Abstract
Regulatory CD25+CD4+ T cells (Treg cells) are a central element of peripheral tolerance. Little is known, however, about phenotypic and functional characteristics of these cells with regard to memory. In this study we show that the chemokine receptor CCR6 is expressed on a distinct subset of mouse Treg cells. Similar to their CD25- counterparts, CCR6+ Treg cells exhibit markers of activation, memory, and expansion that are indicative for an effector-memory function. They are memory-like cells, generated in vivo from CCR6-CD25+ T cells after the encounter of antigen. As conventional CD25- effector-memory T cells, they have a high turnover rate and, in contrast to CCR6- Treg cells, they respond rapidly to restimulation in vitro with up-regulation of interleukin 10. CCR6+ Treg cells are enriched in the peripheral blood and accumulate in the central nervous system after induction of experimental autoimmune encephalomyelitis (EAE). This subset therefore seems to represent a population of regulatory effector-memory T cells (TREM), destined to control potentially destructive immune responses directly in inflamed tissues. Importantly, these cells are also present in humans. Here the expression of CCR6 fully cosegregates with CD45RO, an established marker of human memory T cells.
Introduction
Regulatory T cells are the central element for the maintenance of peripheral tolerance.1-5 Upon activation, they switch into an active suppressor mode that allows them to neutralize or to inactivate other effector cells, such as B cells or T cells. Several types of regulatory T cells have been identified so far, of which most belong to the CD4+ lineage. Based on the expression of the interleukin 2 (IL-2) receptor-α chain (CD25), they can be subdivided into 2 major subsets, CD25-CD4+ T cells (Tr1)2 and CD25+CD4+ T cells (Treg cells).6 Whereas Tr1 cells seem to acquire their suppressor status in the periphery by polarization of naive T cells, Treg cells are described as “born” suppressors. Although some recent data indicate that at least to some extent Treg cells can derive also from the CD25-CD4+ T-cell subset,7 there is little doubt that regulatory CD25+CD4+ T cells are mainly produced intrathymically, where they are specifically trained for recognition of autoantigens.8,9
To carry out their suppressor function, regulatory T cells, as all other lymphocytes, have to migrate to lymphoid organs and to sites of inflammation. Homing and trafficking are facilitated by the expression of distinct sets of chemokine receptors10 of which 2, CCR8 and CCR4, have already been reported to be important for regulatory human CD25+CD4+ T cells.11 Although their expression is not exclusively restricted to regulatory cells,12 CCR4 and even more CCR8 are apparently expressed by a large fraction of regulatory CD25+ T cells. Another chemokine receptor that has not been considered yet is CCR6. The ligands, CCL20 and β-defensin, are produced mainly in inflamed sites and attract CCR6+ cells by inducing migration13,14 and attachment to endothelial cells.15 CCR6 is a marker of certain dendritic cell (DC), B-cell, and memory T-cell subsets13,16 and its expression on Langerhans cells and differentiated monocytes can be induced by IL-10.17 It is also present on the surface of “immature” DCs,18 known to induce tolerance,19 as well as on a subset of suppressive DCs that overexpress the enzyme indoleamine 2,3-dioxygenase (IDO).20
Importantly, CD4+ T cells express CCR6 only as antigen-experienced memory cells.13 In this study we show that CCR6 is present on a substantial fraction of regulatory CD25+CD4+ T cells. These cells exhibit a phenotype of activation, expansion, and memory typical for effector-memory T cells. Because they seem to control immune responses directly at inflamed sites, these regulatory effector/memory-like T cells appear to function as a natural counterbalance to “regular” effector-memory T cells.
Materials and methods
Antibodies and reagents
Fluorescein isothiocyanate (FITC)-, phycoerythrin (PE)-, or allophycocyanin (APC)-conjugated streptavidin, secondary antibodies, and isotype controls were purchased from BD PharMingen (San Diego, CA), R&D Systems (Minneapolis, MN), Coulter (Fullerton, CA), or Caltag (Burlingame, CA). αCD3, αCD4, αCD5, αCD8a, αCD11a, αCD11b, αCD25, αCD44, αCD45R, αCD54, αCD90.2, αCD103, αCD122, αCD152, αCCR5, αKi67, αT-cell receptor β (αTCR-β), and α 5-bromo-2-deoxyuridine (αBrdU) were purchased from BD PharMingen; αCD25, αCD45RB, αCD62L, and αCD69 were from Caltag; αCCR6 and α-glucocorticoid-induced tumor necrosis factor receptor (αGITR; polyclonal) were from R&D Systems; and αCD4, αCD25, αCCR6, and αCD45RO specific for human cells were from BD PharMingen. αCD3 (145-2C11, antimouse; T3D, antihuman), αCD25 (PC61), αCD90.2 (30-H12), and αCD62L (MEL-14) were produced and in some cases labeled at the Max-Delbrück-Center (MDC). CCL19-Fc was provided by J. G. Cyster (UCSF).21
Animals
Mice were kept under pathogen-free conditions according to the institutional, state, and federal guidelines. B10.PL, DO11.10, and TG4 were bred at the MDC animal facility; female BALB/c and SJL/J mice were purchased from Charles River Laboratories (Sulzfeld, Germany), Harlan Winkelmann (Borchen, Germany), or Taconic Farms (Rey, Denmark) and used at age 8 to 15 weeks.
Gene expression profiling
RNA was extracted by Trizol (Invitrogen, Carlsbad, CA) from magnetically activated cell sorting (MACS)-purified populations of CD25+CD4+ and CD25-CD4+ SJL/J lymph node cells. Double-stranded cDNA was prepared with a T7 promoter-tagged polyT primer from 1 μg total RNA. Biotin-labeled cRNA was generated using the ENZO kit (Affymetrix, Santa Clara, CA) of which 10 μg was hybridized to U74Av2 gene chips (Affymetrix). Hybridization, staining, scanning, and data acquisition were carried out according to manufacturer's recommendation at the MDC gene array facility. Data were analyzed using Microarray suite (Affymetrix) and GeneSpring software (Silicon Genetics, Redwood City, CA).
Flow cytometry and cell preparation
Fluorescence-activated cell sorting (FACS) analysis was carried out on an FACSCalibur instrument (BD Bioscience, San Jose, CA). For intracellular staining, cells were fixed in 2% paraformaldehyde/phosphate-buffered saline (PBS) and permeabilized with 0.5% saponin before staining. FACS sorting was carried out on a MoFlo (Dako Cytomation, Carpinteria, CA) or FACSVantage instrument (BD Bioscience) at the Santa Lucia Foundation or at the Deutsche Rheumaforschungsinstitut (DRFZ)-Berlin. Prior to the sorting, cells were enriched for CD4+ or CD25+ T cells by the MACS procedure (Miltenyi Biotech, Bergisch Gladbach, Germany) and dead cells were excluded by staining with propidium iodide. Purity of sorted cells was always above 90%, data were analyzed using CellQuest (BD Bioscience) and Flowjo software (Tree Star, San Carlos, CA). Depending on the experiment, between 1 × 104 and 5 × 106 cells were analyzed. Human peripheral blood mononuclear cells (PBMCs) were obtained from healthy volunteers and mononuclear cells were isolated by Ficoll gradient centrifugation (Pharmacia, Uppsala, Sweden). Approval was obtained from the MDC (Berlin, Germany) and the IRCCS Santa Lucia (Rome, Italy) institutional review boards for these studies. Informed consent was provided according to the Declaration of Helsinki.
Suppression, proliferation, and recall assays
In vitro suppression assays with mouse cells were carried out in RPMI/10% fetal calf serum (FCS) in 96-well V-bottom plates (Costar, Bodenstein, Germany) with 2.5 × 104 CD4+ responder cells, titrated amounts of suppressor cells, and 5 × 104 irradiated (3000 rad) αCD90.2 T cell-depleted splenocytes in the presence of 0.5 to 1 μg/mL soluble αCD3 (145-2C11). After 72 hours at 37°C, 1 μCi/well (0.037 MBq) 3H-thymidine was added for additional 6 to 12 hours. For suppression assays with human T cells, antigen-presenting cells (APCs) were depleted with αCD3 (T3D) and stimulation was carried out with 10 μg/mL soluble αCD3. Proliferation assays with central nervous system (CNS) infiltrates of SJL mice were carried out in U-bottom plates with 105 radiated splenocytes and 5 × 104 CNS-infiltrating cells in the presence of 10 μg/mL soluble αCD3. Then, 5 μg/mL polyclonal αGITR was added to abrogate suppression. Proliferation was determined using a β-plate reader (Wallac, Turku, Findland). For in vitro recall experiments, cell populations (5 × 104) obtained by FACS were stimulated for 4 hours at 37°C in U-bottom plates coated with 20 μg/mL αCD3. Expression of IL-10 was determined here by real-time reverse transcription-polymerase chain reaction (RT-PCR). Assays were performed as duplicates or triplicates.
Migration assays
In vitro migration assays were carried out as described.14 Briefly, 0.5 × 106 CD4+ or CD25+ cells were added to the upper chamber (3-μm pore size tissue culture inserts, Costar or BD Falcon, Bedford, MA); the lower chamber was loaded with RPMI/0.5% bovine serum albumin (BSA) containing 1 μg/mL CCL4 or CCL20 (R&D Systems, Minneapolis, MN; PreproTech, Rocky Hill, NJ; or Biosource, Camarillo, CA). After 3 hours at 37°C a fixed amount of Calibrite beads (BD PharMingen) was added as internal reference to the lower chamber and cell numbers were determined by FACS analysis. Chemotactic index represents the ratio of cells migrated in the presence of chemokines to the cells migrated spontaneously with medium alone. Assays were performed as duplicates.
Real-time RT-PCR
RNA was extracted from FACS-sorted populations with Trizol (Invitrogen, Karlsruhe, Germany) according to the manufacturer's recommendations. cDNA was prepared with Superscipt II reverse transcriptase (Invitrogen) using an oligo dT primer. The following specific primers were used: FoxP3 forward: 5′-ACCACCTTCTGCTGCCACTG-3′; FoxP3 reverse: 5′-TGCTGTCTTTCCTGGGTGTACC-3′; HPRT forward: 5′-TGACACTGGCAAAACAATGCA-3′; HPRT reverse: 5′-GGTCCTTTTCACCAGCAAGCT-3′, IL-10 forward: 5′-TGGCATGAGGATCAGCAGGG-3′, IL-10 reverse: 5′-GGCAGTCCGCAGCTCTAGG-3′. PCR was carried out with a QuantiTect SYBR Green PCR kit (Qiagen, Hilden, Germany) with an iCycler instrument (Bio-Rad, Hercules, CA) and was performed in duplicates or triplicates.
EAE induction and preparation of CNS infiltrates
Experimental autoimmune encephalomyelitis (EAE) was induced by immunizing female SJL mice subcutaneously with 50 μg PLP 139-151 peptide in complete Freund adjuvant, containing 400 μg Mycobacterium tuberculosis H37Ra (Difco, Detroit, MI) followed by intravenous injection of 200 ng Pertussis toxin on day 1. Mice were scored daily for clinical signs: 0, no clinical sign; 1, limp tail; 2, limp tail, impaired righting reflex, and paresis of one limb; 3, hind limb paralysis; 4, hind limb and forelimb paralysis; 5, moribund. For the isolation of CNS-infiltrating cells, mice were anesthetized by intraperitoneal injection with ketamine (50 mg/kg body weight) and xylazine (10 mg/kg body weight) and perfused intracardially through the left ventricle with 30 mL ice-cold PBS. Cells were purified by a Percoll density gradient (30:60) after digestion of the homogenized brain with 0.5 mg/mL collagenase type VIII (Sigma, St Louis, MO).
Adoptive transfer and CFDA labeling
Lymph node and spleen cells from TCR-transgenic TG422 or DO11.10 mice23 were pooled. CD4+CCR6- T cells were isolated by the MACS procedure first using a CD4 T-cell isolation kit (Miltenyi Biotech), followed by MACS depletion of CCR6+ cells and labeled according to manufacturer's recommendation with 3 μM carboxyfluorescein diacetate succinimidyl ester (CFDA-SE; Molecular Probes, Eugene, OR). In brief, 2 × 107 cells were resuspended in 2 mL PBS/0.05% FCS/3 μM CFDA and incubated for 8 minutes at room temperature. Labeling was stopped by washing cells 3 times with RPMI/10% FCS. Recipient mice (B10.PL or BALB/c) received 1 × 107 cells by intravenous injection and were primed on the same day by subcutaneous injection of peptide (20 μg MBP Ac1-11 or 100 μg OVA323-339) emulsified in complete Freund adjuvant.
BrdU labeling
BrdU (Sigma) was supplied by the drinking water at a concentration of 0.8 mg/mL. After 7 or 14 days cells were isolated, stained with antibodies for cell surface markers, fixed overnight in 1% paraformaldehyde/PBS, and permeabilized for 30 minutes at 4°C in 0.5% saponin. Cells were incubated at room temperature for 30 minutes in 0.15 M NaCl, 4.2 mM MgCl2, 10 mM HCl, pH 5 in the presence of 2 U DNase I (Invitrogen), followed by staining with αBrdU for 30 minutes and were finally analyzed by FACS analysis.
Results
CCR6 expression of CD25+CD4+ T cells
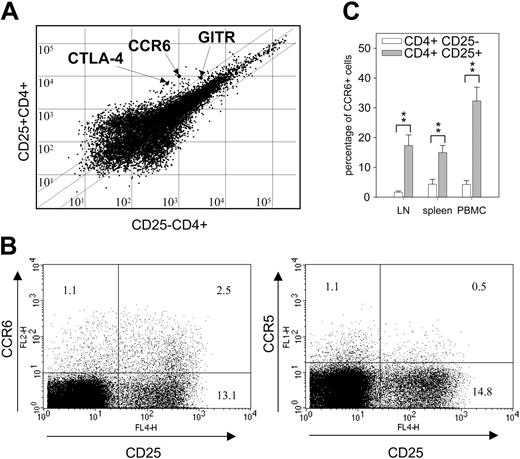
Gene array analysis of mouse CD25+CD4+ T cells indicated that mRNA encoding for CCR6 was significantly more abundant in samples from CD25+CD4+ T cells than in samples of CD25-CD4+ T cells (Figure 1A). The relative increase was about 10-fold, which was well within the range of other genes typically associated with regulatory T cells, such as cytotoxic T-lymphocyte antigen 4 (CTLA-4) and GITR. FACS analysis of lymphocytes revealed that CCR6+ cells are, in fact, much more frequent among CD25+CD4+ T cells (Figure 1B left panel). In comparison, CCR5, a chemokine receptor previously described to be a characteristic marker of these cells,24 is present apparently only on a rather small number of CD25+ T cells (Figure 1B right panel).
CCR6 expression of CD25+CD4+ T cells. (A) Gene array analysis of CD25+CD4+ and CD25-CD4+ lymph node cells. mRNA expression levels are shown for preparations derived from CD4+CD25- and CD4+CD25+ lymphocyte populations (via MACS) isolated from SJL/J mice. Diagonal lines indicate 3-fold overexpression; dots representing CTLA-4, GITR, and CCR6 are indicated by arrows. (B) Comparison of CCR5 and CCR6 expression on CD4+ lymph node cells. Cells from lymph nodes of naive BALB/c mice were triple-stained with antibodies directed against CD4, CD25, and either CCR6 (left panel) or CCR5 (right panel) and analyzed by FACS. The dot plots represent cells gated on CD4 expression. The numbers in each quadrant indicate the percentage of cells within the CD4+ population. One of 3 independent experiments with cells pooled from 2 to 5 animals is shown. (C) Relative fraction of CCR6+CD4+ T cells in lymph nodes, spleens, and PBMCs. Percentage of cells was determined by FACS analysis with cells from naive mice as described for Figure 1B. □ represents the percentage of CCR6+ cells within the population of CD4+CD25- T cells; ▦, their fraction within the population of CD4+CD25+ T cells. Plot shows mean values from 7 to 9 independent experiments, P values are represented by asterisks (**P < .01) and were calculated according to the Student t test.
CCR6 expression of CD25+CD4+ T cells. (A) Gene array analysis of CD25+CD4+ and CD25-CD4+ lymph node cells. mRNA expression levels are shown for preparations derived from CD4+CD25- and CD4+CD25+ lymphocyte populations (via MACS) isolated from SJL/J mice. Diagonal lines indicate 3-fold overexpression; dots representing CTLA-4, GITR, and CCR6 are indicated by arrows. (B) Comparison of CCR5 and CCR6 expression on CD4+ lymph node cells. Cells from lymph nodes of naive BALB/c mice were triple-stained with antibodies directed against CD4, CD25, and either CCR6 (left panel) or CCR5 (right panel) and analyzed by FACS. The dot plots represent cells gated on CD4 expression. The numbers in each quadrant indicate the percentage of cells within the CD4+ population. One of 3 independent experiments with cells pooled from 2 to 5 animals is shown. (C) Relative fraction of CCR6+CD4+ T cells in lymph nodes, spleens, and PBMCs. Percentage of cells was determined by FACS analysis with cells from naive mice as described for Figure 1B. □ represents the percentage of CCR6+ cells within the population of CD4+CD25- T cells; ▦, their fraction within the population of CD4+CD25+ T cells. Plot shows mean values from 7 to 9 independent experiments, P values are represented by asterisks (**P < .01) and were calculated according to the Student t test.
The difference in the frequency of CCR6+ cells was particularly evident when comparing the fraction of CCR6+ cells within the CD25- and the CD25+ T-cell population in the different tissues (Figure 1C). In lymph nodes less than 2% and in spleen and peripheral blood less than 5% of the CD25-CD4+ T cells were CCR6+. Much higher numbers were determined for CD25+CD4+ T cells. Here, 18% of the lymph node cells, 15% of the splenocytes, and 32% of the blood cells expressed the CCR6 receptor.
CCR6+CD25+ T cells display phenotype and function of Treg cells
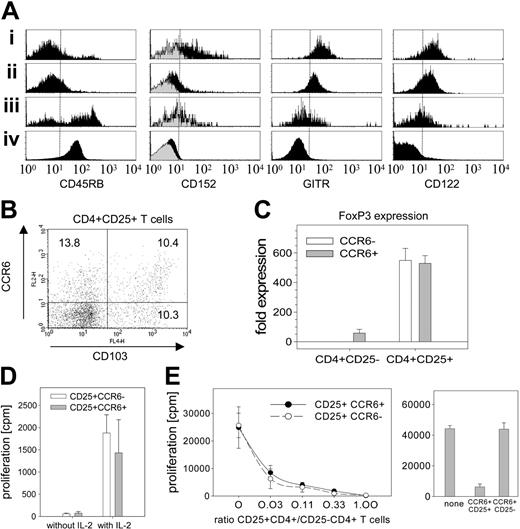
To ensure that the CCR6+CD25+ T cells are in fact Treg cells, FACS analysis was carried out with antibodies directed against markers associated with Treg cells (Figure 2A). In line with the published data, both the CCR6-CD25+ and CCR6+CD25+ T-cell subsets express low levels of CD45RB25 and show elevated expression levels of CD152 (CTLA-4),1,3,4 GITR,26,27 and CD122. The brighter staining of the latter 3 markers, however, was detected on CCR6+CD25+ cells. Some overlap of CCR6 expression was also detected for αEβ7 integrin (CD103),27,28 a marker that had recently been associated with Treg cells with effector/memory-like phenotype.29 Although the 2 markers did not completely cosegregate (Figure 2B), almost half of the cells in the CCR6+ subset coexpressed CD103, whereas approximately 15% of the CCR6- T cells were positive for this marker.
CCR6+CD25+CD4+ cells exhibit phenotypic and functional characteristics of Treg cells. (A) FACS analysis of markers characteristic for Treg cells. Four-color staining was carried out with lymph node cells from naive BALB/c mice. Cells were stained with antibodies specific for CD4, CD25, and CCR6 together with antibodies specific for either CD45RB, CD152, GITR, or CD122. Histograms are shown for the 4 CD4+ T-cell subsets CD25+CCR6+ (i), CD25+CCR6- (ii), CD25-CCR6+ (iii), and CD25-CCR6- (iv). Plots are generated by gating on the respective markers. Staining of CD152 was carried out intracellularly; gray areas represent here the isotype control. Vertical lines are inserted as reference for relative shifts. (B) Expression of CD103 and CCR6 on the CD25+CD4+ T-cell subsets. The dot plot shows the staining CD103 versus CCR6 for the population of lymph node cells gated on CD25+CD4+ cells. Numbers in each quadrant indicate the percentage fraction of the CD25+CD4+ T-cell population. Plots in panels A and B are representative for 3 independent experiments with cells pooled from 2 to 5 animals. (C) Expression of FoxP3. CD25-CCR6-, CD25-CCR6+, CD25+CCR6-, and CD25+CCR6+ lymph node cells were isolated by FACS and expression levels of FoxP3 were determined by real-time RT-PCR. CCR6- cells are represented by □, CCR6+ cells by ▦. Expression was determined in reference to HPRT and expression levels of FoxP3 are shown as fold increase compared to CD25-CCR6- T cells. The plot represents one of 4 independent experiments each with cells pooled from 8 to 10 mice. (D) Proliferative in vitro response of CCR6+CD25+ T cells. CCR6+CD25+ (▦) and CCR6-CD25+ CD4+ T cells (□) were stimulated in vitro with anti-CD3 and radiated APCs in the absence or presence of 20 U/mL IL-2. Proliferation was determined with 3H-thymidine. One of 2 independent experiments with cells pooled from each of 10 mice is shown. (E) Suppressive capacity. The ability to suppress proliferation of CD25-CD4+ splenocytes was tested with FACS populations of CD25+CD4+ lymph node cells differing in their CCR6 expression (left panel) and with CCR6+CD4+ lymph node cells differing in CD25 expression (right panel). CD25-CD4+ splenocytes were incubated in the presence of anti-CD3 and radiated APCs with titrated amounts of CCR6-CD25+CD4+ T cells (○ and dashed line) or CCR6+CD25+CD4+ T cells (• and solid line). Proliferation was determined with 3H-thymidine. The x-axis of the line plot indicates the ratio of CD25+CD4+ regulatory cells to CD25-CD4+ cells. Bars of the bar chart represent proliferation of CD25-CD4+ splenocytes alone and of CD25-CD4+ splenocytes incubated with CCR6+CD25+ or with CCR6+CD25- T cells at a ratio of 0.33. One of 3 independent experiments each with cells pooled from 8 to 10 mice is shown.
CCR6+CD25+CD4+ cells exhibit phenotypic and functional characteristics of Treg cells. (A) FACS analysis of markers characteristic for Treg cells. Four-color staining was carried out with lymph node cells from naive BALB/c mice. Cells were stained with antibodies specific for CD4, CD25, and CCR6 together with antibodies specific for either CD45RB, CD152, GITR, or CD122. Histograms are shown for the 4 CD4+ T-cell subsets CD25+CCR6+ (i), CD25+CCR6- (ii), CD25-CCR6+ (iii), and CD25-CCR6- (iv). Plots are generated by gating on the respective markers. Staining of CD152 was carried out intracellularly; gray areas represent here the isotype control. Vertical lines are inserted as reference for relative shifts. (B) Expression of CD103 and CCR6 on the CD25+CD4+ T-cell subsets. The dot plot shows the staining CD103 versus CCR6 for the population of lymph node cells gated on CD25+CD4+ cells. Numbers in each quadrant indicate the percentage fraction of the CD25+CD4+ T-cell population. Plots in panels A and B are representative for 3 independent experiments with cells pooled from 2 to 5 animals. (C) Expression of FoxP3. CD25-CCR6-, CD25-CCR6+, CD25+CCR6-, and CD25+CCR6+ lymph node cells were isolated by FACS and expression levels of FoxP3 were determined by real-time RT-PCR. CCR6- cells are represented by □, CCR6+ cells by ▦. Expression was determined in reference to HPRT and expression levels of FoxP3 are shown as fold increase compared to CD25-CCR6- T cells. The plot represents one of 4 independent experiments each with cells pooled from 8 to 10 mice. (D) Proliferative in vitro response of CCR6+CD25+ T cells. CCR6+CD25+ (▦) and CCR6-CD25+ CD4+ T cells (□) were stimulated in vitro with anti-CD3 and radiated APCs in the absence or presence of 20 U/mL IL-2. Proliferation was determined with 3H-thymidine. One of 2 independent experiments with cells pooled from each of 10 mice is shown. (E) Suppressive capacity. The ability to suppress proliferation of CD25-CD4+ splenocytes was tested with FACS populations of CD25+CD4+ lymph node cells differing in their CCR6 expression (left panel) and with CCR6+CD4+ lymph node cells differing in CD25 expression (right panel). CD25-CD4+ splenocytes were incubated in the presence of anti-CD3 and radiated APCs with titrated amounts of CCR6-CD25+CD4+ T cells (○ and dashed line) or CCR6+CD25+CD4+ T cells (• and solid line). Proliferation was determined with 3H-thymidine. The x-axis of the line plot indicates the ratio of CD25+CD4+ regulatory cells to CD25-CD4+ cells. Bars of the bar chart represent proliferation of CD25-CD4+ splenocytes alone and of CD25-CD4+ splenocytes incubated with CCR6+CD25+ or with CCR6+CD25- T cells at a ratio of 0.33. One of 3 independent experiments each with cells pooled from 8 to 10 mice is shown.
Importantly, CCR6+CD25+ T cells also expressed FoxP3 (Figure 2C). FoxP3 is a key transcription factor of regulatory T cells30-32 and was detected in comparable levels in CD25+CCR6+ and in CD25+CCR6- T cells. Moreover, both CD25+ subsets showed an anergic response when stimulated in vitro with αCD3 antibodies (Figure 2D). The effect was abrogated when stimulated in the presence of high doses of IL-2 (Figure 2D), which again is characteristic for Treg cells.
Finally, both CCR6- and CCR6+ CD25+ T cells were able to inhibit proliferation of CD4+ effector cells (Figure 2E left panel). Whereas no suppression was detected with CCR6+CD25- T cells (Figure 2E right panel), the CCR6+CD25+ T cells were at least equally effective as their CCR6- counterparts. Thus, CCR6+CD25+ T cells clearly represent a subpopulation of Treg cells.
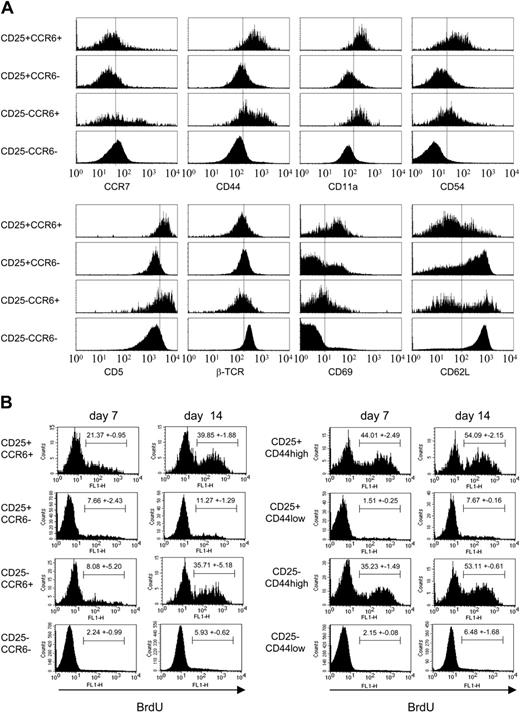
CCR6+ Treg cells exhibit the phenotype of activated effector-memory cells
To further characterize the CCR6+ Treg subset, FACS analysis was extended to established markers of activation and memory (Figure 3A). Staining of CCR7 with a CCL19-Fc fusion protein21 revealed that both CCR6-CD25+ and CCR6+CD25+ T cells expressed low levels of CCR7. In contrast to CCR7, the expression pattern of several other markers clearly segregated with CCR6. Memory cells are typically CD44high,33 as were both CD25-CCR6+ and CD25+CCR6+ cells, whereas the respective CCR6- populations were CD44low. The same pattern was also detected for 2 other activation markers, CD11a (lymphocyte function-associated antigen 1 [LFA-1]) and CD54 (intercellular adhesion molecule 1 [ICAM-1]).34 Both CCR6+ populations were CD11ahigh and CD54high, whereas the 2 CCR6- subsets expressed only low levels.
CCR6+ Treg cells exhibit the phenotype of effector-memory T cells and have a high turnover rate in vivo. (A) Phenotypic characterization. Lymph node cells of naive mice were stained with αCD4, αCD25, and αCCR6 together with antibodies or fusion proteins, directed either against CCR7, CD44, CD11a, CD54, CD5, βTCR, CD69, or CD62L. Histograms are shown for the 4 subsets of CD25+CCR6+, CD25+CCR6-, CD25-CCR6+, and CD25-CCR6-CD4+ T cells and were generated by gating on the respective markers. Staining for CCR7 was carried out using a CCL19-Ig-fusion protein. Vertical bars are inserted as reference for relative shifts. One of 4 independent experiments each with cells pooled from 2 to 6 animals is shown. (B) In vivo turnover rate. FACS analysis of lymph node cells is shown for populations stained with αCCR6 (left panels) or αCD44 (right panels). Proliferating cells were labeled by providing BrdU with the drinking water for a period of 7 days (left columns) or 14 days (right columns). Cells were analyzed by FACS immediately after this period. Histograms of the BrdU-specific staining shown are gated on CD4+ cells. The percentages of BrdU+ cells are indicated. One of 2 independent experiments is shown.
CCR6+ Treg cells exhibit the phenotype of effector-memory T cells and have a high turnover rate in vivo. (A) Phenotypic characterization. Lymph node cells of naive mice were stained with αCD4, αCD25, and αCCR6 together with antibodies or fusion proteins, directed either against CCR7, CD44, CD11a, CD54, CD5, βTCR, CD69, or CD62L. Histograms are shown for the 4 subsets of CD25+CCR6+, CD25+CCR6-, CD25-CCR6+, and CD25-CCR6-CD4+ T cells and were generated by gating on the respective markers. Staining for CCR7 was carried out using a CCL19-Ig-fusion protein. Vertical bars are inserted as reference for relative shifts. One of 4 independent experiments each with cells pooled from 2 to 6 animals is shown. (B) In vivo turnover rate. FACS analysis of lymph node cells is shown for populations stained with αCCR6 (left panels) or αCD44 (right panels). Proliferating cells were labeled by providing BrdU with the drinking water for a period of 7 days (left columns) or 14 days (right columns). Cells were analyzed by FACS immediately after this period. Histograms of the BrdU-specific staining shown are gated on CD4+ cells. The percentages of BrdU+ cells are indicated. One of 2 independent experiments is shown.
CCR6 expression also correlated with CD5, a negative regulator for TCR signaling35 that is up-regulated on TCR ligation.36 TCR-mediated activation of CCR6+ cells was further supported by slightly reduced expression levels of βTCR and, even more, by the expression patterns of CD69 and CD62L (L-selectin). Both markers are known to change their expression levels on TCR activation, which leads to up-regulation of CD69 and down-regulation of CD62L.33 Segregation with CCR6 was only partial but, nevertheless, most of the CCR6+CD25+ T cells clearly express high levels of CD69 and low levels of CD62L.
Rapid turnover of CCR6+ Treg cells in vivo
Although the phenotypic characterization of CCR6+CD25+ T cells revealed an expression pattern typical for antigen-experienced memory cells, a recent study could show that in particular CD4+ effector-memory T cells are characterized by a very rapid turnover rate.37 FACS analysis with anti-Ki67, a common marker of proliferation,38 indicated that in fact a relatively high fraction of CCR6+CD25+ T cells expressed this marker (on the Blood website, see the Supplemental Figure S1 link at the top of the online article). Proliferation of CD44high Treg cells was reported before39 and according to this study is driven by antigen recognition. To investigate whether a correlation between CCR6 expression and proliferation exists, experiments were therefore carried out in which BrdU was provided with the drinking water for a period of 7 or 14 days. After that labeling period lymph node cells were isolated and analyzed by FACS with BrdU-specific antibodies to discriminate the cycling cells from the noncycling cells (Figure 3B). The staining revealed that, in fact, a large fraction of the CCR6+ T cells incorporated BrdU, whereas only few of the CCR6- cells stained positive for this marker (Figure 3B left panel). After a 14-day labeling period almost 40% of the CCR6+ T cells were BrdU+, which applied for both the CCR6+CD25+ and the CCR6+CD25- T-cell subset. In principle it could not be excluded that some of the proliferating cells were activated non-Treg cells. A similar result, however, was also observed when using the previously published marker CD44,39 except that BrdU expression appeared faster (Figure 3B right panel). After a labeling period of 7 instead of 14 days less than half of the CD44+BrdU+ cells expressed already CCR6+, indicating a delayed expression of the chemokine receptor.
CCR6+ Treg cells are generated in vivo after antigen-specific activation
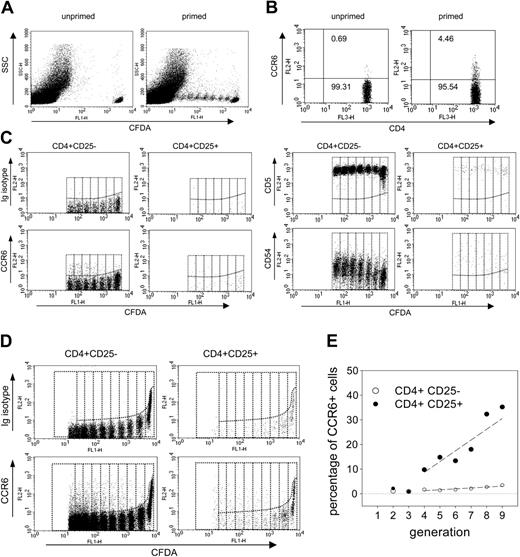
Even prolonged stimulation with anti-CD3 in the presence of IL-2 did not lead to any detectable increase in the number of CCR6+ cells (data not shown), an observation in line with published results obtained for human PBMCs.13 To determine, however, if CCR6+ Treg cells are generated in vivo on antigenic stimulation of CCR6-CD25+ T cells, adoptive transfer experiments were carried out with CFDA-labeled T cells derived from TCR-transgenic mice (Figure 4). TG4 mice22 express a TCR specific for the MBP Ac1-11 peptide. After depletion of CCR6+ cells by MACS the subset of CD4+CCR6- TG4 T cells was transferred to syngenic B10.PL hosts and the mice were primed with the MBP Ac1-11 peptide. Nine days later lymph node cells were isolated and analyzed by FACS.
CCR6+CD25+ T cells are generated in vivo after activation of CCR6-CD4+ T cells. FACS analysis is shown for CFDA-labeled CD4+ T cells. CD4+ T cells were isolated from TCR transgenic mice and depleted of CCR6+ cells by MACS. The CCR6-CD4+ cells were then labeled with CFDA and adoptively transferred into syngenic hosts. Two different model systems were used, based either on the recognition of MBP Ac1-11 (donor, TG4; recipient, B10.PL; A-C) or of OVA323-339 (donor, DO11.10; recipient, BALB/c; D-E). T cells were activated by priming with the respective peptide antigen and lymph node cells were analyzed 9 days later by FACS. (A) Antigen-specific induction of proliferation by TG4 T cells. Dot plots of the CFDA staining versus side scatter (SSC) are shown for lymph node cells of B10.PL mice that received CFDA-labeled CCR6-CD4+ T cells from TG4 mice. The cells were analyzed 9 days after transfer and derived either from primed mice (right panel) or from unprimed control mice (left panel). (B) Induction of CCR6 expression. Dot plots are gated on CD4+ cells and exclude all CFDA- cells so that they represent only transferred TG4 T cells. Staining of CD4 versus CCR6 is shown for cells isolated on day 9 from primed mice (right panel) or from nonprimed control mice (left panel). Numbers represent the percentages of CCR6+ and CCR6- cells of the respective populations. (C) Delayed expression of CCR6. Lymph node cells isolated on day 9 from peptide primed mice were stained with αCD4, αCD25, and αCCR6. The dot plots show CFDA+ CD4+ cells after staining with an isotype control or antibodies specific for CCR6, CD5, or CD54. Staining is shown for the population gated on CD4+CD25- (left panels) and CD4+CD25+ (right panels). Vertical lines separate daughter generations of dividing cells. One of 4 independent experiments is shown. (D) Induction of CCR6 expression in adoptively transferred DO11.10 T cells. Cells were isolated 9 days after the priming of BALB/c mice that previously received CFDA-labeled CCR6-CD4+ T cells from DO11.10. Staining is shown for CFDA versus isotype control (upper panels) or CCR6 (lower panels). Dot plots represent the CFDA+ populations gated on CD25-CD4+ cells (left panels) and on CD25+CD4+ cells (right panels). (E) Fraction of CCR6+ cells in dividing T cells after in vivo priming. The plot represents the relative fraction of CCR6+ T cells in the daughter generations of dividing CD25-CD4+ T cells (○) and CD25+CD4+ T cells (•). The plot is generated from the data shown in panel D; dashed lines represent trend lines. One of 2 independent experiments is shown. More than 106 CD4+ T cells were analyzed in each experiment.
CCR6+CD25+ T cells are generated in vivo after activation of CCR6-CD4+ T cells. FACS analysis is shown for CFDA-labeled CD4+ T cells. CD4+ T cells were isolated from TCR transgenic mice and depleted of CCR6+ cells by MACS. The CCR6-CD4+ cells were then labeled with CFDA and adoptively transferred into syngenic hosts. Two different model systems were used, based either on the recognition of MBP Ac1-11 (donor, TG4; recipient, B10.PL; A-C) or of OVA323-339 (donor, DO11.10; recipient, BALB/c; D-E). T cells were activated by priming with the respective peptide antigen and lymph node cells were analyzed 9 days later by FACS. (A) Antigen-specific induction of proliferation by TG4 T cells. Dot plots of the CFDA staining versus side scatter (SSC) are shown for lymph node cells of B10.PL mice that received CFDA-labeled CCR6-CD4+ T cells from TG4 mice. The cells were analyzed 9 days after transfer and derived either from primed mice (right panel) or from unprimed control mice (left panel). (B) Induction of CCR6 expression. Dot plots are gated on CD4+ cells and exclude all CFDA- cells so that they represent only transferred TG4 T cells. Staining of CD4 versus CCR6 is shown for cells isolated on day 9 from primed mice (right panel) or from nonprimed control mice (left panel). Numbers represent the percentages of CCR6+ and CCR6- cells of the respective populations. (C) Delayed expression of CCR6. Lymph node cells isolated on day 9 from peptide primed mice were stained with αCD4, αCD25, and αCCR6. The dot plots show CFDA+ CD4+ cells after staining with an isotype control or antibodies specific for CCR6, CD5, or CD54. Staining is shown for the population gated on CD4+CD25- (left panels) and CD4+CD25+ (right panels). Vertical lines separate daughter generations of dividing cells. One of 4 independent experiments is shown. (D) Induction of CCR6 expression in adoptively transferred DO11.10 T cells. Cells were isolated 9 days after the priming of BALB/c mice that previously received CFDA-labeled CCR6-CD4+ T cells from DO11.10. Staining is shown for CFDA versus isotype control (upper panels) or CCR6 (lower panels). Dot plots represent the CFDA+ populations gated on CD25-CD4+ cells (left panels) and on CD25+CD4+ cells (right panels). (E) Fraction of CCR6+ cells in dividing T cells after in vivo priming. The plot represents the relative fraction of CCR6+ T cells in the daughter generations of dividing CD25-CD4+ T cells (○) and CD25+CD4+ T cells (•). The plot is generated from the data shown in panel D; dashed lines represent trend lines. One of 2 independent experiments is shown. More than 106 CD4+ T cells were analyzed in each experiment.
As expected, proliferation of TG4 T cells was observed only when the mice were primed with the peptide antigen (Figure 4A). More importantly, also up-regulation of CCR6 was evident only after antigenic stimulation (Figure 4B). CCR6 expression was restricted, however, to a small subset, because only about 5% of the CFDA+CD4+ T cells stained positive for this marker. A more detailed analysis revealed that CCR6 expression is not immediately evident but required several cell divisions (Figure 4C). This applied for both CD25+ as well as CD25- T cells, although CCR6 induction appeared to be more efficient for CD25+ cells.
Up-regulation was also determined for 2 other markers associated with the effector-memory phenotype of CCR6+CD25+ T cells, CD5 and CD54 (Figure 4C). Of these only CD5 up-regulation was immediate and completely independent of cell divisions, whereas CD54 expression gradually increased with each cell division. In both cases, the expression levels were higher on CD25+ than on CD25- cells, an observation in line with the surface phenotype of CCR6+CD25+ T cells determined for lymph node cells of naive mice (compare Figure 3A). Timing of induction of the 3 markers, however, was very similar on CD25- and CD25+ T cells, suggesting that the transition into memory cells seems to follow similar rules both for regulatory and effector T cells.
Because TG4 mice contain relatively small numbers of CD25+ Treg cells (data not shown), we performed another transfer experiment in which we used DO11.10 mice as donors for the CCR6-CD4+ T-cell subset. DO11.10 mice are of BALB/c background and express a transgenic TCR specific for OVA323-339 (Figure 4D-E). Nine days after priming a similar pattern emerged as described for TG4 (Figure 4D). Up-regulation of CCR6 was observed after several rounds of cell division, both in the CD25- and the CD25+ T-cell subset. The larger number of CD25+ T cells, however, allowed us to determine more precisely the relative fraction of these cells within the daughter generations (Figure 4E). For CD25+ T cells the first significant increase was evident after 3 rounds of division and steadily increased to reach about 30% in the ninth generation. In comparison, the number of CCR6+ cells detectable among the CD25- population was much lower and did not reach more than 5%.
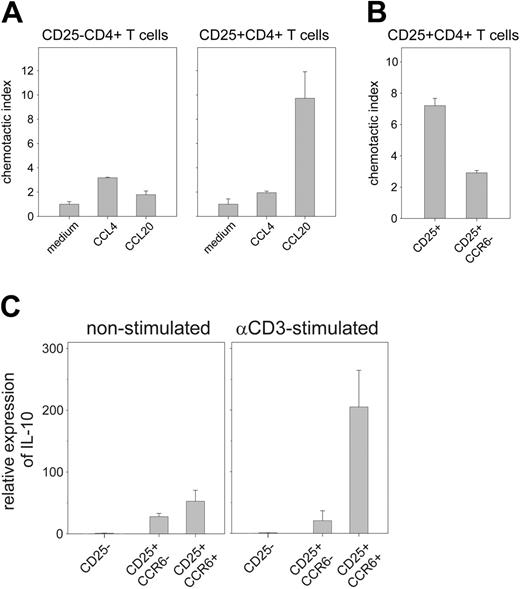
CCR6+ Treg cells respond to the chemokine CCL20 and produce IL-10 after restimulation in vitro
To determine the functional properties of the CCR6+ Treg subset, the cells were analyzed first with regard to their migratory capacity toward the CCR6 ligand CCL20 (Figure 5A). As control, migration was also determined for the CCR5 ligand CCL4, previously reported to be a major attractant of regulatory CD25+ T cells.24 With CD25-CD4+ lymph node cells only marginal increases of migration were detected for both chemokines. In contrast, CD25+CD4+ T cells were very efficiently mobilized by CCL20, producing an index of almost 10. Depletion of CCR6+ cells from the CD25+CD4+ population resulted in a significant decrease of the index, confirming that, in fact, CCR6+CD25+ cells were migrating (Figure 5B). In line with the low number of CCR5+ cells detected within the CD25+ population (compare Figure 1B right panel) and in accordance with other publications29,40 the chemotactic response of CD25+CD4+ T cells to CCL4 was in fact rather weak (Figure 5A right panel).
Functional characterization of CCR6+ Treg cells. (A) Chemotactic response of CD25-CD4+ and CD25+CD4+ T cells to CCL20. The chemotactic response of sorted populations of CD25-CD4+ (left panel) and CD25+CD4+ lymph node cells (right panel) was tested in a migration assay. The cells were incubated with either medium alone, with 1 μg/mL of the CCR5 ligand CCL4, or with1 μg/mL of the CCR6 ligand CCL20. After 3 hours the number of migrated cells was determined by FACS analysis. Migration is expressed as chemotactic index and was calculated by the ratio of cells, migrated in the presence of chemokine, to the number of cells that spontaneously migrated with medium alone. One of 3 independent experiments is shown. (B) Depletion of CCR6+ cells abrogates CCL20-induced migration of CD25+CD4+ T cells. The experiment was carried out as described for panel A, except that populations of CD25+CD4+ splenocytes were used, in which the CCR6+ subset was either still present or had been removed prior to the experiment by MACS. (C) CCR6+CD25+ T cells up-regulate IL-10 expression on restimulation in vitro. Using FACS-sorted cells, RNA from CD25+CCR6+, CD25+CCR6-, and as control of CD25-CD4+ T cells was analyzed for IL-10 expression by real-time RT-PCR. RNA was prepared either from freshly isolated cells (left panel) or after stimulation for 4 hours with plate-bound αCD3 (right panel). The relative expression is shown in reference to the IL-10 mRNA level of CD25- control cells. One of 4 independent experiments is shown each with pooled RNA from 8 to 10 animals.
Functional characterization of CCR6+ Treg cells. (A) Chemotactic response of CD25-CD4+ and CD25+CD4+ T cells to CCL20. The chemotactic response of sorted populations of CD25-CD4+ (left panel) and CD25+CD4+ lymph node cells (right panel) was tested in a migration assay. The cells were incubated with either medium alone, with 1 μg/mL of the CCR5 ligand CCL4, or with1 μg/mL of the CCR6 ligand CCL20. After 3 hours the number of migrated cells was determined by FACS analysis. Migration is expressed as chemotactic index and was calculated by the ratio of cells, migrated in the presence of chemokine, to the number of cells that spontaneously migrated with medium alone. One of 3 independent experiments is shown. (B) Depletion of CCR6+ cells abrogates CCL20-induced migration of CD25+CD4+ T cells. The experiment was carried out as described for panel A, except that populations of CD25+CD4+ splenocytes were used, in which the CCR6+ subset was either still present or had been removed prior to the experiment by MACS. (C) CCR6+CD25+ T cells up-regulate IL-10 expression on restimulation in vitro. Using FACS-sorted cells, RNA from CD25+CCR6+, CD25+CCR6-, and as control of CD25-CD4+ T cells was analyzed for IL-10 expression by real-time RT-PCR. RNA was prepared either from freshly isolated cells (left panel) or after stimulation for 4 hours with plate-bound αCD3 (right panel). The relative expression is shown in reference to the IL-10 mRNA level of CD25- control cells. One of 4 independent experiments is shown each with pooled RNA from 8 to 10 animals.
A specific characteristic of effector-memory T cells is a very pronounced cytokine response on antigen recall.41 It was therefore important to determine whether CCR6+ Treg cells share this feature with their nonregulatory counterparts. In contrast to effector T cells, however, Treg cells in general seem to release only very few, if any, cytokines. Because a number of studies indicated that at least some murine Treg cells can produce IL-10,28,42-44 experiments were carried out in which IL-10 production of the CCR6+ and CCR6- Treg subsets was compared by real-time RT-PCR (Figure 5C). mRNA was isolated either from freshly isolated T cells (Figure 5C left panel) or from T cells stimulated in vitro for 4 hours with αCD3 (Figure 5C right panel). Whereas in CCR6- Treg cells the low levels of IL-10 did not increase following stimulation, a significant increase of IL-10 mRNA levels was observed in the population of CCR6+ Treg cells.
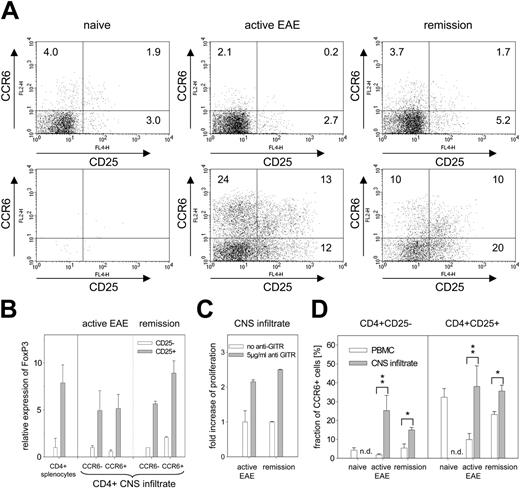
Accumulation of CCR6+ Treg cells in the CNS infiltrate during inflammation
Phenotype and activation status of CCR6+ Treg cells suggests that these cells act directly in inflamed tissues. Because recent studies45,46 showed that high levels of CCL20 are produced in the CNS during the course of EAE, we determined the amount of CCR6+ T cells in blood and in the CNS infiltrate after induction of EAE (Figure 6). Samples were collected from naive mice, from mice with active EAE (score 4), and from mice that had already developed EAE and were in remission (score 0). Whereas only very few cells were detected in perfused brains of naive mice, infiltrating CD4+ T cells could be isolated both during active EAE and during remission (Figure 6A). FACS analysis confirmed that the infiltrating CD4+ lymphocytes were indeed enriched in CCR6+ T cells, which applied for both CD25- as well as CD25+ T cells and was evident in all CNS samples. To ensure that the majority of CD25+ T cells are Treg cells the expression levels of FoxP3 were determined by real-time RT-PCR (Figure 6B). All CD25+ T-cell subsets isolated from the CNS during active EAE or during remission, in fact, produced similar amounts of FoxP3 as CD25+ Treg cells isolated from naive splenocytes. The presence of Treg cells was further demonstrated in an in vitro proliferation assay, in which the activated effector CD4+ T cells of the CNS infiltrate were rendered nonreceptive to the suppressive effect of CD25+ Treg cells by ligation of GITR.26,27,47 As shown in Figure 6C, the addition of αGITR antibodies resulted in an increase of the proliferative response of the CNS infiltrate both from mice with active EAE or from mice in remission.
Accumulation of CCR6+ T cells in the CNS infiltrate during the course of EAE. (A) FACS analysis of cell surface markers CD25 and CCR6 on CD4+ T-cell populations of PBMCs and CNS infiltrate. Lymphocytes of the peripheral blood (top row) and of the CNS infiltrate (bottom row) were stained with antibodies directed against CD4, CD25, and CCR6. Samples were taken from naive mice (left panels), from mice that developed active EAE with a clinical score of 4 (middle panels), or from mice that surpassed the state of active EAE and already reached remission (score 0; right panels). Dot plots are shown for the populations gated on CD4+ cells and display surface staining of CD25 versus CCR6. Numbers represent the percentages of CD4+ cells in each quadrant. One of 4 independent experiments is shown. (B) FoxP3 expression. mRNA expression is shown for FACS populations isolated from the CNS infiltrate of mice with active EAE and from mice in remission. Expression was determined by real-time RT-PCR and is shown for the CCR6- and CCR6+ subsets of CD25-CD4+ T cells (□) and of CD25+CD4+ T cells (▦). Relative expression is shown in reference to the expression level of the CD25-CCR6- subset. Expression of CD25-CD4+ and CD25+CD4+ splenocytes derived from naive mice are shown as control. Each experiment contained RNA from cells obtained by FACS that were pooled from 9 to 10 mice per group. (C) GITR-mediated abrogation of suppressor activity in CNS infiltrates. CNS-infiltrating lymphocytes isolated from mice with active EAE (score 4) and from mice in remission (score 0) were stimulated with anti-CD3 in the absence (□) or presence of anti-GITR (▦). Proliferation was determined after addition of 3H-thymidine and is expressed as fold increase of the proliferation detected in the absence of anti-GITR. One of 2 independent experiments is shown each with cells from 3 to 5 mice per group. (D) Percentage of CCR6+CD25- and CCR6+CD25+ cells in blood and CNS infiltrate. Bars indicate percentage of CCR6+ cells of the CD25-CD4+ and the CD25+CD4+ subset within the PBMCs (□) or the CNS infiltrate (▦). P values are represented by asterisks (single asterisk, P < .05; double asterisk, P < .01) and were calculated according to the Student t test.
Accumulation of CCR6+ T cells in the CNS infiltrate during the course of EAE. (A) FACS analysis of cell surface markers CD25 and CCR6 on CD4+ T-cell populations of PBMCs and CNS infiltrate. Lymphocytes of the peripheral blood (top row) and of the CNS infiltrate (bottom row) were stained with antibodies directed against CD4, CD25, and CCR6. Samples were taken from naive mice (left panels), from mice that developed active EAE with a clinical score of 4 (middle panels), or from mice that surpassed the state of active EAE and already reached remission (score 0; right panels). Dot plots are shown for the populations gated on CD4+ cells and display surface staining of CD25 versus CCR6. Numbers represent the percentages of CD4+ cells in each quadrant. One of 4 independent experiments is shown. (B) FoxP3 expression. mRNA expression is shown for FACS populations isolated from the CNS infiltrate of mice with active EAE and from mice in remission. Expression was determined by real-time RT-PCR and is shown for the CCR6- and CCR6+ subsets of CD25-CD4+ T cells (□) and of CD25+CD4+ T cells (▦). Relative expression is shown in reference to the expression level of the CD25-CCR6- subset. Expression of CD25-CD4+ and CD25+CD4+ splenocytes derived from naive mice are shown as control. Each experiment contained RNA from cells obtained by FACS that were pooled from 9 to 10 mice per group. (C) GITR-mediated abrogation of suppressor activity in CNS infiltrates. CNS-infiltrating lymphocytes isolated from mice with active EAE (score 4) and from mice in remission (score 0) were stimulated with anti-CD3 in the absence (□) or presence of anti-GITR (▦). Proliferation was determined after addition of 3H-thymidine and is expressed as fold increase of the proliferation detected in the absence of anti-GITR. One of 2 independent experiments is shown each with cells from 3 to 5 mice per group. (D) Percentage of CCR6+CD25- and CCR6+CD25+ cells in blood and CNS infiltrate. Bars indicate percentage of CCR6+ cells of the CD25-CD4+ and the CD25+CD4+ subset within the PBMCs (□) or the CNS infiltrate (▦). P values are represented by asterisks (single asterisk, P < .05; double asterisk, P < .01) and were calculated according to the Student t test.
Redistribution of CCR6+ T cells during EAE and their accumulation in the inflamed tissue are summarized in Figure 6D. Whereas the fraction of CCR6+ T cells in the blood decreased dramatically during severe episodes of active EAE, at the same time CCR6+ T cells accumulated within the CNS infiltrate. At the peak of the disease (score 4, day 15 after induction) CCR6+ cells comprised up to 27% of the CD25- and 42% of the CD25+ T-cell population. Within the CD25-CD4+ subset their number decreased to about 15% during remission. The fraction of CCR6+ Treg cells in the CD25+ subset, however, remained almost stable, so that the equilibrium was shifted toward the CCR6+ Treg side during remission, whereas during active EAE these cells were clearly outnumbered by CCR6+CD25- effector T cells.
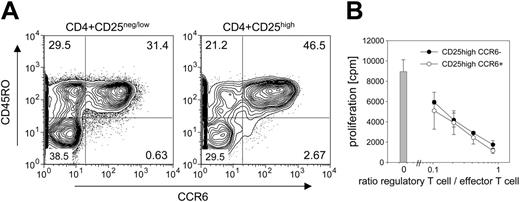
Detection of CCR6+CD25+ regulatory memory-like T cells in human PBMCs
In mice, CD103 expression on Treg cells is associated with effector/memory-like phenotype.29 However, it can also be induced by cytokines, namely by transforming growth factor β (TGF-β)28,29,48 and, more importantly, this marker is virtually absent on human CD25+ Treg cells.49 It can therefore not be used for phenotypic discrimination outside the murine system. To ensure that the association of CCR6 with regulatory memory-like phenotype is also not restricted only to mice, human CD25highCD4+ Treg cells were analyzed by FACS (Figure 7A). Staining with αCCR6 revealed that, depending on the individual, between 30% and 80% of the CD25high T cells and 20% to 70% of the CD25neg/low population in fact express CCR6.
Detection of CCR6+ regulatory memory-like T cells in human PBMCs. (A) FACS analysis. PBMCs were stained with antibodies specific for CD4, CD25, CCR6, and CD45RO. Contour plots are shown for the CD4+ populations gated on high expression of CD25 (CD4+CD25high, right panel), which essentially consists only of Treg cells,50 and the population of CD4+ cells, that express either no or only low levels of CD25 (CD4+CD25neg/low, left panel), which consists mainly of naive and effector cells. The plots show the staining of CCR6 versus CD45RO; the percentage of cells is indicated for each quadrant. One of 5 independent experiments with PBMCs from healthy donors is shown. (B) Suppression assay. CCR6-CD25high (•) and CCR6+CD25high T cells (○) were isolated by FACS from human PBMCs. Their ability to suppress proliferation of CD4+ T cells stimulated by αCD3 was tested as described in Figure 2E. Proliferation in the absence of regulatory CD25high T cells is represented as a bar. Line plot indicates proliferation in presence of increasing amounts of CD25+ T cells. One of 2 independent experiments is shown.
