Abstract
Pre-transplant comorbidity can affect the outcome of allogeneic hematopoietic cell transplantation (HCT). The Seattle group recently proposed a new HCT-specific comorbidity index (HCT-CI) which was based on the Charlson Comorbidity Index (Blood, prepublished online, June 30, 2005).
To validate this scoring system, we retrospectively reviewed the medical records of 315 patients with hematologic malignancies who underwent allogeneic HCT after fludarabine-based reduced-intensity (n=160) or conventional (n=155) conditioning at our center between 2000 and 2004. The median age of the patients was 46 (range, 1–68) years. The diagnoses included acute myeloid leukemia or myelodysplastic syndrome (n=153), chronic myelogeneous leukemia (n=30), acute lymphoblastic leukemia (n=36), lymphoma (n=90), and other hematologic malignancies (n=6). Donors included HLA-matched (n=120) or mismatched (n=53) relatives and unrelated volunteers (n=142). Stem cell source was G-CSF-mobilized peripheral blood stem cell (n=169), bone marrow (n=117), or cord blood (n=29). We did not include the pulmonary function test results due to our inconsistency with the test.
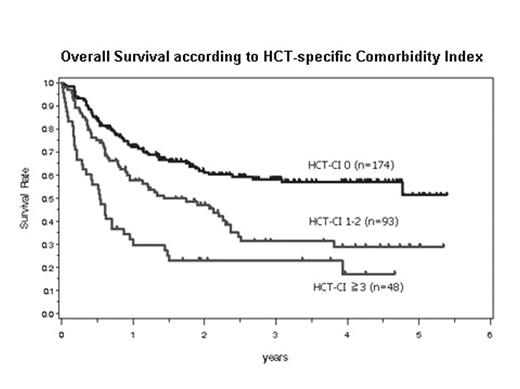
The HCT-CI captured 45% of patients with scores >0 (score 1, n=71; score 2, n=22; score 3, n=27; score 4, n=15; score >4, n=6). The capture rate of HCT-CI in patients who received reduced-intensity conditioning was higher than that in those who received conventional conditioning (51% vs 38%). The involved organ systems included hepatic (n=68), recent infection (n=38), prior malignancies (n=17), cardiac (n=16), renal (n=11), metabolic (n=11), psychiatric (n=11), pulmonary (n=8), and gastrointestinal (n=4) abnormalities. The Kaplan-Meier estimate of overall survival was significantly different among risk groups stratified according to HCT-CI (Figure 1, p<0.0001). In Cox proportional hazard models, a higher HCT-CI score, disease risk, and transplant from donors other than HLA-matched relatives were associated with poor overall survival. A higher HCT-CI score, greater patient age, and transplant from donors other than HLA-matched relatives were associated with a significantly increased risk for non-relapse mortality.
In conclusion, the new HCT-CI using pre-transplant variables was the most significant predictor of non-relapse mortality and survival after allografting. Our validation study suggests that this index will be a useful tool for future use in clinical trials and standard practice.
Overall Survival according to HCT-specific Comorbidity Index
Author notes
Corresponding author

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal