . | Overall . | Yes . | No . | P . | ||
| Chronic phase previously untreated | 151 (100) | 19 (100) | 132 (100) | |||
| Major | 144 (95) | 18 (95) | 126 (95) | > .99 | ||
| Complete | 126 (83) | 18 (95) | 108 (82) | .20 | ||
| Chronic phase after IFN-α failure | 168 (100) | 11 (100) | 157 (100) | |||
| Major | 115 (68) | 8 (73) | 107 (68) | > .99 | ||
| Complete | 93 (55) | 7 (64) | 86 (55) | .75 | ||
| Accelerated phase | 31 (100) | 3 (100) | 28 (100) | |||
| Major | 20 (65) | 2 (67) | 18 (64) | > .99 | ||
| Complete | 17 (55) | 1 (33) | 16 (57) | .57 | ||
. | No. (%) . | . | . | . | ||
|---|---|---|---|---|---|---|
| . | . | Der(9) deletions . | . | . | ||
| Disease stage and cytogenetic response . | Overall . | Yes . | No . | P . | ||
| Chronic phase previously untreated | 151 (100) | 19 (100) | 132 (100) | |||
| Major | 144 (95) | 18 (95) | 126 (95) | > .99 | ||
| Complete | 126 (83) | 18 (95) | 108 (82) | .20 | ||
| Chronic phase after IFN-α failure | 168 (100) | 11 (100) | 157 (100) | |||
| Major | 115 (68) | 8 (73) | 107 (68) | > .99 | ||
| Complete | 93 (55) | 7 (64) | 86 (55) | .75 | ||
| Accelerated phase | 31 (100) | 3 (100) | 28 (100) | |||
| Major | 20 (65) | 2 (67) | 18 (64) | > .99 | ||
| Complete | 17 (55) | 1 (33) | 16 (57) | .57 | ||
By univariate analysis, characteristics previously reported to have prognostic significance were associated with response, including percentage of bone marrow or peripheral blood blasts and basophils, spleen size, pretreatment percentage of Ph+ metaphases, time from diagnosis, performance status, response to IFN-α among previously treated patients, and Hasford risk group. As previously reported,30,31 the use of high-dose imatinib mesylate was also associated with a higher response rate. All variables were then entered in a multivariate analysis and the results of this analysis for complete cytogenetic remission are shown in Table 4. Older age, larger spleen size, presence of peripheral blood blasts, and a higher percentage of Ph+ metaphases had an adverse impact on response, while treatment with high-dose imatinib mesylate was associated with a better probability of response rate. The presence of der(9) deletions was not associated with response probability in univariate analysis, and was also not significant when included in the multivariate analysis (P = .48). The results were similar when analyzed for probability of major cytogenetic response.
Multivariate logistic regression model in estimating the association between deletion of chromosome 9 and complete response, considering other covariates in the model
Variable . | Parameter estimate . | Standard error . | P . | Odds ratio . |
|---|---|---|---|---|
| Age, 60 y and older vs less than 60 y | -0.68 | 0.28 | .015 | 0.51 |
| Spleen, more than 0 cm vs 0 cm BCM | -0.75 | 0.36 | .038 | 0.47 |
| PB blasts, more than 0% vs 0 % | -1.24 | 0.54 | .021 | 0.29 |
| Ph+ at start, 90% or greater vs less than 90% | -1.17 | 0.49 | .017 | 0.31 |
| Stage, CP untreated vs CP IFN failure | 1.02 | 0.34 | .003 | 2.77 |
| Stage, AP vs CP IFN failure | 1.15 | 0.63 | .068 | 3.15 |
| Dosage, 800 mg vs 400 mg | 1.03 | 0.36 | .004 | 2.81 |
| Der(9) deletions | -0.33 | 0.47 | .48 | 0.72 |
Variable . | Parameter estimate . | Standard error . | P . | Odds ratio . |
|---|---|---|---|---|
| Age, 60 y and older vs less than 60 y | -0.68 | 0.28 | .015 | 0.51 |
| Spleen, more than 0 cm vs 0 cm BCM | -0.75 | 0.36 | .038 | 0.47 |
| PB blasts, more than 0% vs 0 % | -1.24 | 0.54 | .021 | 0.29 |
| Ph+ at start, 90% or greater vs less than 90% | -1.17 | 0.49 | .017 | 0.31 |
| Stage, CP untreated vs CP IFN failure | 1.02 | 0.34 | .003 | 2.77 |
| Stage, AP vs CP IFN failure | 1.15 | 0.63 | .068 | 3.15 |
| Dosage, 800 mg vs 400 mg | 1.03 | 0.36 | .004 | 2.81 |
| Der(9) deletions | -0.33 | 0.47 | .48 | 0.72 |
BCM indicates below costal margin; PB, peripheral blood; CP, chronic phase; AP, accelerated phase; and IFN-α, interferon alpha.
Survival
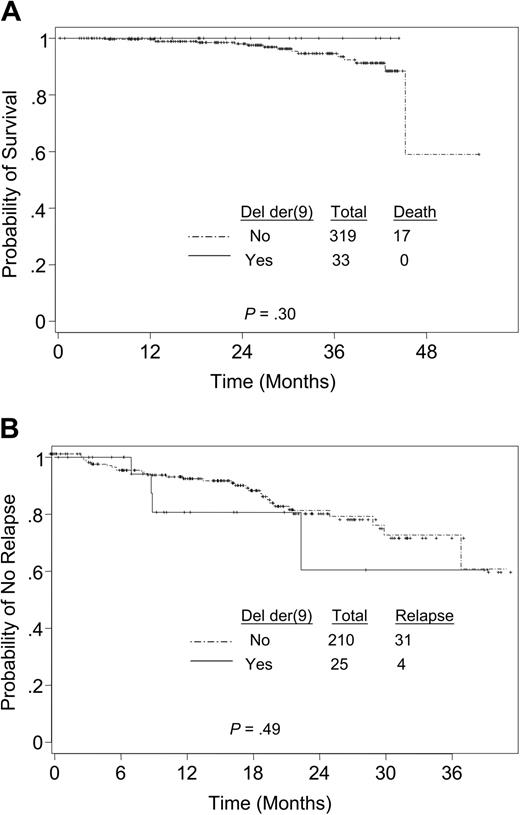
After a median follow-up of 28 months, 17 (5%) patients died. All deaths occurred in the cohort of patients without deletions. For the total population, the estimated 3-year survival rate was 94% (95% CI 0.92-0.97). By univariate analysis, age older than 60 years, presence of peripheral blood blasts, elevated white cell count of 50 × 109/L or more, and response to prior IFN-α therapy were associated with worse survival. The presence of a deletion of der(9) was not associated with an inferior estimated probability of survival (Figure 1A). In a multivariate Cox proportional hazard model, a higher platelet count (≥ 700 × 109/L) and the presence of peripheral blood blasts were the only variables associated with a significantly higher risk of death.
Kaplan-Meier estimates. Estimates of (A) overall survival grouped by deletion of der(9) (Del der(9)) and (B) remission duration grouped by deletion of der(9) among patients who achieved complete cytogenetic remission. Solid line indicates deletion; broken line indicates no deletion.
Kaplan-Meier estimates. Estimates of (A) overall survival grouped by deletion of der(9) (Del der(9)) and (B) remission duration grouped by deletion of der(9) among patients who achieved complete cytogenetic remission. Solid line indicates deletion; broken line indicates no deletion.
Duration of response
A total of 236 patients achieved a complete cytogenetic remission. The date of response was not available in 1 patient with deletion of der(9), rendering 235 patients available for the analysis of duration of response. Thirty-five (15%) patients had lost their response at the time of this analysis. The probability of a sustained complete cytogenetic remission at 3 years for all patients was 71% (95% CI 0.61-0.83). When patients were grouped according to their der(9) status, 4 (16%) patients with deletions lost their response compared with 31 (15%) without deletions (P = .75). Figure 1B shows the Kaplan-Meier estimates of time to loss of complete cytogenetic remission. The covariates associated with duration of complete cytogenetic remission in a univariate analysis were age, bone marrow blasts, and the Hasford risk group. In a multivariate analysis, patients 60 years of age and older and patients with 5% or more bone marrow blasts had a significantly higher risk of relapse (hazard ratios of 3.54 and 3.96, and P values of .001 and .005, respectively).
Discussion
Deletions of der(9) have been recognized in 9% to 15% of patients with CML in recent years.11-16,37 These deletions are usually large, involving several megabases, and are thought to occur at the time of the Philadelphia chromosome translocation rather than during disease progression.12,15 They are also more prevalent (40% to 50%) among patients with variant Philadelphia translocations.11,12,14 Several studies have suggested that deletions of der(9) have an adverse prognosis, and are associated with an inferior probability of survival and/or progression-free survival in CML.11,12,14 Most of these observations were before the imatinib mesylate era, in patients treated with hydroxyurea, IFN-α, or bone marrow transplantation. The impact of imatinib mesylate on outcome of patients with deletions of der(9) is not clearly established. In this study, we found that imatinib mesylate may overcome the adverse prognostic significance of del(9) deletions.
Two important methodologic aspects need to be considered when analyzing these results. First, the Vysis ES probe that can identify deletions of der(9) has been routinely used at our institution since May 2002. Thus, only 42% of the patients treated with imatinib mesylate at our institution were evaluable for the status of der(9) deletions. There were no differences in the clinical characteristics and response to imatinib mesylate between patients in whom this probe was used or not, suggesting that our study group was representative of the total population. Second, the Vysis ES probe system can detect the losses of genomic sequences of the chromosome 9 but not of chromosome 22. Therefore, the latter were not assessed in this study. Most instances of deletions involve der(9) alone or together with deletions of chromosome 22. Deletions of sequences only of chromosome 22 represent only approximately 5% to 10% of all deletions.14,16,37 It is unlikely that this small proportion of patients not detected in our series would significantly alter the results. In addition, deletions of chromosome 22 alone have not been implicated in adverse prognosis.
Deletions of der(9) were detected in 9% (95 CI 0.07, 0.13) of our patients, a proportion similar to that reported in the literature.11-14,16,37 Similar to recent reports,16 we did not observe significant differences in the clinical characteristics of patients with and without der(9) deletions. The response rates to imatinib mesylate were similar in patients with and without deletions, and within those reported in the literature.20,21,23,26,31,32,38 There was also no significant difference in the probabilities of survival and remission durations between the 2 groups (Figure 1). A recent report by Huntly et al16 suggested that patients with der(9) deletions had a significantly lower response rate than those without this abnormality, particularly among those who had failed prior IFN-α therapy. The rate of major cytogenetic remission in that report for patients in CP with deletions was 55% compared with 75% for patients without deletions (P = .008).16 Huntly et al16 also reported a significant difference in the rate of progression between the 2 groups, and a trend for inferior survival for patients with der(9) deletions. Considering that both series represent relatively small numbers of patients with deletions, and with a relatively short follow-up, the results of both series need to be considered cautiously. It is possible that longer follow-up will show that imatinib mesylate delays but does not prevent recurrence of the disease in patients with der(9) deletions. Another possible explanation for the disparity between the cytogenetic response rates in the present report and that of Huntly et al16 is that 36% of our patients were treated with high-dose imatinib mesylate (ie, 800 mg daily), and there were significantly more patients in chronic phase with deletions than without deletions treated with high-dose imatinib mesylate (58% vs 34%; P = .026). High-dose imatinib mesylate has been associated with improved cytogenetic and molecular response rates compared with standard dose in patients with CP both after IFN-α failure30 and those previously untreated.31 Thus, it is possible that higher doses of imatinib may be more effective in overcoming the adverse prognostic influence of der(9) deletions. In fact, it could be hypothesized that part of the benefit obtained from high-dose imatinib mesylate may derive from offsetting the negative effect of adverse prognostic features such as deletions of der(9). However, it is important to recognize that the possible effect of high-dose imatinib mesylate cannot be fully isolated in this cohort other than by a multivariate analysis. Thus, a prospective analysis of the prognostic significance of deletions of der(9) in patients treated in a uniform way is warranted.
Smaller deletions undetectable by FISH may be present in some patients. Kolomietz et al39 used real-time quantitative PCR to investigate these smaller deletions. Among 71 patients with poor outcome and without evidence of deletion of der(9) by FISH, 25 (35%) had microdeletions extending 120 kilobase (kb) from the 5′ end of the ABL gene in the centromeric direction on the derivative chromosome 9.39 Thus, deletions may be more prevalent than currently recognized, and the prognostic significance may vary when patients with microdeletions are included. Still, with complete cytogenetic response rates in excess of 90% with high-dose imatinib mesylate, it is unlikely that these changes will have a major impact, at least in the rate of response to imatinib.
In conclusion, der(9) deletions occur in a significant fraction of patients with CML. These patients have clinical characteristics similar to those of patients without the abnormality. In contrast to previous literature reports, there was no difference in response to imatinib mesylate or in overall outcome among patients treated with imatinib by the presence or absence of der(9) deletions. Although a larger number of patients with longer follow-up might be necessary for definitive conclusions, our data suggest that treatment with imatinib mesylate may overcome the adverse prognostic impact of der(9) deletions in patients with CML. Still, until the significance of this phenomenon is clearly established in a prospective analysis, it is important to continue monitoring patients for this abnormality.
J.C. is a Clinical Research Scholar for The Leukemia and Lymphoma Society.
Prepublished online as Blood First Edition Paper, November 30, 2004; DOI 10.1182/blood-2004-06-2208.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 U.S.C. section 1734.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal