Abstract
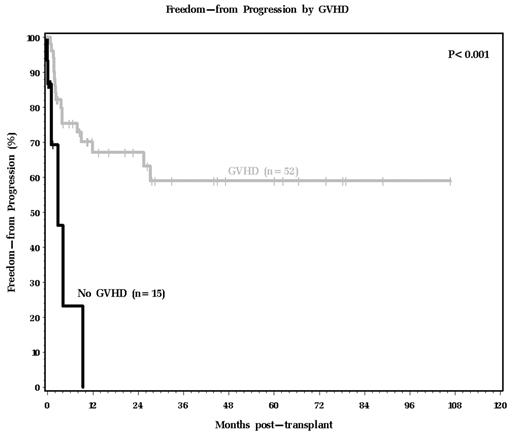
Non-myeloablative allogeneic stem cell transplantation (NMT) is increasingly used as an alternative to conventional bone marrow transplantation (BMT). Limited NMT data is available for lymphoma patients (pts). Most series include all hematological malignancies and only a minority with Hodgkin lymphoma (HL) or non-Hodgkin lymphoma (NHL). Therefore, we reviewed the Cleveland Clinic BMT Program experience with lymphoma pts and specifically compared the outcome between NMT and BMT. Between July 2, 1985 and December 7, 2004, 67 pts received a matched related (n=47) or unrelated (n=20) donor BMT (n=46) or NMT (n=21) for HL (n=11), aggressive NHL (n=32), indolent NHL (n=23), or unknown NHL (n=1). Pts with lymphoblastic, Burkitt, or atypical Burkitt-like lymphoma were excluded. Compared to BMT pts, NMT pts were older, had longer time from diagnosis to transplant (tx), and were more likely to have a normal LDH and be in remission (CR/PR) at tx. The median follow-up of surviving BMT and NMT pts was 73.8 (range 11.8–106.7) and 20.6 (range 2.8–44.0) months, respectively. 18 (39%) BMT and 5 (24%) NMT pts progressed, and 9 (20%) BMT and 2 (10%) NMT pts died from lymphoma. The incidence of grade 2–4 acute GVHD was not different between the BMT and NMT groups. Among all pts, the risk of lymphoma progression was significantly higher in pts with compared to pts without GVHD (Figure 1). The overall survival for NMT pts was significantly better than for BMT pts (P=.019). Among 15 pts that previously received high dose therapy with autologous stem cell transplant (ASCT), all 7 BMT pts died a median of 1 (range 1–14) month post-BMT while 4/8 NMT pts remained alive 8, 21, 29, and 33 months post-NMT. By multivariate analysis, BMT (HR 7.74, 95% CI 2.49–24.0, P<.001), HL (HR 6.52, 95% CI 2.04-20-85, P=.002), prior ASCT (HR 3.33, 95% CI 1.20–9.25, P=.021), and increasing age by decade (HR 1.7, 95% CI 1.11–2.62, P=0.14) were associated with a significantly higher mortality while CR/PR at tx was associated with a significantly lower mortality (HR 0.44, 95% CI 0.21–0.93, P=.032). Restricting the multivariate analysis to the 56 NHL pts identified no significant independent prognostic factors. Finally, excluding the 15 pts with prior ASCT showed that BMT, >3 prior chemotherapy regimens, tumor >10 cm at diagnosis, older age, and no remission at tx were all associated with a significantly higher mortality. We conclude that: 1) lymphoma progression and lymphoma- or transplant-related death beyond 2 years are uncommon; 2) BMT after failed ASCT is uniformly fatal while NMT (even after failed ASCT) may lead to long-term survival; 3) GVHD (with its presumed graft vs. lymhoma effect) is important for long-term, progression-free survival; 4) compared to BMT, NMT is associated with a better OS (although pt selection may account for some of the observed difference), and 5) both NMT and BMT are appropriate options for selected NHL pts. Whether NMT or BMT offers any benefit compared to ASCT for HL pts is unclear.
Author notes
Corresponding author

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal