Abstract
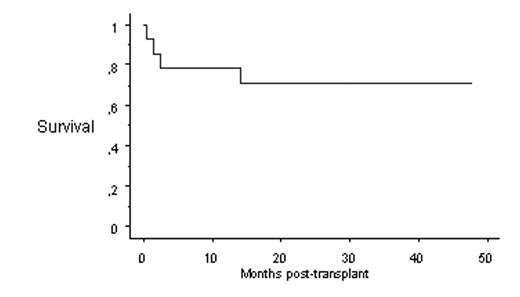
Survival after HSCT from HLA-identical siblings is inferior in SAA patients 30 years or older as compared with younger patients, with long-term overall survival of 58% and 80%, respectively (Bacigalupo et al, Semin in Hematol 2000). In order to improve survival in patients >30 years, the use of a less toxic regimen including low dose cyclophosphamide (<200 mg/kg) in combination with ATG, while adding fludarabine, might be an option to explore with the aim to reduce transplant-related mortality (Marsh et al, Br J Haematol, 2003). In order to evaluate the toxicity profile, engraftment potential, and efficacy of HLA-identical HSCT using such fludarabine-based conditioning regimen, we conducted this study from the SFGM-TC and GITMO databases, focussing on patients older than 30 years or those younger than 30 years but with co-morbidities at HSCT. From December 1998 to June 2004, 15 HSCT were performed in 14 patients (median age 39 years, range 16–60 years), for idiopathic SAA (n=13), or paroxysmal nocturnal hemoglobinuria (PNH) (n=1). HSCT was performed either as first-line treatment (n=8), or after failure of immune suppression with ATG/ciclosporine (CsA) (n=4), or failure of a first allogeneic HSCT (n=3). In addition to fludarabine (120 mg/m2) and ATG (3.75 mg/kg x 2 to 4 days), the patients received two different reduced doses of cyclophosphamide of 120 mg/kg (n=4) or 20 mg/kg (n=9). Two patients received only ATG and fludarabine (175 mg/m2) without cyclophosphamide. Marrow (n=12, median dose of nucleated cells 5.108/kg, range 2–15.108/kg) or PBSC (n=3) grafts were unmanipulated. GVHD prophylaxis consisted of CsA/methotrexate (n=11), CsA alone (n=1), methotrexate alone (n=1), or nothing (n=2 second grafts). Graft rejection occurred in one patient, who received a second graft from the same donor with the same conditioning regimen (fluda/ATG/cyclophosphamide 20 mg/kg) successfully. All other patients engrafted with a neutrophil (ANC >500 cells/μL) and platelet (PLT >50 000/μL) recovery occurring at a median of 18 days (range 12–28 days), and 26 days (range 11–272 days) after transplant, respectively. Acute GVHD occurred in 3 patients with a maximum grade II in 2 patients and grade III in one. Among 11 evaluable patients, six developed chronic GVHD (limited in 3 cases). Four patients died of infection (n=3) or multi-organ failure (n=1), within the 3 months post-HSCT for 3 of them. With a median follow-up of 28 months (range 11–48 months), 10/14 patients survived with long-term engraftment and full (n=8) or mixed (n=2) donor chimerism (KM probability of long-term survival 71%-see figure). In conclusion, reduced intensity fludarabine-based conditioning regimen is feasible in SAA patients over the age of 30 and produces encouraging survival: a prospective trial is being conducted within the European Group for Blood and Marrow Transplantation (EBMT).
Author notes
Corresponding author

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal