Stimulation of platelet G protein–coupled receptors results in the cleavage of phosphatidylinositol 4,5-trisphosphate (PIP2) into inositol 1,4,5-trisphosphate and 1,2-diacylglycerol by phospholipase C (PLCβ). It also results in the phosphorylation of PIP2 by the γ isoform of phosphatidylinositol 3-kinase (PI3Kγ) to synthesize phosphatidylinositol 3,4,5-trisphosphate. To understand the role of PIP2 in platelet signaling, we evaluated knock-out mice lacking 2 isoforms of PLCβ (PLCβ2 and PLCβ3) or lacking the Gβγ-activated isoform of PI3K (PI3Kγ). Both knock-out mice were unable to form stable thrombi in a carotid injury model. To provide a functional explanation, knock-out platelets were studied ex vivo. PLCβ2/β3–/– platelets failed to assemble filamentous actin, had defects in both secretion and mobilization of intracellular calcium, and were unable to form stable aggregates following low doses of agonists. Platelets lacking PI3Kγ disaggregated following low-dose adenosine diphosphate (ADP) and had a mildly impaired ability to mobilize intracellular calcium. Yet, they exhibited essentially normal actin assembly and secretion. Remarkably, both PLCβ2/β3–/– and PI3Kγ–/– platelets spread more slowly upon fibrinogen. These results suggest substantial redundancy in platelet signaling pathways. Nonetheless, the diminished ability of knock-out platelets to normally spread after adhesion and to form stable thrombi in vivo suggests that both PLCβ2/β3 and PI3Kγ play vital roles in platelet cytoskeletal dynamics.
Introduction
Human platelets play critical roles in hemostasis and thrombosis by adhering to and aggregating at sites of vascular injury. Thus, inactive circulating platelets are recruited to the site of vascular injury and activated by a process that involves agonist binding to cell-surface receptors, activation of both guanine nucleotide binding regulatory proteins (G proteins) and protein kinases, as well as the generation of lipid second messengers. Stimulation of G protein–coupled receptors leads to the production of lipid second messengers by 2 distinct classes of enzymes: the β isoforms of phospholipase C (PLCβ) and the γ isoform of phosphatidylinositol 3-kinase (PI3Kγ). Human platelets contain 4 isoforms of PLCβ that are activated by receptors coupled to G proteins containing a Gαq subunit. Stimulation of receptors coupled to G proteins containing a Gαi subunit result in the Gβγ-mediated activation of PI3Kγ.1
PLCβ isoforms hydrolyze phosphatidylinositol 4,5-trisphosphate (PIP2) to generate the second messengers inositol 1,4,5-trisphosphate (IP3) and 1,2-diacylglycerol (DAG).2 The latter in turn release intracellular calcium stores and activate classical and novel isoforms of protein kinase C (PKC), respectively.3,4 PI3Kγ phosphorylates PIP2 to generate the lipid second messenger phosphatidylinositol 3,4,5-triphosphate (PIP3).1 A role for PIP3 in platelets remains to be identified, but it does lead to the activation of Akt,5 and in other cells it stimulates the activity of both phosphatidylinositol-dependent kinase 1 (PDK1) and exchange factors for Rho family guanosine triphosphate phosphohydrolases (GTPases).6
An inherited deficiency of PLCβ2 has been reported to result in a bleeding diathesis and defective platelet aggregation and secretion ex vivo.7-9 Because PLCβ2 is the predominant isoform of PLCβ in human platelets, it suggests PLCβ is a critical component of platelet signaling.7 Although there are no reports of genetic abnormalities of PI3Kγ in humans, Hirsch and colleagues reported that PI3Kγ-null mice have a mild platelet aggregation defect and impaired thrombosis following injection with collagen and epinephrine.10
Nonetheless, the relative contributions of PLCβ and PI3Kγ to platelet function are not known. Given the availability of specific murine models, we have addressed this question by studying the function of platelets from genetically modified mice lacking PI3Kγ or both PLCβ2 and PLCβ3. We found that the lipid second messengers generated by these enzymes affect different aspects of platelet function ex vivo, yet each enzyme is required for normal platelet function in vivo.
Materials and methods
Reagents
Antibodies against the individual isoforms of PLCβ were acquired from Santa Cruz Biotechnology (Santa Cruz, CA). Bovine albumin was obtained from ICN Biomedicals (Costa Mesa, CA). Fura-2 am, Vybrant DiO, and Alexa Fluor 633-phalloidin were purchased from Molecular Probes (Eugene, OR). Human α-thrombin was acquired from Haematologic Technologies (Essex Junction, VT). Immunoblotting reagents were purchased from Invitrogen (Carlsbad, CA). The adenosine triphosphate (ATP) standard was obtained from Chrono-Log (Havertown, PA). All other reagents were purchased from Sigma (St Louis, MO).
Animal models
The generation of the murine lines lacking PI3Kγ (PI3Kγ–/–) or both PLCβ2 and PLCβ3 (PLCβ2/β3–/–) has been previously described.11 The PI3Kγ-null line was backcrossed 6 generations into a C57BI6 genetic background, and the PLCβ2/β3-null line was backcrossed 6 generations into a CD1 genetic background. The Institutional Animal Care and Use Committee of the University of Pennsylvania approved the studies using these animals.
Immunoblotting
Murine (1.5 × 108) or human (1 × 108) platelets were lysed in NuPAGE LDS Sample Buffer (Invitrogen) and then fractionated by electrophoresis on a 7% to 12% bis-tris gel. After transfer to nitrocellulose membranes, blots were incubated with anti–mouse PLCβ1, PLCβ2, PLCβ3, or PLCβ4 antibodies as per protocols recommended by the manufacturer (Santa Cruz Biotechnology).
Carotid artery injury induced by FeCl3
Mice weighing 20 to 30 g at the age of 8 weeks were anesthetized using sodium pentobarbital 80 mg/kg by intraperitoneal injection.12,13 A midline incision was made in the neck, and the right carotid artery was exposed by blunt dissection. A 1 × 2–mm patch of no. 1 Whatman filter paper (Whatman, Florham Park, NJ), soaked in either 10% FeCl3 for C57BL/6J mice or 15% FeCl3 for CD1 mice, was applied to the exposed artery for 2 minutes. After removal of the filter paper, the artery was washed with phosphate-buffered saline (PBS) and blood flow was recorded using a small animal blood flow meter (model T106; Transonic Systems, Ithaca, NY) for up to 30 minutes. Thrombus formation, as defined by lack of arterial flow, was recorded for data analysis. Occlusive thrombi were considered stable if total occlusion lasted for more than 10 minutes.
Measurement of cytoplasmic calcium concentration
Platelets were washed twice in HEPES (N-2-hydroxyethylpiperazine-N′-2-ethanesulfonic acid)–Tyrode buffer containing 1 mM EGTA (ethylene glycol tetraacetic acid), pH 6.5, in the presence of 0.5 μM prostaglandin E1 (PGE1). They were then resuspended at a concentration of 2 × 108/mL in HEPES-Tyrode buffer, pH 7.4. After loading with 5 μM Fura-2 am for 40 minutes at 37°C in the dark, the platelets were sedimented at 833g for 15 minutes at 25°C and the pellet was resuspended at a final platelet concentration of 2 × 108/mL in HEPES-Tyrode buffer, pH 7.4, immediately prior to analysis.
Aliquots of Fura-2-AM–loaded platelets were transferred to a 10 × 10–mm cuvet and prewarmed to 37°C. For some experiments, CaCl2 was added to a final concentration of 1 mM and the cells were activated with 1 U/mL human α-thrombin or 10 μM adenosine diphosphate (ADP). Subsequent measurements of Fura-2-AM fluorescence were performed under continuous stirring using an SLM-Aminco model AB2 fluorescence spectrophotometer (SLM-Aminco, Urbana, IL) with excitation at dual wavelengths of 340 nm and 380 nm and emission spectra measured at 510 nm.
Platelet aggregation and secretion
Blood from the vena cava of anesthetized mice was anticoagulated with 15 U/mL heparin and centrifuged at 200g for 7 minutes at room temperature to obtain platelet-rich plasma (PRP). The concentration of platelets in the PRP was adjusted to 2.5 × 108 platelets per milliliter using HEPES-Tyrode buffer, pH 7.4 (134 mM NaCl, 3 mm KCl, 0.3 mM NaH2PO4, 12 mM NaHCO3, 2 mM MgCl2, 5 mM HEPES, 5 mM glucose, 0.35% bovine albumin). Alternatively, platelets were washed as described in the previous section and resuspended in HEPES-Tyrode buffer, pH 7.4, with 1 mM CaCl2.
Platelet aggregation in response to agonist stimulation was measured by the turbidometric method at 37°C in a Lumi-dual Aggregometer (Chrono-Log). Platelet ATP secretion was measured concurrently by means of the luciferin/luciferase reaction after adding Chrono-lume no. 395 (Chrono-Log) to the aggregometer cuvet.
Platelet actin assembly
Washed platelets were resuspended at a concentration of 1 × 107/mL in HEPES-Tyrode buffer, pH 7.4. After prewarming for 5 minutes at 37°C, they were stimulated with 1 U/mL α-thrombin. One minute after the addition of thrombin, the platelets were fixed by adding a 0.55 volume of 10% paraformaldehyde for 3 minutes. The fixed cells were permeabilized and stained by adding a 0.1 volume of 1% Triton X-100 containing 45 μM Alexa Fluor 633–phalloidin at 25°C. Phalloidin binding was measured by flow cytometry (FACSCalibur, Becton Dickinson, San Jose, CA), and data were analyzed using CELLQuest v 3.3 software (Becton Dickinson, Franklin Lakes, NJ).
Spreading of platelets on immobilized fibrinogen
Glass slides were coated with fibrinogen by covering them overnight at 4°C with a solution of 100 μg/mL fibrinogen dissolved in PBS. The coated slides were washed 3 times with PBS, blocked with bovine serum albumin (BSA) 5 mg/mL in PBS for 2 hours at room temperature, and washed 3 times in PBS. Washed platelets, resuspended at a final concentration of 5 × 107/mL in HEPES-Tyrode buffer containing 1 mM CaCl2, were then layered over fibrinogen-coated slides and allowed to spread for up to 45 minutes in the presence of 500 μM thrombin receptor agonist peptide “AYP” (AYPGQV). The spread platelets were fixed with 10% paraformaldehyde, washed twice with PBS, and stained for 10 minutes at 37°C with 5 μM Vybrant DiO (Molecular Probes, Eugene, OR). Images of the adherent fixed platelets were imaged by an Olympus AX70 analytic microscope equipped with a 100× objective lens (Olympus, Melville, NY). Images were captured with a Sensys CCD digital camera (Photometrics, Tucson, AZ) coupled to a MacIntosh computer and were processed with IPLab software (Signal Analytics, Vienna, VA).
Results
Characterization of PLCβ isoforms in PLCβ2/β3 knock-out platelets
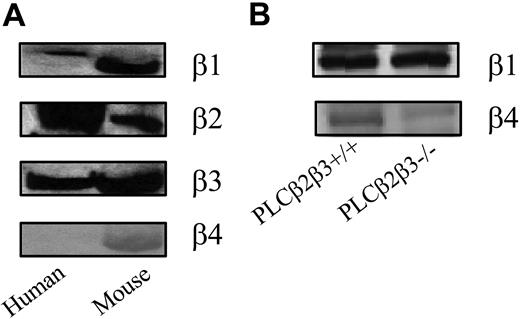
The predominant isoform of PLCβ in human platelets is PLCβ2.7 A small amount of PLCβ3 is detectable, but there is little PLCβ1 and PLCβ4. Surprisingly, we found that murine platelets, compared with human platelets, have relatively less PLCβ2 and relatively more PLCβ1 and PLCβ3 (Figure 1). Nonetheless, to ensure that deleting PLCβ2 and PLCβ3 in murine platelets did not induce a compensatory increase in PLCβ1 or PLCβ4 expression, we immunoblotted PLCβ2/β3–/– murine platelets with antibodies specific for PLCβ1 or PLCβ4. There was no increase in the intensity of bands corresponding to PLCβ1 and PLCβ4 in the PLCβ2/β3-null platelets (Figure 1).
Immunoblots of PLCβ isoforms in wild-type and PLCβ2/β3-null platelets. Total cell lysates containing human or murine platelets were fractionated by gel electrophoresis and immunoblotted with PLCβ isoform-specific polyclonal antibodies. (A) Murine platelets have relatively less PLCβ2 and relatively more PLCβ1. (B) Murine platelets lacking PLCβ2 and PLCβ3 did not have a compensatory increase in PLCβ1 or PLCβ4.
Immunoblots of PLCβ isoforms in wild-type and PLCβ2/β3-null platelets. Total cell lysates containing human or murine platelets were fractionated by gel electrophoresis and immunoblotted with PLCβ isoform-specific polyclonal antibodies. (A) Murine platelets have relatively less PLCβ2 and relatively more PLCβ1. (B) Murine platelets lacking PLCβ2 and PLCβ3 did not have a compensatory increase in PLCβ1 or PLCβ4.
PLCβ2/β3- and PI3Kγ-deficient platelets have impaired in vivo function
Mice whose platelets lacked either PLCβ2/β3 or PI3Kγ displayed no overt evidence of spontaneous bleeding or thrombosis. Because it is possible that abnormalities might become apparent only under conditions of hemostatic stress, we tested the ability of these mice to form stable clots using a chemical-induced carotid injury model.12,13 Ferric chloride was applied to an exposed carotid artery of anesthetized mice, and the formation of thrombi was monitored by Doppler ultrasound.
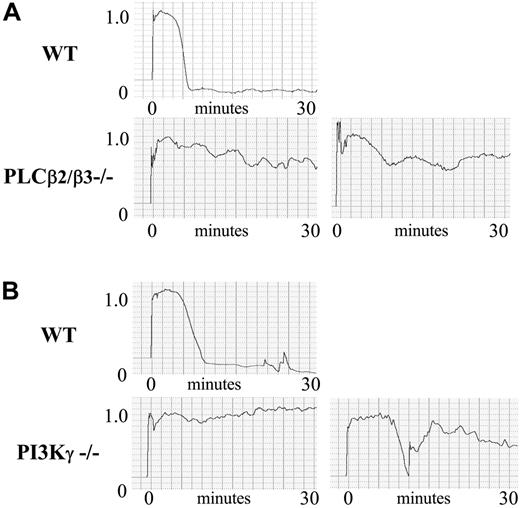
An example of a typical experiment is shown in Figure 2. In this experiment, wild-type mice rapidly formed occlusive thrombi that were stable over the 30-minute length of the experiment. By contrast, arterial occlusion was not detected in the 2 PLCβ2/β3–/– mice shown (Figure 2A, lower panels). Thrombus formation in response to chemical-induced injury was also defective in PI3Kγ-null mice. In the example shown in Figure 2B (lower left panel), the thrombus completely failed to form in one PI3Kγ–/– mouse. In the other example shown (Figure 2B, lower right panel), a thrombus formed after an 8-minute lag. However, this was unstable and washed away. The results of experiments using 7 PLCβ2/β3–/– and 8 PI3Kγ–/– mice are shown in Table 1. They indicate that absence of either PLCβ2/β3 or PI3Kγ in platelets completely prevents the formation of stable arterial thrombi. This demonstrates that each enzyme is required for normal in vivo platelet function.
Effect of PLCβ2/β3 or P13Kγ knock-out in carotid injury model
. | Stable . | Unstable . | No clot . |
|---|---|---|---|
| PLCβ/β3+/+ | 10 | 2 | 0 |
| PLCβ2/β3-/- | 0 | 1 | 6 |
| P13Kγ+/+ | 12 | 2 | 0 |
| P13Kγ-/- | 0 | 3 | 5 |
. | Stable . | Unstable . | No clot . |
|---|---|---|---|
| PLCβ/β3+/+ | 10 | 2 | 0 |
| PLCβ2/β3-/- | 0 | 1 | 6 |
| P13Kγ+/+ | 12 | 2 | 0 |
| P13Kγ-/- | 0 | 3 | 5 |
Mice lacking either PLCβ2/β3 or P13Kγ were analyzed by a ferric chloride-induced carotid injury model. Results from multiple independent experiments are shown. These data demonstrate that loss of either PLCβ2/β3 or P13Kγ induces a defect that prevents stable arterial thrombus formation.
Effect of PI3Kγ- or PLCβ2/β3-null mutations on in vivo thrombosis. Carotid injury was induced by application of FeCl3-soaked filter paper for 2 minutes, and vessel occlusion was monitored by a Doppler ultrasound. The Doppler tracings show flow (milliliters per minute) on the y axis and time on the x axis. Control mice typically developed stable occlusions within their injured arteries. In contrast, PLCβ2/β3 and PI3Kγ knock-out mice both failed to form stable arterial occlusions in response to chemical injury.
Effect of PI3Kγ- or PLCβ2/β3-null mutations on in vivo thrombosis. Carotid injury was induced by application of FeCl3-soaked filter paper for 2 minutes, and vessel occlusion was monitored by a Doppler ultrasound. The Doppler tracings show flow (milliliters per minute) on the y axis and time on the x axis. Control mice typically developed stable occlusions within their injured arteries. In contrast, PLCβ2/β3 and PI3Kγ knock-out mice both failed to form stable arterial occlusions in response to chemical injury.
Second messengers generated by PLCβ2/β3 and PI3Kγ are required for the platelet calcium response
IP3 generated by PLC-mediated PIP2 hydrolysis causes the release of calcium from the platelet-dense tubular system.4 Although the PLCβ mediates this process after stimulation of G protein–coupled receptors, PLCγ hydrolyzes PIP2 after stimulation of glycoprotein VI (GPVI) by collagen. Interestingly, PI3K enhances the activation of PLCγ and thereby increases GPVI-mediated PIP2 hydrolysis.14 This effect of PI3K on the regulation of PLCγ may be due to PI3K-generated phospholipid products binding to the pleckstrin homology (PH) domain within PLCγ and thereby orienting PLCγ for optimal enzymatic activity.15,16 It is currently unknown whether PI3K products also bind to the PH domain of PLCβ and regulate the ability of this PLC isoform to hydrolyze PIP2.
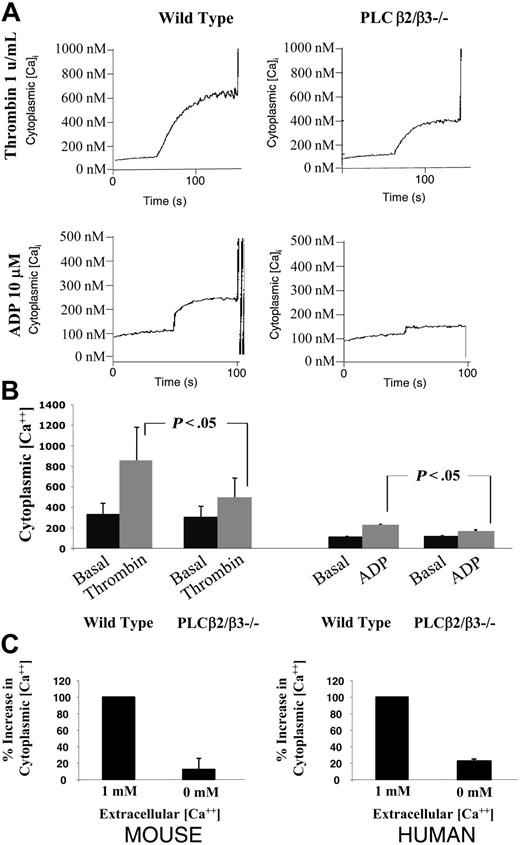
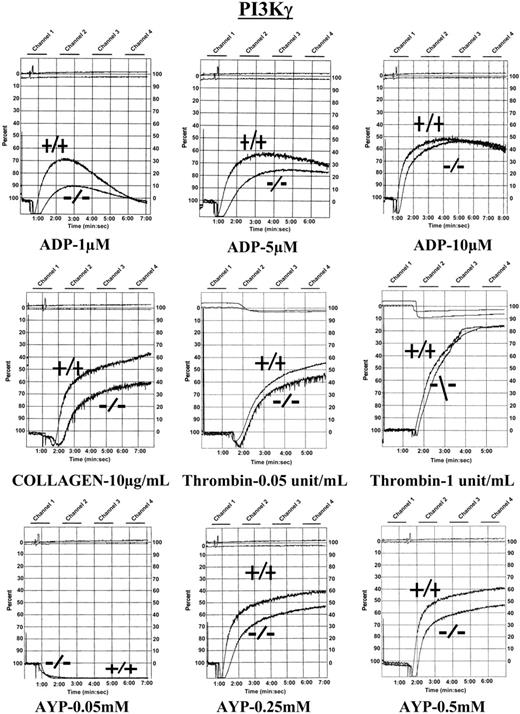
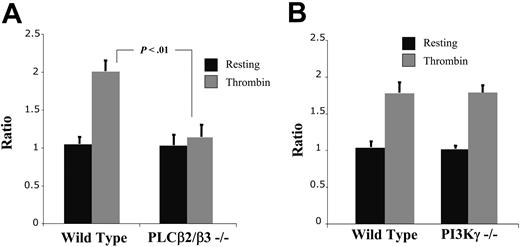
To determine the relative contribution of PLCβ2/β3 and PI3Kγ to the increased platelet cytosolic calcium induced by stimulation of G protein–coupled receptors, we measured agonist-stimulated calcium mobilization in the platelets of PLCβ2/β3–/– and PI3Kγ–/– mice. Murine platelets were incubated with the calcium fluorophore Fura-2 AM, stimulated with 1 U/mL thrombin, and the resulting increase in Fura-2 fluorescence quantitated as a function of time. As shown in Figure 3A-B, the PLCβ2/β3–/– platelets had a statistically significant 58% decrease in thrombin-stimulated Fura-2 fluorescence (n = 6, P < .05) and a 43% decrease in ADP-stimulated Fura-2 fluorescence (n = 3, P < .05).
Thrombin causes a rise in the concentration of cytosolic calcium by releasing a pool of calcium stored in the dense tubular system and by opening ion channels that allow for the influx of extracellular calcium. Because loss of PLCβ2/β3 activity could impair either source of calcium, we analyzed the relative contribution of extracellular calcium in wild-type and PLCβ2/β3-null platelets. We found that the absence of extracellular calcium eliminated 90% of the rise in cytosolic concentration of calcium in wild-type murine platelets (Figure 3C). A similar dependency on extracellular calcium was found in PLCβ2/β3-null murine platelets and in human platelets. These results indicate that the major source of the transient rise in cytoplasmic calcium is by influx through the cellular membrane and that this influx is regulated, at least in part, by PLCβ.
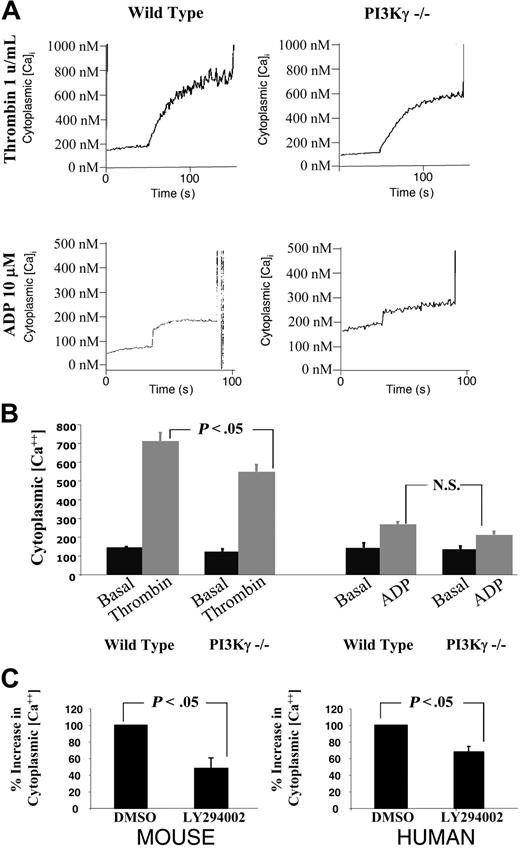
To determine whether PIP3 also contributes to the platelet calcium response, we measured thrombin-stimulated Fura-2 fluorescence in platelets from PI3Kγ–/– mice.14 As shown in Figure 4A-B, the response of PI3Kγ–/– platelets was 25% less than that of wild-type platelets. This indicates that PI3Kγ makes a small but significant contribution to the calcium response (n = 3, P < .05). We also found that pharmacologic inhibition of PI3K with LY294002 impaired the thrombin-induced rise in cytosolic calcium by an even larger extent (Figure 4C). Because this inhibitor affects all PI3K isoforms, these results suggest that other PI3K isoforms present in platelets also contribute to this process. Pharmacologic inhibition of PI3K also impairs the thrombin-induced rise in cytosolic calcium in human platelets, indicating that a similar pathway also exists in these cells.
Platelet cytoplasmic calcium concentration in PLCβ2/β3-null platelets. Washed murine platelets were incubated with a calcium fluorophore (Fura-2 AM) and then stimulated with either 1 U/mL thrombin or 10 mM ADP. The concentration of cytoplasmic calcium (nM) was quantitated as a function of time. (A) Representative fluorimetry tracings of experiments using thrombin- or ADP-stimulated wild-type and PLCβ2/β2-null platelets. (B) A graph displaying the mean ± SEM of the cytosolic calcium concentration for 6 experiments. (C) A graph demonstrating the influence of the extracellular calcium concentration on the ability of platelets to raise their cytoplasmic calcium concentration in response to 1 U/mL thrombin. The change in cytosolic calcium was normalized to the response seen in wild-type cells. The graphs show the mean ± SEM for 3 experiments.
Platelet cytoplasmic calcium concentration in PLCβ2/β3-null platelets. Washed murine platelets were incubated with a calcium fluorophore (Fura-2 AM) and then stimulated with either 1 U/mL thrombin or 10 mM ADP. The concentration of cytoplasmic calcium (nM) was quantitated as a function of time. (A) Representative fluorimetry tracings of experiments using thrombin- or ADP-stimulated wild-type and PLCβ2/β2-null platelets. (B) A graph displaying the mean ± SEM of the cytosolic calcium concentration for 6 experiments. (C) A graph demonstrating the influence of the extracellular calcium concentration on the ability of platelets to raise their cytoplasmic calcium concentration in response to 1 U/mL thrombin. The change in cytosolic calcium was normalized to the response seen in wild-type cells. The graphs show the mean ± SEM for 3 experiments.
Effect of PLCβ2/β3 and PI3Kγ deficiencies on platelet secretion
Studies using pharmacologic inhibitors suggest that an increase in cytosolic calcium and PKC activation are both required for maximal platelet secretion, implying involvement of PLCβ in this process.17 In cells other than platelets, exocytosis is sensitive to pharmacologic inhibition of PI3K, yet a role for PI3K in platelet exocytosis remains controversial.18,19 To determine whether loss of either PLCβ2/β3 or PI3Kγ impairs platelet exocytosis, we measured agonist-stimulated secretion of ATP in washed platelets using the luciferin-luciferase reaction.
We found that secretion was impaired in PLCβ2/β3–/– platelets following stimulation of the weaker platelet agonists ADP and U46619 (thromboxane A2 analog). However, there was no significant defect in collagen- or thrombin-stimulated secretion (Figure 5A). In fact, collagen-mediated platelet secretion, which is mediated by PLCγ, was mildly enhanced in PLCβ2/β3–/– platelets. In contrast to the findings in the PLCβ2/β3 knock-out platelets, PI3Kγ–/– platelets were able to secrete granules as efficiently as wild-type platelets (Figure 5B). This normal secretion in PI3Kγ-null platelets does not eliminate the possibility that other PI3K isoforms could contribute to platelet exocytosis under certain circumstances. In fact, it has been reported that platelets lacking the critical p85α subunit of other PI3K isoforms have a defect in collagen-induced platelet secretion.20
Both PLCβ2/β3 and PI3Kγ contribute to platelet aggregation
PLC and PI3K each contribute to the signaling responsible for platelet aggregation,7,8,21 yet it is not clear which isoforms of the enzymes are involved. Genetic studies suggest that p85α-coupled isoforms of PI3K (PI3Kα, PI3Kβ, and PI3Kδ) play a dominant role in GPVI-mediated platelet aggregation but are not involved in aggregation stimulated by G protein–coupled receptors.20 Similarly, a study using an independently derived PI3Kγ-null cell line suggests that PI3Kγ has only a contributory role in aggregation stimulated by ADP.10 To test the relative contribution of PLCβ2/β3 and PI3Kγ to platelet aggregation initiated by G protein–coupled receptors, we compared the ex vivo aggregation of platelets obtained from PLCβ2/β3–/– and PI3Kγ–/– mice.
Platelet cytoplasmic calcium concentration in PI3Kγ-null platelets. Washed murine platelets were incubated with a calcium fluorophore (Fura-2 AM) and then stimulated with either 1 U/mL thrombin or 10 mM ADP. The concentration of cytoplasmic calcium (nM) was quantitated as a function of time. (A) Representative fluorimetry tracings of experiments using thrombin- or ADP-stimulated wild-type and PI3Kγ-null platelets. (B) A graph displaying the mean ± SEM of the cytosolic calcium concentration for 3 experiments. (C) A graph demonstrating the influence of the extracellular calcium concentration on the ability of platelets to raise their cytoplasmic calcium concentration in response to 1 U/mL thrombin. The change in cytosolic calcium was normalized to the response seen in wild-type cells. The graph shows the mean ± SEM for 3 experiments.
Platelet cytoplasmic calcium concentration in PI3Kγ-null platelets. Washed murine platelets were incubated with a calcium fluorophore (Fura-2 AM) and then stimulated with either 1 U/mL thrombin or 10 mM ADP. The concentration of cytoplasmic calcium (nM) was quantitated as a function of time. (A) Representative fluorimetry tracings of experiments using thrombin- or ADP-stimulated wild-type and PI3Kγ-null platelets. (B) A graph displaying the mean ± SEM of the cytosolic calcium concentration for 3 experiments. (C) A graph demonstrating the influence of the extracellular calcium concentration on the ability of platelets to raise their cytoplasmic calcium concentration in response to 1 U/mL thrombin. The change in cytosolic calcium was normalized to the response seen in wild-type cells. The graph shows the mean ± SEM for 3 experiments.
Platelet ATP secretion in response to agonist stimulation. Secretion of washed platelets was measured at 37°C by the turbidometric method in a Lumi-dual Aggregometer following the addition of various agonists. Secretion induced by low doses of ADP or U46619 (thromboxane A2 analog) was impaired in PLCβ2/β3 knock-out platelets (A). Shown are means ± standard error of 3 experiments. Similar results were seen in 7 experiments analyzing secretion in platelet-rich plasma. (B) A graph showing an analysis of the agonist-induced secretion response of PI3Kγ-null platelets compared with control cells. Paired student t testing revealed no significant defect in PI3Kγ knock-out platelets with any agonist. Shown are the means ± SEM normalized in 2 experiments. A similar lack of secretion defect was found in 3 experiments analyzing secretion in platelet-rich plasma (not shown).
Platelet ATP secretion in response to agonist stimulation. Secretion of washed platelets was measured at 37°C by the turbidometric method in a Lumi-dual Aggregometer following the addition of various agonists. Secretion induced by low doses of ADP or U46619 (thromboxane A2 analog) was impaired in PLCβ2/β3 knock-out platelets (A). Shown are means ± standard error of 3 experiments. Similar results were seen in 7 experiments analyzing secretion in platelet-rich plasma. (B) A graph showing an analysis of the agonist-induced secretion response of PI3Kγ-null platelets compared with control cells. Paired student t testing revealed no significant defect in PI3Kγ knock-out platelets with any agonist. Shown are the means ± SEM normalized in 2 experiments. A similar lack of secretion defect was found in 3 experiments analyzing secretion in platelet-rich plasma (not shown).
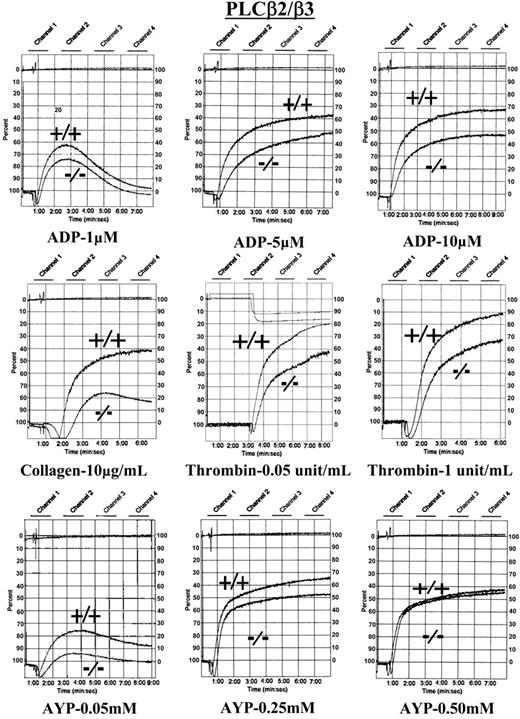
We found small decreases in the extent and rate of aggregation of PLCβ2/β3–/– platelets stimulated by ADP, thrombin (or the PAR4 agonist peptide “AYP”), or collagen (Figure 6). Impaired aggregation was most apparent at lower agonist concentrations and became less so as the agonist concentration was increased. Platelets from PI3Kγ–/– platelets aggregated less well than wild-type platelets when stimulated by ADP and collagen (Figure 7). In the case of ADP, the differences between the PI3Kγ–/– and wild-type platelets disappeared as the ADP concentration increased. These data demonstrate that PLCβ2/β3 and PI3Kγ both participate in agonist-stimulated platelet aggregation and appear to be required for maximum responses.
Platelet-actin assembly requires PLCβ2/β3 but not PI3Kγ
Following agonist stimulation, platelets rapidly reorganize their actin cytoskeletons by a process that includes the assembly of F-actin.18,22 Thus, after thrombin stimulation, the platelet content of F-actin increases by 50% to 75% and is limited by the availability of monomer G-actin.23 Moreover, it is likely that cytoskeletal reorganization is needed to enable platelets to firmly adhere to matrices under high shear conditions.24
In the carotid artery injury model shown in Figure 1, we found that PLCβ2/β3–/– and PI3Kγ–/– platelets were unable to form stable thrombi. To determine whether this resulted from impaired actin reorganization, using flow cytometry we measured the F-actin content of unstimulated and thrombin-stimulated platelets from PLCβ2/β3–/– and PI3Kγ–/– mice. As shown in Figure 8, the basal F-actin contents of PLCβ2/β3–/– and PI3Kγ–/– platelets was identical with control platelets. However, after thrombin stimulation there was no change of the F-actin content in PLCβ2/β3–/– platelets. This indicates that second messengers generated by PLCβ are required for F-actin assembly. Therefore, impaired actin assembly may contribute to the inability of PLCβ2/β3–/– platelets to form stable thrombi. By contrast, the increase of F-actin in PI3Kγ–/– platelets following thrombin stimulation was identical to wild-type platelets. This indicates that actin assembly cannot account for the PI3Kγ–/– defect found in the carotid injury model (Table 1) and demonstrates that other PI3K-dependent factors must contribute to the formation of stable adherent platelet thrombi.
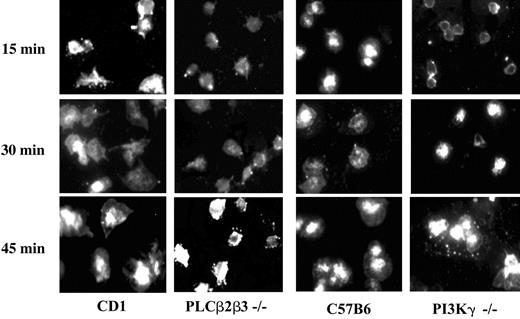
Second messengers generated by both PLCβ2β3 and PI3Kγ are required for platelet spreading
Platelet spreading at sites of vascular injury is a complex process. It involves not only actin reorganization but also the platelet microtubule, myosin motors, and integrins.25,26 To investigate the role of PLCβ2/β3 and PI3Kγ in platelet spreading, we allowed washed murine platelets to attach and spread on a fibrinogen-coated surface for up to 45 minutes. The adherent platelets were fixed at various time points, incubated with the nonspecific membrane labeling solution (Vybrant DiO), and examined by fluorescence microscopy. Although the small size of platelets precluded accurate quantitation of spreading, inspection of the micrographs (Figure 9) revealed clear differences in the rate of spreading among the various types of platelets. There was only a small difference between knock-out platelets and wild-type platelets at 45 minutes after plating. However, at 15 and 30 minutes after plating there was substantial spreading of the wild-type platelets while there was little spreading of either knock-out platelets. Thus, these experiments indicate that both PI3Kγ and PLCβ2/β3 enzymes generate second messengers that contribute to the early phases of platelet spreading.
Aggregation tracings of platelets lacking PLCβ2/β3. Murine platelets lacking PLCβ2/β3 were analyzed after agonist stimulation in a Lumi-dual Aggregometer. Platelets lacking both PLCβ2 and PLCβ3 have a defect in aggregation in response to ADP and low doses of thrombin and exhibit impairment in the second wave of aggregation. Results are representative of 9 experiments performed to date.
Aggregation tracings of platelets lacking PLCβ2/β3. Murine platelets lacking PLCβ2/β3 were analyzed after agonist stimulation in a Lumi-dual Aggregometer. Platelets lacking both PLCβ2 and PLCβ3 have a defect in aggregation in response to ADP and low doses of thrombin and exhibit impairment in the second wave of aggregation. Results are representative of 9 experiments performed to date.
Aggregation tracings of platelets lacking PI3Kγ. Murine platelets lacking the γ isoform of PI3K were analyzed after agonist stimulation. Platelets lacking PI3Kγ had a mild defect in agonist-mediated aggregation associated with an impaired second wave of aggregation. Results are representative of 7 experiments performed to date.
Aggregation tracings of platelets lacking PI3Kγ. Murine platelets lacking the γ isoform of PI3K were analyzed after agonist stimulation. Platelets lacking PI3Kγ had a mild defect in agonist-mediated aggregation associated with an impaired second wave of aggregation. Results are representative of 7 experiments performed to date.
Discussion
Our studies demonstrate that hydrolysis of PIP2 by PLCβ and phosphorylation of PIP2 by PI3Kγ affect different aspects of platelet activation. However, both are required for complete platelet function in vivo. Aspects of these observations are consistent with published reports of signaling pathways in platelets exposed to calcium chelators or pharmacologic inhibitors of PI3K or PKC. Our finding that PI3Kγ contributes to ADP-specific aggregation confirms the observation made by Hirsch et al, who used an independently derived murine line.10 Although we studied murine platelets lacking both PLCβ2 and PLCβ3, our work is also consistent with studies by Rao and colleagues that described a patient with platelet dysfunction attributed to decreased expression of PLCβ2.7-9
One striking aspect of this current work is the demonstration of a significant in vivo defect associated with relatively mild ex vivo studies. Mice lacking either PLCβ2/β3 or PI3Kγ never formed a stable thrombosis following chemical-induced injury of their carotid arteries. Yet, we detected only modest to moderate differences between the knock-out lines and their controls with respect to ex vivo platelet aggregation, secretion, or ability to raise intracellular calcium. Our finding of impaired platelet spreading suggests that the in vivo defect may be due to essential roles of both PLCβ and PI3Kγ in organizing the platelet cytoskeleton. This is consistent with the critical contribution of cytoskeletal dynamics to the ability of platelets to adhere to the vessel wall under conditions of shear found within the arterial system.
This work demonstrates that PLCβ2/β3 knock-out platelets have a defect in their ability to raise the concentration of cytosolic calcium following agonist stimulation. The residual calcium response in PLCβ2/β3-null platelets is potentially due to signaling by residual amounts of other PLC isoforms (predominantly PLCβ1) in murine platelets. The agonist-induced increase in cytoplasmic calcium is required for multiple calcium-dependent enzymes critical for platelet actin reorganization. For example, activation of the severing activity of gelsolin requires a rise of several hundred nanomolar concentrations of cytosolic calcium.27,28 Once stimulated, gelsolin creates an increase in uncapped barbed ends on F-actin and thus generates a nidus for further actin assembly.29 The rise in the cytosolic calcium concentration within platelets is also required for activation of actin-regulating Rho-family GTPases.30 Additionally, calcium mobilization regulates μ-calpain, a protease essential for clot retraction.31-33
We were surprised to observe the impaired calcium response in both the PI3Kγ knock-out platelets and in the normal platelets exposed to a pharmacologic inhibitor of PI3K. To our knowledge, this is the first time it has been established that there is a role for PI3K in mediating a thrombin-stimulated increase in the concentration of cytosolic calcium in platelets. Although other PI3K isoforms have been shown to contribute the calcium response following stimulation of the collagen receptor, GPVI, this is mediated through another isoform of phospholipase C, PLCγ. It is speculated that PI3K-generated PIP3 binds to the PH domain of PLCγ and enhances its ability to anchor to the cell membrane.15,16,34,35 It is currently unknown whether PIP3 also influences the intracellular localization of PLCβ and directly regulates its activity.
A recent report by Poole and colleagues demonstrated that the P2Y12 receptor contributes to the ADP-stimulated calcium response in platelets through a pathway dependent on PI3K.36 We also observed a small but statistically significant defect in the calcium response in ADP-stimulated PI3Kγ platelets. At this point, we do not know whether PI3K isoforms other than PI3Kγ may also be required for this ADP-stimulated pathway.
The increase in the cytosolic calcium concentration in a stimulated platelet is due to a combination of calcium release from the dense tubular system and calcium influx across the plasma membrane. The influx across the cellular membrane is probably mediated by the ATP-regulated P2X1 purinergic receptor, the type III IP3 receptor, GAP1 IP4 receptor, as well as the receptors responsible for the calcium-induced calcium response (CICR).37,38 We found that most of the calcium flux in murine and human platelets was ablated when platelets were stimulated in the absence of extracellular calcium. This implies that the platelet calcium response could be highly dependent on secreted ATP that stimulates the P2X1 purinergic receptor. Alternatively, a small release of calcium from the sarcoplasmic reticulum could stimulate the receptors that control the calcium-induced calcium response. Thrombin-stimulated PLCβ2/β3-null platelets had no significant defect in secretion yet did show a defect in their ability to increase cytosolic calcium; this suggests that a receptor other than P2X1 mediates most of the calcium flux in thrombin-stimulated platelets.
Actin assembly in response to thrombin. Following stimulation of washed murine platelets with 1 U/mL thrombin, platelets were fixed, permeabilized, and stained with fluorescent phalloidin. Flow cytometry was used to quantitate phalloidin binding in 100 000 cells, and analysis was performed using CELLQuest software. Shown is the mean ± SEM for 3 experiments. Platelet actin assembly in response to thrombin requires PLCβ2/β3 (A) but does not require PI3Kγ (B).
Actin assembly in response to thrombin. Following stimulation of washed murine platelets with 1 U/mL thrombin, platelets were fixed, permeabilized, and stained with fluorescent phalloidin. Flow cytometry was used to quantitate phalloidin binding in 100 000 cells, and analysis was performed using CELLQuest software. Shown is the mean ± SEM for 3 experiments. Platelet actin assembly in response to thrombin requires PLCβ2/β3 (A) but does not require PI3Kγ (B).
Platelet spreading on immobilized fibrinogen. Washed platelets were layered at a density of 5 × 107/mL onto fibrinogen-coated slides. After several time points, cells were fixed and incubated with the membrane stain, vybrant DiO. Platelets lacking either PLCβ2β3 or PI3Kγ had impaired spreading compared with wild-type platelets. The spreading defect was most apparent at earlier time points. This demonstrates that second messengers generated by both PLCβ2β3 and PI3Kγ are required for platelet spreading. Results are representative for 3 experiments performed to date.
Platelet spreading on immobilized fibrinogen. Washed platelets were layered at a density of 5 × 107/mL onto fibrinogen-coated slides. After several time points, cells were fixed and incubated with the membrane stain, vybrant DiO. Platelets lacking either PLCβ2β3 or PI3Kγ had impaired spreading compared with wild-type platelets. The spreading defect was most apparent at earlier time points. This demonstrates that second messengers generated by both PLCβ2β3 and PI3Kγ are required for platelet spreading. Results are representative for 3 experiments performed to date.
Studies of growth factor–induced actin assembly have shown that PI3K is also essential for Rac-mediated actin reorganization in a variety of adherent tissue-culture cell lines. However, pharmacologic inhibition of PI3K by wortmannin does not appear to influence either barbed-end exposure or F-actin levels in thrombin-stimulated platelets. Our results showing normal F-actin assembly in thrombin-stimulated PI3Kγ knock-out platelets are consistent with these PI3K-inhibition studies.21 Interestingly, these platelets still fail to spread normally upon fibrinogen.
There are several potential explanations for why PI3Kγ–/– platelets fail to spread ex vivo. First, they might have a defect in ADP-mediated actin dynamics. Because ADP does not induce significant changes in F-actin levels in platelets that are stimulated in solution, we would not be able to detect such a defect using our flow cytometry assay. However, ADP may contribute to aspects of actin dynamics that are not important for actin assembly in solution but instead play key roles in platelet spreading. For example, it is conceivable that ADP augments integrin-directed actin changes. Second, PI3Kγ may be required for cytoskeletal events required for platelet spreading that are independent of actin assembly. This could potentially involve activation of myosin motors, regulation of platelet microtubules, or recruitment of cytoskeletal proteins toward the platelet membrane. The identification of platelet PI3K signaling cascades that contribute to cytoskeletal dynamics will require further study.
In conclusion, our study demonstrates considerable redundancy in the signaling pathways mediated by PLCβ and PI3Kγ that mediate secretion, calcium response, and aggregation. Despite small abnormalities in ex vivo assays, this work demonstrates clear in vivo phenotypes associated with the genetic loss of PLCβ and PI3Kγ. Because of the diminished ability of knock-out platelets to reorganize their cytoskeleton, their impaired spreading upon fibrinogen, and their inability to form stable thrombi in vivo, this work suggests that both PLCβ2/β3 and PI3Kγ play vital roles in platelet cytoskeletal dynamics.
Prepublished online as Blood First Edition Paper, February 10, 2005; DOI 10.1182/blood-2004-05-2005.
Supported in part by funds from the National Institutes of Health (NIH). L.L. and Y.W. contributed equally to this work.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 U.S.C. section 1734.


This feature is available to Subscribers Only
Sign In or Create an Account Close Modal