Detection of CCR6+ regulatory memory-like T cells in human PBMCs. (A) FACS analysis. PBMCs were stained with antibodies specific for CD4, CD25, CCR6, and CD45RO. Contour plots are shown for the CD4+ populations gated on high expression of CD25 (CD4+CD25high, right panel), which essentially consists only of Treg cells,50 and the population of CD4+ cells, that express either no or only low levels of CD25 (CD4+CD25neg/low, left panel), which consists mainly of naive and effector cells. The plots show the staining of CCR6 versus CD45RO; the percentage of cells is indicated for each quadrant. One of 5 independent experiments with PBMCs from healthy donors is shown. (B) Suppression assay. CCR6-CD25high (•) and CCR6+CD25high T cells (○) were isolated by FACS from human PBMCs. Their ability to suppress proliferation of CD4+ T cells stimulated by αCD3 was tested as described in Figure 2E. Proliferation in the absence of regulatory CD25high T cells is represented as a bar. Line plot indicates proliferation in presence of increasing amounts of CD25+ T cells. One of 2 independent experiments is shown.
Importantly, in humans CCR6 expression is strictly correlated with CD45RO (Figure 7A). CD45RO is a well-established marker of memory T cells, indicating that also here CCR6 expression on CD25highCD4+ T cells defines a subset of memory T cells. As shown in Figure 7B, these cells are able to suppress proliferation of other CD4+ T cells. Additional data relating to their migratory capacity as well as to expression pattern of other cell surface markers (not shown) further support the presence of equivalent or at least similar CCR6+ effector/memory-like Treg subsets both in humans and mice (manuscript in preparation).
Discussion
Although CCR6+CD25+ T cells are true Treg cells that share phenotype and suppressive capacity with their CCR6- counterparts, they also have many of the characteristic features of “effector-memory” cells. First, they express apparently all cell surface molecules typically present on CD4+ effector-memory T cells (Figure 3A). This includes the murine “memory” marker CD44 as well as classical activation markers such as CD69, CD11a, CD54, and CD5. Also down-regulation of the lymph node homing markers CD62L and CCR7 is evident on CCR6+ Treg cells, a precondition for migration to peripheral sites.33 Second, like conventional CD25- memory cells, CCR6+ Treg cells are generated in vivo on antigen contact (Figure 4). For both, induction of memory phenotype is not immediate and only a fraction of the activated cells actually acquire the effector-memory phenotype. TCR ligation alone is not sufficient to induce a memory phenotype because the process is driven primarily by cytokines.51 Third, CCR6+ Treg cells have a rapid turnover rate in vivo (Figure 3B). Until recently, a rapid turnover rate had not been associated with effector-memory cells. A recent study, however, clearly demonstrated that this is, in fact, a very characteristic feature of effector-memory T cells.37 Finally, effector-memory cells respond to TCR ligation with immediate cytokine production41 and CCR6+ Treg cells clearly up-regulate IL-10 on antigen recall, a feature not observed for CCR6- Treg cells (Figure 5C).
Based on these aspects, CCR6+ Treg cells can be considered as the regulatory equivalent to CD4+ effector-memory T cells. CCR6 expression therefore allows distinguishing regulatory effector/memory-like T cells from naive or recently activated Treg cells and in contrast to CD103, CCR6 is present also on human regulatory memory-like T cells (Figure 7). Although there is apparently no difference in the suppressive capacity of CCR6+ and CCR6- Treg cells in vitro, the discrepancy in their ability to up-regulate IL-10 suggests, however, a nonredundant role for each of the 2 Treg subsets. IL-10 produced by Treg cells has been found to be crucial for the control of inflammatory bowel disease.44,52 Although in our model system the studies do not establish whether CCR6 is involved in the progression of EAE, they show at least that CCR6+ Treg cells accumulate in the CNS during inflammation (Figure 6). A number of reports clearly demonstrated that IL-10-/- mice develop severe chronic EAE53,54 and a recent study even suggests that IL-10 produced by Treg cells is involved also in the control of the disease.55 Thus, CCR6+ Treg cells appear to play a key role in the prevention of organ-specific autoimmune diseases and it had already been communicated that CD25+ Treg cells from CCR6-/- mice, in contrast to cells from wild-type mice, are not able to control induced psoriasis-like diseases or inflammatory bowel disease.56
Because expression of chemokine receptors is closely linked to the function of the cells, they are used as key markers to define cell subsets. Whereas CCR7 discriminates the lymph node resident population of central-memory T cells from effector-memory T cells,41,57 CCR6 appears associated directly with effector-memory function. It mediates migration into peripheral sites because the 2 ligands of CCR6, CCL2058 and β-defensin,59 are expressed mostly in inflamed tissues and mucosal surfaces. The latter is secreted by macrophages and DCs on encounter with microbial pathogens and, as part of the innate immune response, has even a dual function by disrupting cytoplasmic membranes of microorganisms. Thus, CCR6+ T cells seem to be involved primarily in “front-line” immune responses directly in inflamed tissues, where CCR6+ Treg cells act as natural counter-players of effector-memory T cells.
Immune regulation is not a matter of “black and white” but rather of balancing the numbers of proinflammatory and regulatory cells. Because also tolerogenic APCs such as immature DCs and, in particular, IDO+ DCs, express CCR6,20 strength and direction can be further “fine-tuned” by synergistic interactions of Treg cells with these subsets. For instance, expression levels of IDO, the key enzyme of DC-mediated bystander suppression, are sustained by IL-10 and even up-regulated by CD152,60 one of the markers expressed also at highest levels on CCR6+ Treg (Figure 2A). So far, neither in mice nor in humans has a chemokine receptor been identified that is expressed exclusively by regulatory cells. They are always shared by both activating and suppressive lymphocyte populations, which might explain why chemokine receptor knockout mice exhibit only moderate phenotypic differences. Whereas CCR4-/- and CCR8-/- do not show any signs of autoaggression,61,62 CCR6-/- mice58,63 showed at least increased inflammatory responses in contact hypersensitivity studies.63 The same mice, however, exhibited reduced inflammation in a delayed-type hypersensitivity model63 and differential effects were observed also in 2 models of inflammatory bowel disease.64 Thus, depending on the situation, ligands of the same chemokine receptor can attract populations predominantly consisting of either regulatory or effector cells.
Taken together, our data show that CCR6 expression defines a subpopulation of CD25+ memory-like suppressor T cells, present both in mice and humans. Memory, however, consists of 2 elements, effector-memory T cells (TEM) and central-memory T cells (TCM). Whereas the rapidly cycling TEM cells provide immediate protection against invading pathogens in peripheral tissues, long-lasting TCM cells are likely to generate new waves of effector cells in antigen-draining lymph nodes.65 Several recent studies have shown already that therapeutic vaccination can lead to persisting tolerance by addressing Treg cells.7,66 This study introduces CCR6+ Treg cells as a population that seems to represent “regulatory effector-memory” T cells (TREM). It remains to be seen, though, whether also “regulatory central-memory” T cells (TRCM) as equivalent to TCM cells exist.
Prepublished online as Blood First Edition Paper, December 21, 2004; DOI 10.1182/blood-2004-07-2505.
Supported by a grant awarded by the clinical cooperation program of the Max-Delbrück-Center (F.P.).
The online version of the article contains a data supplement.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 U.S.C. section 1734.
We thank J. G. Cyster for the CCL19-Fc fusion protein; D. C. Wraith for transgenic mice; G. Müller, M. Lipp, T. Kammertöns, and T. Blankenstein for reagents; K. Raba und T. Kaiser from the DRFZ for cell sorting; L. Santambrogio for advice; A. Sgobio for help in statistical data analysis; M. Hofstätter, S. Kleissle, K. Petsch, and A. Diamantini for technical assistance; and S. Giering for help in preparing the manuscript.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal