Abstract
We previously observed a loss of Epstein-Barr virus (EBV)–specific CD8+ T cells in subjects progressing to EBV-related non-Hodgkin lymphoma (NHL), correlating with loss of CD4+ T cells. The aim of the present study was to determine the role of EBV-specific CD4+ T cells in the development of NHL during chronic HIV infection. To this end, CD4+ and CD8+ memory T cells, capable of both proliferation and subsequent interferon γ (IFNγ) production, directed against a latent (Epstein-Barr virus nuclear antigen 1 [EBNA1]) and a lytic (BamH fragment Z left frame 1 [BZLF1]) EBV antigen were studied longitudinally in 9 progressors to NHL, 4 progressors to non–EBV-related AIDS, and 4 slow progressors to AIDS. In all 3 groups we observed a decline of EBV-specific memory CD4+ and CD8+ T-cell responses during HIV infection. However, whereas latent antigen EBNA1-specific CD4+ T cells were lost well before diagnosis in all subjects who developed an AIDS-related NHL (and EBNA1-specific CD8+ T cells were significantly lower compared with the other groups), these cells were better preserved in progressors to non–EBV-related disease and slow progressors. Loss of EBNA1-specific T-cell immunity thus might be important for progression to NHL. Interestingly, BZLF1-specific T cells were not lost in all progressors to NHL, suggesting a different function of these cells in the surveillance of EBV-infected B cells.
Introduction
The Epstein-Barr virus (EBV) is a widespread human γ-herpesvirus that persists for life in resting memory B cells after primary infection in the oropharynx.1,2 Both primary infection as well as subsequent reactivations of the virus and proliferation of EBV-infected B cells are controlled mainly by CD8+ T cells.3,4
In immunosuppressed individuals a combination of factors may lead to lymphoproliferative disorders.5,6 In HIV-infected subjects the risk of non-Hodgkin lymphoma (NHL) is 60- to 100-fold increased compared with the general population.7-9 Most of these lymphomas are large B-cell lymphomas of which 50% to 70% are EBV positive.10,11 While in HIV-infected individuals EBV-specific CD8+ T cells are generally well preserved,12,13 their ability to secrete interferon γ (IFNγ) in short-term antigen-specific stimulation assays is decreased, and in individuals progressing toward AIDS-related non-Hodgkin lymphoma the CD8+ T-cell function ultimately collapses completely.14 An association of this loss of CD8+ T-cell function with a decrease in total CD4+ T-cell numbers14 suggests that a lack of EBV-specific CD4+ T-cell help could play a role in disease progression. This would be in accordance with many human15-19 and animal studies20-26 that demonstrate the importance of CD4+ T cells in the development and maintenance of effective CD8+ T-cell responses.
While the importance of EBV-specific CD8+ T cells has been clearly demonstrated, and both the height and patterns of immunodominance of these CD8+ T-cell responses are clearly defined, to date few data on EBV-specific CD4+ T-cell responses are available. Due to the extremely low frequencies of these cells, only few investigators have been able to determine the ex vivo magnitude of the EBV-specific CD4+ T-cell response.27-29 Thus, its role for maintenance of control over latent EBV infection is unclear. In addition, the immunodominant targets of EBV-specific CD4+ T cells are not yet well defined, although it is clear that among the latent proteins Epstein-Barr virus nuclear antigen 1 (EBNA1) is recognized in a majority of EBV carriers.27,30 Regarding (early-phase) lytic antigens, which are known to be major targets of the CD8+ T-cell response,4,31,32 the antigens BamH fragment Z left frame 1 (BZLF1) and BamHI-M leftward reading frame 1 (BMLF1) are recognized during acute infectious mononucleosis,28 and a recent publication suggests that BamHI-M rightward reading frame 1 (BMRF1) might be a common target for CD4+ T cells.29
In order to study EBV-specific CD4+ T-cell responses, we used a recently developed method, enabling specific and reproducible in vitro expansion and restimulation of specific T cells with EBNA1 or BZLF1 peptide pools.33 Numbers of antigen-specific CD4+ central memory T cells, capable of proliferation and subsequently IFNγ production in response to re-exposure to antigen, were shown to correlate with protection against hepatitis C virus and malaria.17,34 We recently observed that for EBV this assay may provide a good indication of an individual's EBV-specific CD4+ memory T-cell response, as suggested by an inverse correlation with EBV load in a cross-sectional study.33 Here, we aimed to determine the role of EBV-specific CD4+ T-cell responses in the occurrence of NHL in the context of (untreated) HIV infection and its relation to the CD8+ T-cell response. We therefore performed a longitudinal follow-up of EBV-specific memory CD4+ and CD8+ T-cell responses in 9 HIV-infected subjects who developed EBV-positive NHL compared with progressors to non–EBV-related AIDS and slow progressors to AIDS.
Patients, materials, and methods
Patients
All HIV-seropositive subjects were participants of the Amsterdam Cohort studies on AIDS and HIV-1 infection. Blood samples from these homosexual men at risk for HIV-1 infection were collected every 3 months for HIV-1 serology and immunologic studies. In addition, at all time points peripheral blood mononuclear cells (PBMCs) were cryopreserved. All individuals under study gave their informed consent according to the Declaration of Helsinki.
Nine progressors to EBV-related NHL were studied longitudinally at several time points (3 to 8) from HIV seroconversion to NHL diagnosis. All the NHLs in this study were large B-cell systemic tumors, of which the EBV positivity was defined by positive EBV-encoded RNA (EBER) staining.11,12 These individuals were compared with 4 progressors to other AIDS-defining events and 4 subjects with slow progression of HIV disease. Time from HIV seroconversion to AIDS (NHL and non–EBV-related) or last time point of follow-up (slow progressors), CD4+ T-cell numbers, and HLA class I and II typing are indicated in Table 1. A number of individuals received antiretroviral treatment late during HIV infection (Table 1); however, we did not include any time points during this therapy. Two of the progressors to NHL received antiretroviral therapy before diagnosis (at 3 and 24 months before NHL, respectively), whereas 2 were treated by antiretroviral therapy from the date of NHL diagnosis onwards. Several of the individuals under study were described previously,14 as indicated in Table 1.
Patient data
Disease type and subject no. . | Age at SC or entry, y . | Follow-up, mo* . | HLA class I . | HLA class II . | CD4 T-cell number† . | Diagnosis . | Antiretroviral treatment‡ . |
|---|---|---|---|---|---|---|---|
| NHL | |||||||
| 68 | 43.5 | 12.4 | A29,A30,B18,B44 | DR7,DR14,DQ1,DQ2 | 850 | NHL | At 92 d before NHL (5, 6) |
| 139§ | 46.3 | 7.3 | A1,A2,B8,B51 | DR3,DR4,DQ2,DQ3, | 80 | NHL | — |
| 292 | 38.0 | 11.2 | A24,B16 | DRDR11,DR12,DQ3 | 210 | NHL | At diagnosis (1, 2, 5) |
| 308§ | 34.2 | 7.8 | A1,B8,B51 | DR1,DR17,DQ2,DQ5 | 100 | NHL | — |
| 354 | 35.2 | 6.1 | A1,A32,B7,B70 | DR4,DR15,DQ6,DQ7 | 30 | NHL | — |
| 434 | 48.9 | 13.1 | A2,A28,B7,B27 | DR6,DR9,DQ1 | 410 | NHL | 724 d before NHL (1, 5, 7) |
| 617 | 27.9 | 11.3 | A2,A11,B35,B62 | DR8,DR13,DQ1 | 390 | NHL | At diagnosis (5, 6, 7) |
| 6006§ | 41.8 | 6.3 | A2,A32,B7,B35 | DR11,DR17,DQ2,DQ7 | 50 | NHL | — |
| 8003 | 28.9 | 4.4 | ND | ND | 200 | NHL | — |
| Median | 38.0 | 7.8 | NA | NA | 200 | NA | NA |
| PROG | |||||||
| 53 | 27.3 | 7.1 | A1,A3,B39,B61 | DR1,DR11,DQ1,DQ3 | 140 | PCP | — |
| 232§ | 35.1 | 11.2 | A1,A3,B7,B8 | DR3,DQ2 | 150 | Mycobacteria | 3613 d after entry (3, 6, 7) |
| 341§ | 33.3 | 10.7 | A24,A28,B8,B13 | DR3,DR9,DQ2,DQ3 | 90 | PCP | 3533 d after SC (1, 5) |
| 495 | 37.6 | 4.6 | A1,B52,B60 | DR7,DR11,DQ1,DQ2 | 160 | Candida | — |
| Median | 34.2 | 8.9 | NA | NA | 145 | NA | NA |
| SP | |||||||
| 36§ | 34.9 | 9.3 | A1,A32,B8,B44 | DR3,DR12,DQ2,DQ3 | 450 | NA | 2224 d after SC (5, 6, 7) |
| 67 | 34.4 | 14.6 | A26,A28,B7,B57 | DR3,DR15,DQ2,DQ6 | 460 | NA | — |
| 750 | 31.7 | 17.6 | ND | ND | 380 | NA | — |
| 1160§ | 35.3 | 15.0 | A2,B8,B27 | DR,DR11,DQ2,DQ3 | 240 | NA | — |
| Median | 34.65 | 14.8 | NA | NA | 415 | NA | NA |
Disease type and subject no. . | Age at SC or entry, y . | Follow-up, mo* . | HLA class I . | HLA class II . | CD4 T-cell number† . | Diagnosis . | Antiretroviral treatment‡ . |
|---|---|---|---|---|---|---|---|
| NHL | |||||||
| 68 | 43.5 | 12.4 | A29,A30,B18,B44 | DR7,DR14,DQ1,DQ2 | 850 | NHL | At 92 d before NHL (5, 6) |
| 139§ | 46.3 | 7.3 | A1,A2,B8,B51 | DR3,DR4,DQ2,DQ3, | 80 | NHL | — |
| 292 | 38.0 | 11.2 | A24,B16 | DRDR11,DR12,DQ3 | 210 | NHL | At diagnosis (1, 2, 5) |
| 308§ | 34.2 | 7.8 | A1,B8,B51 | DR1,DR17,DQ2,DQ5 | 100 | NHL | — |
| 354 | 35.2 | 6.1 | A1,A32,B7,B70 | DR4,DR15,DQ6,DQ7 | 30 | NHL | — |
| 434 | 48.9 | 13.1 | A2,A28,B7,B27 | DR6,DR9,DQ1 | 410 | NHL | 724 d before NHL (1, 5, 7) |
| 617 | 27.9 | 11.3 | A2,A11,B35,B62 | DR8,DR13,DQ1 | 390 | NHL | At diagnosis (5, 6, 7) |
| 6006§ | 41.8 | 6.3 | A2,A32,B7,B35 | DR11,DR17,DQ2,DQ7 | 50 | NHL | — |
| 8003 | 28.9 | 4.4 | ND | ND | 200 | NHL | — |
| Median | 38.0 | 7.8 | NA | NA | 200 | NA | NA |
| PROG | |||||||
| 53 | 27.3 | 7.1 | A1,A3,B39,B61 | DR1,DR11,DQ1,DQ3 | 140 | PCP | — |
| 232§ | 35.1 | 11.2 | A1,A3,B7,B8 | DR3,DQ2 | 150 | Mycobacteria | 3613 d after entry (3, 6, 7) |
| 341§ | 33.3 | 10.7 | A24,A28,B8,B13 | DR3,DR9,DQ2,DQ3 | 90 | PCP | 3533 d after SC (1, 5) |
| 495 | 37.6 | 4.6 | A1,B52,B60 | DR7,DR11,DQ1,DQ2 | 160 | Candida | — |
| Median | 34.2 | 8.9 | NA | NA | 145 | NA | NA |
| SP | |||||||
| 36§ | 34.9 | 9.3 | A1,A32,B8,B44 | DR3,DR12,DQ2,DQ3 | 450 | NA | 2224 d after SC (5, 6, 7) |
| 67 | 34.4 | 14.6 | A26,A28,B7,B57 | DR3,DR15,DQ2,DQ6 | 460 | NA | — |
| 750 | 31.7 | 17.6 | ND | ND | 380 | NA | — |
| 1160§ | 35.3 | 15.0 | A2,B8,B27 | DR,DR11,DQ2,DQ3 | 240 | NA | — |
| Median | 34.65 | 14.8 | NA | NA | 415 | NA | NA |
SC indicates seroconversion; —, no antiretroviral treatment; ND, not done; PROG, progressor; PCP, Pneumocystis carinii pneumonia; SP, slow progressor; and NA, not applicable.
Time from entry or seroconversion to AIDS diagnosis or last time point of follow-up (for the slow progressors)
CD4 count at AIDS diagnosis or at least time point studied (slow progressors)
Antiretroviral therapy: 1 indicates zidovudine (zdv); 2, didanosine (ddI); 3, zalcitabine (ddC); 5, lamuvidine (3TC); 6, indinavir; and 7, saquinavir (HGC)
Individuals included in a previous study14
T-cell stimulation
EBV-specific CD4+ T cells were stimulated using overlapping peptide pools. Fifteen-mer peptides with 11–amino acid overlap spanning the immunogenic C-terminal region of EBNA1 (57 peptides) and the entire BZLF1 protein (59 peptides) were synthesized by Jerini AG (Berlin, Germany). Purity and sequences were verified by high-performance liquid chromatography (HPLC) and mass spectrometry. Peptides were dissolved in dimethyl sulfoxide (DMSO) and pooled at a final concentration of 1 mg/mL of each peptide. As a negative control, PBMCs were stimulated with medium and costimulated alone. As a positive control, PBMCs were stimulated with 10 ng/mL phorbol myristate acetate (PMA) and 2 μg/mL ionomycin.
Expansion of EBV-specific T cells
To expand EBV-specific T cells, PBMCs were cultured for 12 days in the presence of EBNA1 or BZLF1 peptide pool. The culture medium consisted of RPMI 1640 (Gibco, Life Technologies, Breda, The Netherlands) supplemented with penicillin/streptomycin and 10% human pool serum. Cells were cultured at 2 × 105 PBMCs/well in 100 μL medium in 96 round-bottom plates at 37°C and 5% CO2. Peptide pool (at 2 μg/mL of each peptide) was added on days 0 and 6. Interleukin 2 (IL2) was added at 10 U/mL on days 3, 6, and 9. On day 12 cells were pooled, washed in RPMI, and rested overnight in complete medium. On day 13 cells were restimulated for 6 hours using the protocol indicated in “Detection of IFNγ-producing EBV-specific T cells.”
Detection of IFNγ-producing EBV-specific T cells
After stimulation with overlapping peptide pools IFNγ-producing cells were enumerated by intracellular cytokine staining (ICCS).14,35,36 Briefly, 1 × 106 PBMCs were restimulated in 500 μL medium containing 10% human pool serum for 6 hours (after expansion in culture) with EBNA1 or BZLF1 peptide pools (at 2 μg/mL of each peptide) and both αCD28 (2 μg/mL) and αCD49d (1 μg/mL) as costimuli, in the presence of 1:1000 brefeldin A (Golgiplug; Becton Dickinson [BD], San José, CA) after 1 hour to allow accumulation of cytokines in the cytosol. After stimulation, cells were washed in phosphate-buffered saline (PBS), permeabilized (FACS Permeabilizing Solution; BD), washed again, and stained with antibodies specific for CD3 peridinin chlorophyll A protein (PerCP), CD4 allophycocyanin (APC), CD8 phycoerythrin (PE), and IFNγ fluorescein isothiocyanate (FITC; BD). Cells were washed again, fixed (Cellfix; BD), and 200 000 events were acquired on a FACSCalibur flow cytometer (BD). Lymphocytes were gated by forward and sideward scatter and data analyzed using CELL Quest software (BD). Instead of using the percentage of IFNγ-producing cells within the CD3+CD4+ or CD8+ T-cell fractions, we aimed to determine a more absolute number of EBV-specific CD4+ T cells, enabling comparison of donors and patients with very different CD4+ T-cell numbers and reflecting the proliferative capacity of the specific cells. Therefore, we calculated the number of EBNA1- or BZLF1-specific IFNγ-producing CD4+ T cells recovered out of 106 cultured PBMCs (by compensating for the total recovery of cells at day 12). Responses were defined as positive when they were more than 2 times the medium levels of IFNγ production, which generally gave a cutoff around 0.10% or 100 specific cells grown out of 106 PBMCs put into culture.
Polyclonal T-cell proliferation
Polyclonal T-cell proliferation was determined by measurement of 3H thymidine incorporation after stimulation of whole-blood cultures with the anti-CD3 monoclonal antibody (mAb) CLB T3/4 (Sanquin Reagents, Amsterdam, the Netherlands), as previously described.37
Real-time quantitative PCR assay for measurement of EBV load in PBMCs
EBV load was measured in duplicate in DNA from 2 × 105 cells. Real-time polymerase chain reaction (PCR) amplification was performed as previously described,38,39 using PCR primers specific for the nonglycosylated membrane protein BNRF1 p14340 and using a fluorogenic probe (PE Biosystems, Nieuwekerk aan de IJssel, the Netherlands) to detect the 74–base pair product. As a control for input DNA the amount of β-albumin DNA, a household gene present at 2 copies/cell, was also determined using primers and probes as described before.41
Statistical analysis
For comparison of EBV-specific T-cell numbers between different groups, Mann-Whitney tests were used. For comparison of time points within groups, Wilcoxon signed rank test was used. Correlations were calculated using Spearman correlation tests. Software program SPSS 11.5 for Windows was used (SPSS, Chicago, IL).
Results
Study population
We studied 9 subjects who progressed to an EBV-positive AIDS-related NHL within a median of 7.8 years from HIV seroconversion, 4 subjects who progressed to other AIDS-defining events within a median time of 8.9 years from HIV seroconversion, and 4 slow progressors who did not develop any AIDS-defining symptoms during a median time of at least 14.8 years. The selection was based on availability of samples and inclusion of patients in a previous study. As no samples were available from EBV-negative NHLs (such as Burkitt) in this cohort, progressors to other non–EBV-related AIDS-defining events with similar CD4+ T-cell decline were chosen. The median age of the patients at seroconversion was not different between the progressors to NHL (39.9 years), the progressors to AIDS opportunistic infections (OIs; 34.2 years), and the slow progressors (34.7 years). Median CD4+ T-cell numbers at AIDS diagnosis were similar (P = .71) between progressors to NHL (200/μL, range 30-850/μL) and other progressors (145/μL, range 90-160/μL), although the range was much wider for the NHL patients. A number of the individuals under study received antiretroviral treatment late during follow-up (at time points not included in this study), as indicated in Table 1. Confirming our earlier studies,14,39,42 EBV DNA load in PBMCs was not different at any time point during follow-up between progressors to NHL and slow progressors or progressors to non–EBV-related AIDS (Figure 1).
Kinetics of EBV-specific memory T-cell responses during chronic HIV infection
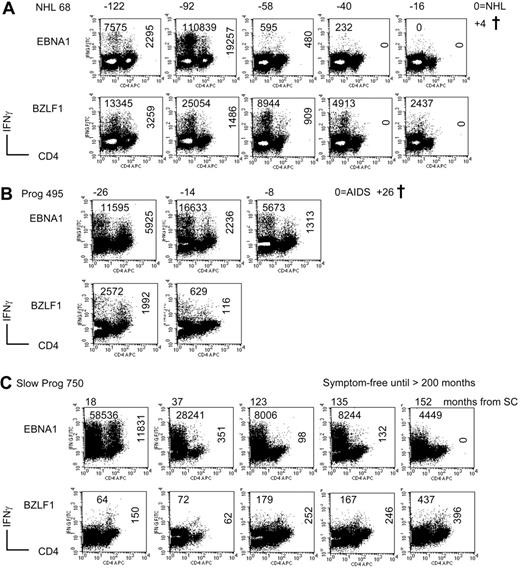
EBV-specific memory CD4+ and CD8+ T-cell responses were studied using a recently developed method, enabling specific and reproducible in vitro expansion and restimulation of specific T cells with EBNA1 or BZLF1 peptide pools.33 The results of this assay were expressed as the number of IFNγ-producing cells, after restimulation, per 106 PBMCs put into culture at day 0. This value gives an indication of both proliferative capacity and ability to produce IFNγ after antigen-driven expansion. Figure 2A shows a subject who progressed to NHL in whom initially both CD4+ and CD8+ T-cell responses to EBNA1 and BZLF1 were detected. The CD4+ T cells to both EBNA1 and BZLF1 were lost already 40 months before NHL diagnosis. CD8+ T-cell responses to EBNA1 disappeared 16 months before NHL, whereas BZLF1-specific CD8+ T cells were detected until the end of follow-up. Figure 2B shows a progressor to AIDS (Candida esophagitis) who initially had a high CD4+ and CD8+ T-cell response to EBNA1 and BZLF1, which declined but was detectable until AIDS diagnosis. In Figure 2C, a representative slow progressor is shown who lost EBNA1-specific CD4+ T cells at more than 150 months after HIV seroconversion but had a sustained EBNA1-specific CD8+ T-cell response and a low but stable BZLF1-specific CD4+ T-cell response.
Comparable EBV load in NHL and other progressors or slow progressors. EBV DNA load in PBMCs (depicted in copies per 106 PBMCs) as measured by TaqMan real-time PCR of the BNRF1 gene at 6, 3, and 1 years before AIDS diagnosis (NHL and other progressors) or equivalent time from HIV seroconversion (slow progressors). • indicates progressors to NHL or other AIDS; and  , slow progressors. Values above the graphs indicate median EBV load levels of NHL versus progressors and slow progressors (P+SP) and the P value of the Mann-Whitney test.
, slow progressors. Values above the graphs indicate median EBV load levels of NHL versus progressors and slow progressors (P+SP) and the P value of the Mann-Whitney test.
Comparable EBV load in NHL and other progressors or slow progressors. EBV DNA load in PBMCs (depicted in copies per 106 PBMCs) as measured by TaqMan real-time PCR of the BNRF1 gene at 6, 3, and 1 years before AIDS diagnosis (NHL and other progressors) or equivalent time from HIV seroconversion (slow progressors). • indicates progressors to NHL or other AIDS; and  , slow progressors. Values above the graphs indicate median EBV load levels of NHL versus progressors and slow progressors (P+SP) and the P value of the Mann-Whitney test.
, slow progressors. Values above the graphs indicate median EBV load levels of NHL versus progressors and slow progressors (P+SP) and the P value of the Mann-Whitney test.
Decline in EBV-specific CD4+ and CD8+ memory T cells during HIV infection. Examples of EBNA1- and BZLF1-specific T-cell responses during the course of HIV infection, measured after 12 days of specific in vitro expansion. Panel A represents a subject who progressed to an EBV-related NHL, panel B represents an individual who progressed to non–EBV-related AIDS (Candida esophagitis), and panel C represents a slow progressor (asymptomatic for more than 17 years). Values in the top left corner indicate the number of CD8+ T cells that grew out of 106 PBMCs put into culture (after substraction of the medium background), whereas the vertical values in the right part of the plots indicate the number of specific CD4+ T cells. The values above the plots indicate the follow-up time in months relative to NHL or AIDS or to HIV seroconversion for the slow progressor. † indicates death; Prog, progressor; and SC, seroconversion.
Decline in EBV-specific CD4+ and CD8+ memory T cells during HIV infection. Examples of EBNA1- and BZLF1-specific T-cell responses during the course of HIV infection, measured after 12 days of specific in vitro expansion. Panel A represents a subject who progressed to an EBV-related NHL, panel B represents an individual who progressed to non–EBV-related AIDS (Candida esophagitis), and panel C represents a slow progressor (asymptomatic for more than 17 years). Values in the top left corner indicate the number of CD8+ T cells that grew out of 106 PBMCs put into culture (after substraction of the medium background), whereas the vertical values in the right part of the plots indicate the number of specific CD4+ T cells. The values above the plots indicate the follow-up time in months relative to NHL or AIDS or to HIV seroconversion for the slow progressor. † indicates death; Prog, progressor; and SC, seroconversion.
Decline of EBV-specific CD4+ T cells during chronic HIV infection: loss of EBNA1-specific CD4+ T cells in all progressors to EBV-related NHL
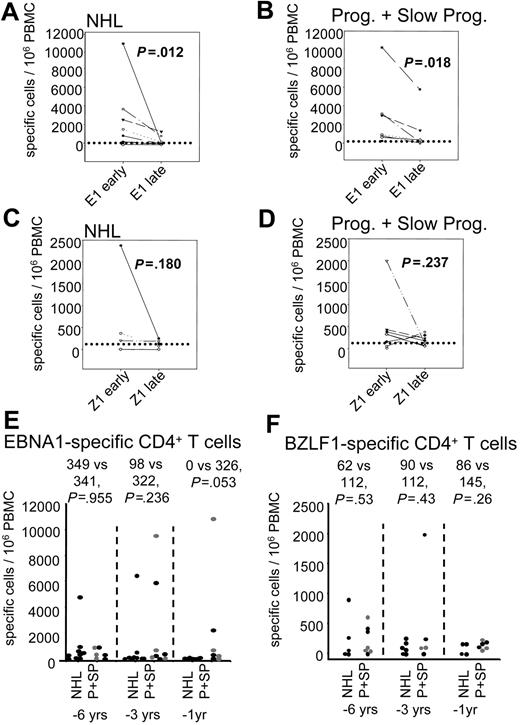
To study the evolution of EBV-specific memory CD4+ T-cell responses within the different groups of individuals, we calculated the median of the responses early (defined as > 200 CD4+ T cells per μL, or in the first half of follow-up when CD4+ T cells did not decline to such low levels) and late in infection. As shown in Figure 3A-B, EBNA1-specific CD4+ T-cell responses declined significantly in all HIV-infected individuals during HIV infection, from a median of 498 to 105 specific cells out of 106 PBMCs for the NHL (P = .012; Wilcoxon signed rank test) and from 846 to 343 for the progressors to AIDS and slow progressors (P = .018). BZLF1-specific CD4+ T-cell responses (Figure 3C-D), which were measured only in a proportion of individuals (Table 2), were not altered (P = .180 and .237).
Presence of EBNA1- and BZLF1-specific memory T cells
. | NHL present early* . | Detectable till end of follow-up† . | CD4 at time of loss‡ . | Progressor present early* . | Detectable till end of follow-up† . | CD4 at time of loss‡ . | Slow progressor present early* . | Detectable till end of follow-up† . | CD4 at time of loss‡ . |
|---|---|---|---|---|---|---|---|---|---|
| EBNA1-CD4 | 7/9 | 0/7 | 300 | 4/4 | 2/4 | 290 | 4/4 | 1/4 | 280 |
| BZLF1-CD4 | 4/8 | 1/4 | 310 | 3/3 | 2/3 | 290 | 4/4 | 1/4 | 360 |
| EBNA1-CD8 | 4/9 | 2/4 | 385 | 3/4 | 2/3 | 280 | 3/4 | 2/3 | 280 |
| BZLF1-CD8 | 6/8 | 6/6 | ND | 3/4 | 3/3 | ND | 3/4 | 2/3 | 280 |
. | NHL present early* . | Detectable till end of follow-up† . | CD4 at time of loss‡ . | Progressor present early* . | Detectable till end of follow-up† . | CD4 at time of loss‡ . | Slow progressor present early* . | Detectable till end of follow-up† . | CD4 at time of loss‡ . |
|---|---|---|---|---|---|---|---|---|---|
| EBNA1-CD4 | 7/9 | 0/7 | 300 | 4/4 | 2/4 | 290 | 4/4 | 1/4 | 280 |
| BZLF1-CD4 | 4/8 | 1/4 | 310 | 3/3 | 2/3 | 290 | 4/4 | 1/4 | 360 |
| EBNA1-CD8 | 4/9 | 2/4 | 385 | 3/4 | 2/3 | 280 | 3/4 | 2/3 | 280 |
| BZLF1-CD8 | 6/8 | 6/6 | ND | 3/4 | 3/3 | ND | 3/4 | 2/3 | 280 |
ND indicates not done.
Frequency of individuals in whom these responses were measurable at an early time point during HIV/total number of individuals tested
Frequency of individuals in whom these responses were maintained until end of follow-up/total individuals tested
Total CD4+ T-cell numbers per μL at time point when memory T-cell responses were lost
In order to compare the responses between groups, we choose 3 different time points during follow-up, at which we had data from a majority of subjects, in relation to the date of AIDS diagnosis or the equivalent median time from study entry or seroconversion (for the slow progressors). These results are shown in Figure 3E for EBNA1 and Figure 3F for BZLF1. At 6 years (range, 40-75 months) and 3 years (range, 26-45 months) before AIDS diagnosis, the numbers of EBNA1-specific CD4+ T cells were not different between NHL and other patients (at 6 years, 349 vs 341, P = .681; at 3 years, 98 vs 322, P = .236; Mann-Whitney test; Figure 3E). In contrast, at 1 year (range, 7-20 months) before AIDS, EBNA1-specific CD4+ T-cell responses were not detectable in the NHL patients, whereas they were still present in 2 of 3 progressors and 3 of 4 slow progressors (0 vs 326, P = .053; Figure 3E). For BZLF1-specific CD4+T-cell responses, no differences between the groups were found at any time point (Figure 3F).
Eventually, EBNA1-specific CD4+ T cells were lost in all progressors to NHL (Table 2). The median CD4+ T-cell number at time of loss (first time point at which no response was detected) was 300 per μL. In contrast, EBNA1-specific CD4+ T cells were maintained in 2 of 4 progressors (whereas 2 progressors lost this response at total CD4+ T-cell numbers of 290/μL), and 1 of 4 slow progressors maintained this response until the end of follow-up (3/4 others lost it at a median of 280 CD4+ T cells/μL). At the end of follow-up, BZLF1-specific CD4+ T cells were maintained in 1 of 4 progressors to NHL (3/4 lost these cells at median CD4 counts of 360/μL), 2 of 3 other progressors (1 lost them at CD4 count of 290/μL), and 1 of 4 slow progressors (3/4 lost this response at CD4 counts of 360/μL; Table 2). Thus, it appears that EBNA1-specific CD4+ T cells were specifically lost in the progressors to NHL.
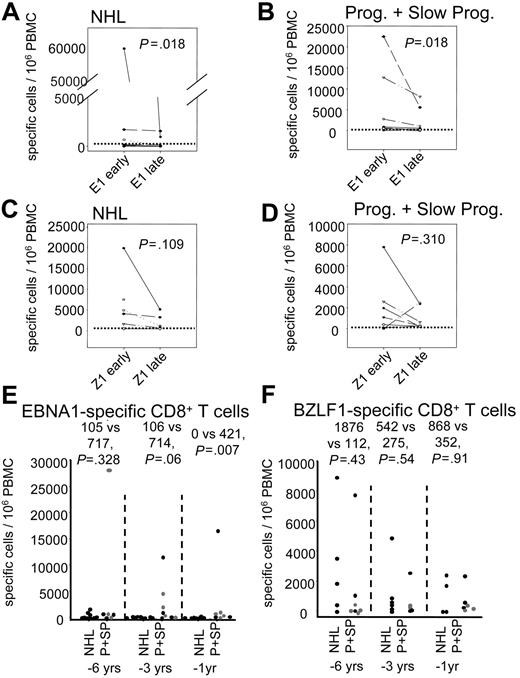
Lower EBNA1-specific CD8+ T cells in the progressors to NHL
As shown in Figure 2A-C, CD8+ T-cell responses measured after 12 days of specific expansion also declined during HIV infection. In parallel to CD4+ T cells, CD8+ T-cell responses to EBNA1 declined significantly (P = .018 for NHL and P = .018 for progressors and slow progressors; Figure 4A-B), whereas BZLF1-specific CD8+ T-cell responses did not change (P = .109 and P = .310; Figure 4C-D).
CD4+ T-cell responses to EBNA1 and BZLF1. CD4+ T-cell responses to EBNA1 (E1; A-B,E) and BZLF1 (Z1; C-D,F) after 12 days of specific expansion and restimulation. Results are expressed as the number of IFNγ-producing cells after specific restimulation at day 12 that grew out of 106 PBMCs put into culture at day 0. Panels A-D show the responses early (CD4+ T-cell numbers > 200/μL, or first half of the follow-up time) and late during HIV infection for progressors to NHL (A,C) and progressors to AIDS and slow progressors together (B,D). The P values of the Wilcoxon signed rank test are indicated above the graphs. Panels E-F show the comparison of progressors to NHL (NHL) with progressors and slow progressors (P+SP) at 6, 3, and 1 years before AIDS diagnosis. Values above the graphs indicate median of NHL versus P+SP and the P value of the Mann-Whitney test. In panels E-F, • indicates progressor to NHL or other AIDS; and  , slow progressors. The horizontal dotted line indicates the detection limit.
, slow progressors. The horizontal dotted line indicates the detection limit.
CD4+ T-cell responses to EBNA1 and BZLF1. CD4+ T-cell responses to EBNA1 (E1; A-B,E) and BZLF1 (Z1; C-D,F) after 12 days of specific expansion and restimulation. Results are expressed as the number of IFNγ-producing cells after specific restimulation at day 12 that grew out of 106 PBMCs put into culture at day 0. Panels A-D show the responses early (CD4+ T-cell numbers > 200/μL, or first half of the follow-up time) and late during HIV infection for progressors to NHL (A,C) and progressors to AIDS and slow progressors together (B,D). The P values of the Wilcoxon signed rank test are indicated above the graphs. Panels E-F show the comparison of progressors to NHL (NHL) with progressors and slow progressors (P+SP) at 6, 3, and 1 years before AIDS diagnosis. Values above the graphs indicate median of NHL versus P+SP and the P value of the Mann-Whitney test. In panels E-F, • indicates progressor to NHL or other AIDS; and  , slow progressors. The horizontal dotted line indicates the detection limit.
, slow progressors. The horizontal dotted line indicates the detection limit.
When comparing responses at different time points before AIDS there was no difference in the EBNA1-specific CD8+ T-cell response between NHL and other subjects at 6 years before AIDS (105 vs 717 cells out of 106 PBMCs; P = .328), whereas they tended to decrease at 3 years (106 vs 714 cells out of 106 PBMCs; P = .059) and were significantly lower in the NHL patients at 1 year before AIDS diagnosis (0 vs 421 cells out of 106 PBMCs; P = .007; Figure 4E). For BZLF1, no difference was found at any of those time points (6 years before AIDS: 1876 vs 112, P = .432; at 3 years: 542 vs 275, P = .537; at 1 year: 868 vs 352, P = .914; Figure 4F).
EBV-specific CD8+ T-cell responses. CD8+ T-cell responses to EBNA1 (A-B,E) and BZLF1 (C-D,F) after 12 days of specific expansion and restimulation. Results are expressed as the number of IFNγ-producing cells after specific restimulation at day 12 that grew out of 106 PBMCs put into culture at day 0. Panels A-D show the responses early (CD4+ T-cell numbers > 200/μL, or before half of the follow-up time) and late during HIV infection for progressors to NHL (A,C) and progressors to AIDS and slow progressors together (B,D). The P values of the Wilcoxon signed rank test are indicated above the graphs. Panels E-F show the comparison of progressors to NHL (NHL) with progressors and slow progressors (P+SP) at 6, 3, and 1 years before AIDS diagnosis. Values above the graphs indicate median of NHL versus P+SP and the P value of the Mann-Whitney test. In panels E-F, • indicates progressor to NHL or other AIDS; and  , slow progressors. The horizontal dotted line indicates the detection limit.
, slow progressors. The horizontal dotted line indicates the detection limit.
EBV-specific CD8+ T-cell responses. CD8+ T-cell responses to EBNA1 (A-B,E) and BZLF1 (C-D,F) after 12 days of specific expansion and restimulation. Results are expressed as the number of IFNγ-producing cells after specific restimulation at day 12 that grew out of 106 PBMCs put into culture at day 0. Panels A-D show the responses early (CD4+ T-cell numbers > 200/μL, or before half of the follow-up time) and late during HIV infection for progressors to NHL (A,C) and progressors to AIDS and slow progressors together (B,D). The P values of the Wilcoxon signed rank test are indicated above the graphs. Panels E-F show the comparison of progressors to NHL (NHL) with progressors and slow progressors (P+SP) at 6, 3, and 1 years before AIDS diagnosis. Values above the graphs indicate median of NHL versus P+SP and the P value of the Mann-Whitney test. In panels E-F, • indicates progressor to NHL or other AIDS; and  , slow progressors. The horizontal dotted line indicates the detection limit.
, slow progressors. The horizontal dotted line indicates the detection limit.
At AIDS diagnosis or end of follow-up, EBNA1-specific CD8+ T cells were maintained at low levels in 2 of 4 of the progressors to NHL who initially responded (lost in 2/4 at total CD4+ T-cell numbers of 385/μL), in 2 of 3 other progressors (lost in 1/3 at CD4+ T-cell numbers of 280/μL), and in 2 of 3 slow progressors (lost in 1/3 at CD4+ T-cell numbers of 280/μL; Table 2). BZLF1-specific CD8+ T cells were maintained in all 6 responding progressors to NHL and 3 of 3 responders among the other progressors, whereas they were lost in 1 of 3 responding slow progressors at CD4+ T-cell numbers of 280/μL (Table 2).
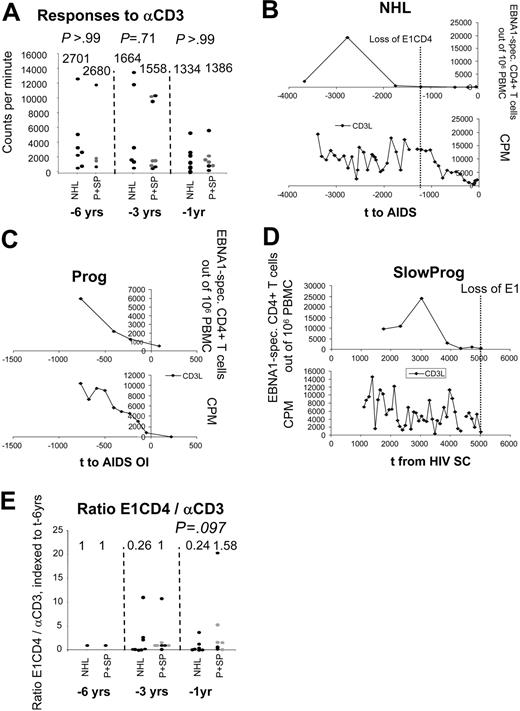
EBNA1-specific CD4+ T-cell proliferation is specifically lost
To investigate whether loss of EBNA1-specific T cells is specific or a consequence of general loss of T-cell proliferative capacity, we investigated the general proliferative capacity of T cells, as measured by proliferative responses to CD3 mAb37 at 6, 3, and 1 years before AIDS diagnosis (the same time points as used for comparison of specific responses between groups). As shown in Figure 5A, progressors to NHL did not differ from other progressors and slow progressors with regard to T-cell proliferative responses to CD3 (at 6 years before AIDS: median 2701 vs 2680 counts per minute; at 3 years: 1684 vs 1558; at 1 year 1334 vs 1386). This further confirmed that indeed EBNA1-specific T cells were specifically lost in subjects who developed NHL. To illustrate this, Figure 5B shows a progressor to NHL in whom the CD4+ T-cell response to EBNA1 was lost before CD3 responses declined. In contrast, Figures 5C and 5D show a progressor to non–EBV-related AIDS and a slow progressor, respectively, in whom the decline in EBNA1-specific CD4+ T cells paralleled the decline in proliferation to CD3 mAb. In accordance with a specific loss of CD4+ T-cell responses to EBNA1, the ratio between EBNA1-specific CD4+ T-cell responses and proliferative responses to CD3 mAb tended to be lower in the progressors to NHL (ratio = 0.24, arbitrary units, indexed to 1 at 6 years before AIDS) compared with the progressors to AIDS and slow progressors (ratio = 1.58), at 1 year before AIDS diagnosis (P = .097; Figure 5E). No correlations were found between the proliferative response to CD3 mAb and memory CD4+ T-cell responses to EBNA1 or BZLF1 in the progressors to NHL (Rho = 0.190, P = .385 for EBNA1; Rho = 0.260, P = .370 for BZLF1; Spearman correlation test) or in the other subjects (Rho = 0.479, P = .192 for EBNA1; Rho = 0.373, P = .362 for BZLF1). Thus, loss of EBNA1-specific memory T-cell responses occurs specifically during progression to EBV-related NHL.
EBV-specific T-cell responses in relation to polyclonal proliferative capacity. Panel A indicates the proliferative response to αCD3 mAb expressed in counts per minute (CPM) at 6, 3, and 1 years before NHL or AIDS. • indicates progressors to NHL (NHL) or other AIDS (P); and  , slow progressors (SP). The P value of the Mann-Whitney test is given above the graphs. Panels B-D give representative examples of the CD4+ T-cell response to EBNA1 and BZLF1 for a progressor to NHL (B; in whom the responses to EBNA1 and BZLF1 were lost before loss of the response to αCD3), a progressor to AIDS (C; in whom the BZLF1-specific response was lost early and EBNA1-specific response parallels the αCD3 response), and a slow progressor (D; in whom no response to BZLF1 was measured and the EBNA1-specific response decreased in parallel with the αCD3 response). Panel E shows the ratio between EBNA1-specific CD4+ T-cell responses and general proliferative capacity (in response to αCD3 mAb) indexed to the time point at 6 years before AIDS diagnosis.
, slow progressors (SP). The P value of the Mann-Whitney test is given above the graphs. Panels B-D give representative examples of the CD4+ T-cell response to EBNA1 and BZLF1 for a progressor to NHL (B; in whom the responses to EBNA1 and BZLF1 were lost before loss of the response to αCD3), a progressor to AIDS (C; in whom the BZLF1-specific response was lost early and EBNA1-specific response parallels the αCD3 response), and a slow progressor (D; in whom no response to BZLF1 was measured and the EBNA1-specific response decreased in parallel with the αCD3 response). Panel E shows the ratio between EBNA1-specific CD4+ T-cell responses and general proliferative capacity (in response to αCD3 mAb) indexed to the time point at 6 years before AIDS diagnosis.
EBV-specific T-cell responses in relation to polyclonal proliferative capacity. Panel A indicates the proliferative response to αCD3 mAb expressed in counts per minute (CPM) at 6, 3, and 1 years before NHL or AIDS. • indicates progressors to NHL (NHL) or other AIDS (P); and  , slow progressors (SP). The P value of the Mann-Whitney test is given above the graphs. Panels B-D give representative examples of the CD4+ T-cell response to EBNA1 and BZLF1 for a progressor to NHL (B; in whom the responses to EBNA1 and BZLF1 were lost before loss of the response to αCD3), a progressor to AIDS (C; in whom the BZLF1-specific response was lost early and EBNA1-specific response parallels the αCD3 response), and a slow progressor (D; in whom no response to BZLF1 was measured and the EBNA1-specific response decreased in parallel with the αCD3 response). Panel E shows the ratio between EBNA1-specific CD4+ T-cell responses and general proliferative capacity (in response to αCD3 mAb) indexed to the time point at 6 years before AIDS diagnosis.
, slow progressors (SP). The P value of the Mann-Whitney test is given above the graphs. Panels B-D give representative examples of the CD4+ T-cell response to EBNA1 and BZLF1 for a progressor to NHL (B; in whom the responses to EBNA1 and BZLF1 were lost before loss of the response to αCD3), a progressor to AIDS (C; in whom the BZLF1-specific response was lost early and EBNA1-specific response parallels the αCD3 response), and a slow progressor (D; in whom no response to BZLF1 was measured and the EBNA1-specific response decreased in parallel with the αCD3 response). Panel E shows the ratio between EBNA1-specific CD4+ T-cell responses and general proliferative capacity (in response to αCD3 mAb) indexed to the time point at 6 years before AIDS diagnosis.
Discussion
It was previously shown that dysfunctional EBV-specific CD8+ T cells may be a major cause for the development of NHL in HIV-infected subjects.12,14 To investigate whether this could be related to loss of specific CD4+ T-cell help we studied EBV-specific CD4+ T cells in both progressors to AIDS-related NHL and progressors to AIDS or slow progressors. Confirming our earlier cross-sectional results,33 where we found a decreased frequency of EBV-specific memory CD4+ and CD8+ T cells in untreated HIV-infected subjects, we observed a decline in these responses during HIV infection in both progressors to NHL and progressors to non–EBV-related AIDS or slow progressors. However, while latent antigen EBNA1-specific CD4+ T cells were lost well before diagnosis in all the subjects who developed an EBV-related NHL, these were relatively preserved in progressors to non–EBV-related disease and slow progressors. Loss of EBNA1-specific T-cell immunity may thus be a factor that increases the chance of development of an EBV-positive lymphoma growing out. Interestingly, BZLF1-specific T cells were maintained in progressors to NHL, suggesting a less important function of these cells in the surveillance of EBV-infected B cells.
As EBV-specific CD4+ T cells are present in very low numbers during latent EBV infection,27,28 we used a specific and reproducible expansion step before analysis. Furthermore, studies of HIV-specific CD4+ T cells suggest that the presence of an intact central memory T-cell pool, capable of proliferation, correlates better with control of HIV infection than the presence of effector cells only capable of IFNγ production directly ex vivo.16,43 Assays comparable to the one used here, combining in vitro expansion and restimulation, were shown to correlate well with protection against disease in both hepatitis C and malaria infection.17,34,44 Several recent studies in mice clearly demonstrated the importance of CD4+ T cells for the generation of an effective memory CD8+ T-cell response with adequate proliferative and functional properties,20,21,45 especially during the transition from effector to memory CD8+ T cells.46,47 In addition, several disease models in mice indicated the necessity of specific CD4+ T-cell help for maintenance of CD8+ T-cell function during chronic infection.22-24 In the setting of human EBV infection, a clear peak in EBV-specific CD4+ T cells during acute infection (Precopio et al28 and E.P., K.v.D., J. F. L. Weel, F. J. Bemelman, L. E. Gamadia, M.H.J.v.O., and D.v.B., unpublished results, March 2004) shows that EBV-specific CD4+ T cells transiently expand. Also in support for a role of EBV-specific CD4+ T cells in vivo for controlling EBV, it was recently demonstrated that after bone marrow transplantation the use of a CD4+ T-cell–depleted graft led to an increased frequency of patients with detectable EBV replication, although the incidence of posttransplantation lymphoproliferative disease (PTLD) was not increased as long as CD8+ T cells were present in the graft.48 In an earlier study we found a loss of EBV-specific CD8+ T-cell function at very late stages (CD4+ T cells < 200/μL) during HIV infection.14 Here it appears that loss of EBNA1-specific CD4+ T cells (at a median total CD4+ T-cell count of 300/μL and more than 1 year before NHL diagnosis) occurs at an earlier stage, which might be in accordance with a role in maintenance of CD8+ T-cell function. However, as loss of EBNA1-specific CD4+ T cells occurs well before the loss in EBNA1-specific CD8+ T cells, this could mean that CD8+ T cells are less dependent on CD4+ T-cell maintenance than suggested in mouse studies. While CD4+ T cells may not be indispensable for the maintenance of CD8+ T-cell responses, they might play a role in the priming of new EBNA1-specific CD8+ T-cell clones, refreshing the repertoire of CD8+ T cells that may get exhausted due to the high amounts of EBV-infected cells present in HIV-infected subjects.
Next to a role in helping the CD8+ T-cell response, EBV-specific CD4+ T cells might also have an effector function by themselves. Numerous studies investigated the recognition of EBV-infected cells by CD4+ T cells via recognition of latent49-53 or lytic antigens54 and suggested that EBV-specific CD4+ T cells could directly control outgrowth of EBV-infected B cells or tumors. In a mouse model, it was recently demonstrated that EBNA1-specific CD4+ T cells can indeed display a cytotoxic function in vivo, although this HLA class I–negative model is probably not representative for AIDS-related NHL.55
Interestingly, while loss of EBNA1-specific CD4+ T cells appeared to be associated with progression to NHL, BZLF1-specific CD4+ T cells were still detected in a number of NHL patients. This suggests a different role for these cells in the control of EBV-infected B cells. EBNA1 is expressed in a majority of tumors, and, as both EBNA1-specific CD4+ and CD8+ T cells have recently been shown to be capable of recognizing EBV-infected B cells,51,52,56-58 it seems likely that loss of these cells could alter the capacity to control tumor outgrowth. Interestingly, high numbers of EBNA1-specific CD8+ T cells were detected in a number of patients. High EBNA1-specific responses, measured directly ex vivo, have been described earlier and seemed to be associated with HLA B7, B35, or B53.59 Here, high numbers of EBNA1-specific CD8+ T cells were not associated with particular HLA types, in accordance with our earlier findings.33 This difference might be explained by the use of an expansion step, which allows for the detection of otherwise immeasurable responses, due to the important proliferative capacity of CD8+ T cells in vitro. Thus, using this 12-day expansion assay, EBNA1-specific T-cell responses are more readily detected and seem to be more frequent than previously thought.
In contrast to the EBNA1-specific response, presumably responsible for recognizing proliferating B cells, BZLF1-specific T cells most likely will recognize antigens from EBV-infected epithelial cells or B cells entering lytic cycle and could play a more important role in controlling the amount of viral reactivation than the proliferation of latently EBV-infected cells. This is to our knowledge the first time that a difference between lytic and latent EBV antigen–specific T cells is suggested regarding their role in the control of EBV. In healthy carriers, a difference in phenotype of CD8+ T cells was shown.60 This may also have to do with both frequency and/or site of antigen encounter, whereby the (mostly CCR7+) latent antigen–specific CD8+ T cells are more likely to be induced by proliferating EBV-infected B cells, whereas the lytic antigen–specific CD8+ T cells (which are more often CCR7-) might be driven by lytic replication in epithelial cells of the oropharynx or reactivating B cells in (tonsillar or peripheral) lymph nodes. Interestingly, the difference between latent and lytic antigen–specific immune responses was also observed at the antibody level in HIV-infected subjects, who have decreased titers of EBNA1- but increased titers of viral capsid antigen (VCA)–specific immunoglobulin G (IgG).61,62 This may indicate that loss of immunity to EBNA1, but not lytic EBV antigens, is a general feature of HIV infection. The question then remains why EBNA1-specific T cells are lost prior to BZLF1-specific T cells. It is not likely to be a difference in expression of antigens, as for both EBNA1 and BZLF1 a lot of antigen is expected to be present in HIV carriers. Even if different escape mechanisms would affect the EBNA1- and BZLF1-specific response, it could not explain why in healthy carriers EBNA1-specific cells are present. Alternatively, if EBNA1-specific cells are indeed mostly driven by proliferating B cells (either directly and/or via cross-presentation), this might occur mainly in the lymph nodes. As extensive HIV replication occurs mainly in these sites, EBNA1-specific T cells could be much more prone to killing than BZLF1-specific T cells, which are likely to be driven more by EBV replication in epithelial cells or reactivation of EBV in B cells in the oropharynx. Another explanation could be different redistribution of EBNA1- and BZLF1-specific cells, with EBNA1-specific T cells potentially homing to lymph nodes where the precursors of NHL are likely to be located. Finally, it could be that a lower precursor frequency of EBNA1-compared with BZLF1-specific CD4+ T cells could lead to an earlier loss of the former cells. However, early in HIV infection, the frequency of EBNA1-specific CD4+ T cells was higher than that of BZLF1-specific CD4+ T cells, making this an unlikely explanation.
In conclusion, the evolution toward an EBV-related NHL is the result of a multistep process. Thereby a high rate of B-cell stimulation, characteristic for HIV infection, together with a high frequency of EBV-infected B cells, increases the chance of malignant transformation, which can ultimately lead to EBV-positive B-cell tumor outgrowth.5,6,63 This process is normally kept under control by EBV-specific CD8+ T cells. It is very likely that in the absence of specific CD4+ T-cell help, a functional CD8+ T-cell response cannot be maintained.23
Prepublished online as Blood First Edition Paper, July 12, 2005; DOI 10.1182/blood-2005-01-0432.
Supported by the Dutch Cancer Society (grant no. CLBD2000-2164; D.v.B.). E.P., M.H.J.v.O., F.M., and D.v.B. participated in designing the research; E.P., K.v.D., and N.M.N. performed research; E.P. and D.v.B. performed data analysis; and E.P., M.H.J.v.O., F.M., and D.v.B. wrote the manuscript.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 U.S.C. section 1734.
This study was part of the Amsterdam Cohort Studies on AIDS and HIV-1 infection, a collaboration of the Municipal Health Service, the Academic Medical Center and Sanquin Research at CLB.


This feature is available to Subscribers Only
Sign In or Create an Account Close Modal