Abstract
We here investigate the crosstalk of PKC and PKA signaling during primary CD3+ T-lymphocyte activation using pharmacologic inhibitors and activators in combination with our established panel of PKC isotype–deficient mouse T cells in vitro. PKCθ and PKA inversely affect the CD3/CD28-induced IL-2 expression, whereas other PKC isotypes are dispensable in this signaling pathway. Gene ablation of PKCθ selectively results in a profound reduction of IL-2 production; however, complete abrogation of IL-2 production in these PKCθ–/– T cells was achieved only by simultaneous coactivation of the cAMP/PKA pathway in CD3+ T cells. Conversely, the reduced IL-2 production in PKC inhibitor–treated T cells can be rescued by inhibition of the cAMP/PKA pathway in wild-type but not in PKCθ–/– T cells. Mechanistically, the cAMP/PKA and PKCθ pathways converge at the level of NF-AT, as shown by DNA binding analysis. The combined increase in PKA and decrease in PKCθ activity leads to an enhanced inhibition of nuclear NF-AT translocation. This PKCθ/PKA crosstalk significantly affects neither the NF-κB, the AP-1, nor the CREB pathways. Taken together, this opposite effect between the positive PKCθ and the negative cAMP/PKA signaling pathways appears rate limiting for NF-AT transactivation and IL-2 secretion responses of CD3+ T lymphocytes.
Introduction
Following T-cell receptor (TCR) stimulation, lymphocyte activation threshold is coordinated by a complex interplay of distinct signal transduction pathways. The “fine-tuning” of signaling cascades is considered as a crucial step during T-cell activation in order to result in adequate amplitude of an immune response. The molecular processes that regulate the precise level of the immune activation and their complex interpathway integration are, however, still poorly understood. Among several signaling pathways, protein kinase C (PKC) plays an important role in the cellular activation pathway downstream of the antigen receptor. PKCθ, in particular, is known to translocate to the immunologic synapse.1 Once activated, PKCθ plays a critical role in TCR signaling.2 This is confirmed by analysis of CD3+ T cells of mice lacking PKCθ. Ex vivo, PKCθ-deficient T cells are mostly TCR unresponsive and deficient in the production of interleukin 2 (IL-2) due to an impaired transactivation of NF-κB, AP-1, and NF-AT.3-5 In strict contrast, the cyclic adenosine monophosphate (cAMP)–dependent protein kinase A (PKA) pathway represents a negative regulatory mechanism that controls IL-2 expression in T cells. cAMP itself has been demonstrated to activate directly a class of cyclic nucleotide ion channels6,7 as well as the Rap1 guanine exchange factors Epac1 and Epac2.8 The principle cAMP receptor in lymphoid cells, however, is PKA.9
cAMP is produced after TCR stimulation in T lymphocytes, suggesting the cAMP-mediated repression of T-cell activation may represent a physiologic negative feedback control mechanism.10 Suppression of cAMP signaling is thus required for T-cell activation.11 Among other mechanisms, cAMP inhibition is mediated by de novo transcriptional induction of phosphodiesterases (PDEs) upon T-cell activation. In T cells, PDE4 seems to play a particularly important role.12,13 Increased PDE4 expression in T cells is associated with increased IL-2 production via its hydrolysis of cAMP.12 Inversely, PDE4 blockade is shown to augment cAMP levels and thus known to abrogate cytokine secretion and proliferation in T cells through inhibition of NF-κB and NF-AT and activation of CREB.13 Several direct targets of cAMP/PKA signaling have been identified, such as CREB,14 COOH-terminal Src kinase (Csk),15 and NF-AT.16 The detailed interplay and potential crosstalks of PKA with other signaling pathways during physiologic T-cell activation, however, remain mostly unresolved.
Using cell-permanent pharmacologic inhibitors and activators of PKA and PKC, a critical functional crosstalk of PKA- and PKC-derived signals during T-cell activation has been elaborated.17,18 A number of compounds have been reported to inhibit the PKC family, and thus have been used extensively. However, the specificity of these compounds has not been tested rigorously in cell-based assays. Among them, Ro-31-8220 and related bisindolylmaleimides are the most selective PKC inhibitors; however, these compounds inhibit at least 2 other entirely distinct protein kinase families with similar potency.19 Thus, conclusions drawn from their use in intact cells might have been, at least in part, misleading. Additionally, the PKC isotype–specific roles and selective downstream signaling pathways could not be resolved in these pharmacologic panPKC inhibition studies.
In this study, we carefully investigate the crosstalk of PKA- and PKC-derived signals during primary CD3+ T-cell activation using pharmacologic inhibitors and activators of PKA, PDE4, and PKC plus our established panel of PKC knock-out mice.4,20-23,43 Our results reveal a nonredundant physiologic counteraction between the positive PKCθ isotype and the negative cAMP/PKA signaling pathways in regulating the threshold of T-cell activation. Of importance, multiple inhibitory and activatory systems result in consistent data of the critical roles of PKA and PKCθ: PKA activation (via both PKA activator, Sp-8-Br-cAMP, and PDE4 inhibitor RP73401/piclamilast) plus PKCθ inhibition (by PKCθ gene ablation) augment T-cell immunosuppression as measured in TCR/CD28-induced IL-2 secretion responses of T lymphocytes in vitro. Conversely, the reduced activation in panPKC inhibitor–treated T cells can be rescued by pharmacologic inhibition of the cAMP/PKA pathway. Mechanistically, our data resolve that this yin/yang PKA/PKCθ signaling crosstalk selectively regulates NF-AT but not the distinct AP-1, CREB, and NF-κB transactivation pathways.
Materials and methods
Pharmacologic inhibitors
8-pCPT-2′-O-Me-cAMP was purchased from Sigma-Aldrich (St Louis, MO), and H89, Rp-8-Br-cAMP, and Sp-8-Br-cAMP were purchased from Calbiochem (San Diego, CA). PDE4 LMWI RP73401/piclamilast, Ro-31-8220, GF109203X, and panPKC LMWI were provided by ALTANA Pharma (Konstanz, Germany). Antibodies against murine CD69, CD44, and CD25 were obtained from BD PharMingen (San Diego, CA).
Protein kinase scintillation proximity assay
Activity of recombinant baculovirus-expressed recombinant proteins were incubated in kinase assay buffer (40 mM Tris [pH 7.5], 40 mM MgCl2, 0.2 mM HEPES [pH 7.4], 0.2 mM DTT, 0.0002% Triton X-100, 0.3 mg/mL BSA) containing 1 μM ATP, 2 μCi (0.074 MBq) [33P-ATP], 3 μM N-terminal biotinylated peptide (NH2-RKRQRSMRRRVH-COOH), 1 μM PDBu, 160 μM phosphatidylserine. After 40 minutes at room temperature, radioactivity was counted with the Wallac Micro β1450 (PerkinElmer, Shelton, CT).
Analysis of T-cell proliferation
Naive CD3+ T cells were purified from pooled spleen and lymph nodes with mouse T-cell enrichment columns (R&D Systems, Minneapolis, MN). T-cell populations were typically 95% CD3+, as determined by staining and flow cytometry. For anti-CD3 stimulations, T cells (5 × 105) in 200 μL proliferation medium (RPMI supplemented with 10% FCS, 2 mM l-glutamine, and 50 units mL–1 penicillin/streptomycin) were added in duplicates to 96-well plates precoated with anti-CD3 antibody (clone 2C11, 10 μg mL–1). Alternatively, PDBu (10 ng mL–1; Sigma) plus Ca2+ ionophore (ionomycin, 125 ng mL–1; Sigma) was used. Where indicated soluble anti-CD28 (1 μg mL–1; BD Biosciences, San Jose, CA) was added. Cells were harvested at 64 hours after a 16-hour pulse with [3H]thymidine (1 μCi [0.037 MBq]/well) on filters, and the incorporation of [3H]thymidine was measured with a Matrix 96 direct β counter system. Results shown were the mean ± SD of at least 3 independent experiments.
Analysis of IL-2 production
IL-2 produced from the proliferating CD3+ cell cultures was determined by enzyme-linked immunosorbent assay (ELISA, QuantikineM; R&D Systems) from the supernatant. Results shown were the mean ± SD of at least 3 independent experiments.
Western blot analysis
T cells were stimulated with medium alone (control), solid-phase hamster anti-CD3 (clone 2C11, 10 μg mL–1), with or without hamster anti-CD28 (1 μg mL–1, clone 37.51; BD Biosciences) at 37°C for various time periods. Protein lysates were subjected to Western blotting as previously described,4 using antibodies against PKCθ (BD/Signal Transduction), NF-ATc (Affinity BioReagents, Golden, CO), CREB, pCREB (Cell Signalling, Beverly, MA), and DNA Polymerase δ (Santa Cruz Biotechnology, Santa Cruz, CA). All experiments have been performed at least 3 times with similar outcomes.
Gel mobility shift assays
Nuclear extracts were harvested from 2 × 107 cells according to standard protocols as previously described.4 Extract proteins (2 μg) were incubated in binding buffer with [32P]-labeled, double-stranded oligonucleotide probes (NF-κB: 5′-GCC ATG GGG GGA TCC CCG AAG TCC-3′; AP-1: 5′-CGC TTG ATG ACT CAG CCG GAA-3′; NF-AT: 5′-GCC CAA AGA GGA AAA TTT GTT TCA TAC AG-3′) (Nushift; Active Motif, Carlsbad, CA). All experiments have been performed at least 3 times with similar outcomes.
Statistical analysis
Statistical analysis was done with the statistic environment R (www.cran.r-project.org) as described by Everitt and Rabe-Hesketh24 and Dalgaard.25
Results
Activation of resting T lymphocytes (resulting in IL-2 cytokine secretion and subsequent proliferation) is known to require stimulation of the TCR/CD3 complex (plus the CD28 auxiliary receptor) or treatment with phorbol ester (a potent PKC agonist) plus Ca2+ ionophore. In this study, we investigated potential crosstalk between the distinct second messenger systems, DAG and cAMP, with regard to the activation of CD3+ T lymphocytes in vitro.
Pharmacologic targeting of the PKA and the PKC pathways during CD3+ T-cell activation
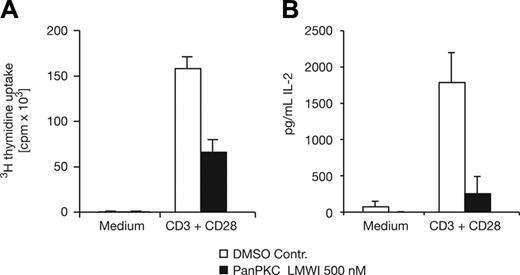
For evaluating the PKC functions, we initially used panPKC low-molecular-weight inhibitors (LMWIs) (Geiselhart et al18 and not shown). The obtained IC50 values on the baculo-expressed isolated enzymes in vitro were listed in Table 1 in direct comparison with the commonly used panPKC LMWI GF109203X and Ro-31-8220. Consistent with published reports, the panPKC LMWI was able to significantly reduce activation-induced proliferation in purified mature mouse CD3+ T cells, isolated from spleen and lymph nodes at a concentration of 500 nM (Figure 1A). The decrease in proliferation, observed in panPKC LMWI–treated T cells stimulated with anti-CD3 plus anti-CD28, was accompanied by a nearly complete reduction in the level of secreted IL-2 (Figure 1B). Thus, and similar to the PKCθ–/– T cells,3-5 pharmacologic inhibition of PKC results in partially defective IL-2 cytokine production and cell cycle progression in vitro (Figure 1 and Geiselhart et al18 ).
IC50 values of panPKC LMWI on isolated PKC isotypes in kinase assays and established controls as Ro-31-8220, GF109203X
Substance . | PKC-θ IC50, μM . | PKC-α IC50, μM . | PKC-β IC50, μM . | PKC-δ IC50, μM . | PKC-η IC50, μM . | PKC-ϵ IC50, μM . | PKC-ι IC50, μM . | PKC-ζ IC50, μM . |
|---|---|---|---|---|---|---|---|---|
| panPKC LMWI | 0.00113 | 0.00337 | 0.00954 | 0.00252 | 0.00995 | 0.00308 | >1 | >1 |
| Ro-31-8220 | 0.0049 | 0.0025 | 0.0069 | 0.0059 | 0.0064 | 0.0047 | >1 | >1 |
| GF109203X | 0.0101 | 0.0033 | 0.0061 | 0.0795 | 0.0352 | 0.0089 | >50 | >100 |
Substance . | PKC-θ IC50, μM . | PKC-α IC50, μM . | PKC-β IC50, μM . | PKC-δ IC50, μM . | PKC-η IC50, μM . | PKC-ϵ IC50, μM . | PKC-ι IC50, μM . | PKC-ζ IC50, μM . |
|---|---|---|---|---|---|---|---|---|
| panPKC LMWI | 0.00113 | 0.00337 | 0.00954 | 0.00252 | 0.00995 | 0.00308 | >1 | >1 |
| Ro-31-8220 | 0.0049 | 0.0025 | 0.0069 | 0.0059 | 0.0064 | 0.0047 | >1 | >1 |
| GF109203X | 0.0101 | 0.0033 | 0.0061 | 0.0795 | 0.0352 | 0.0089 | >50 | >100 |
Impaired T-cell activation in panPKC LMWI–treated cells. (A) Proliferative response and (B) IL-2 production of purified naive CD3+ T cells in the presence of the panPKC LMWI inhibitor, which reduces the proliferation (P = .016) and IL-2 secretion (P = .003) significantly. Cells were left unstimulated or were stimulated with anti-CD3 (precoated at a concentration of 10 μg mL–1) plus soluble anti-CD28 (1 μg mL–1), as indicated, and analysis was done by using standard procedures. Results shown are the mean ± SD of at least 3 independent experiments.
Impaired T-cell activation in panPKC LMWI–treated cells. (A) Proliferative response and (B) IL-2 production of purified naive CD3+ T cells in the presence of the panPKC LMWI inhibitor, which reduces the proliferation (P = .016) and IL-2 secretion (P = .003) significantly. Cells were left unstimulated or were stimulated with anti-CD3 (precoated at a concentration of 10 μg mL–1) plus soluble anti-CD28 (1 μg mL–1), as indicated, and analysis was done by using standard procedures. Results shown are the mean ± SD of at least 3 independent experiments.
In order to investigate the cAMP/PKA and cAMP/Epac pathways, we used the established inhibitor (Rp-8-Br-cAMP26 ) and 2 specific activators (Sp-8-Br-cAMP and PDE4 LMWI/piclamilast, which is significantly more potent than rolipram27 ) of the cAMP/PKA pathway. Sp cAMP, an established cAMP agonist of the cAMP/PKA pathway,8 thereby simply bypasses the generation of endogenous cAMP. As reported previously,17 the Sp cAMP isomer was able to abrogate activation-induced proliferation and IL-2 secretion in response to anti-CD3 and anti-CD28 stimulation of primary CD3+ T cells (Figure 2A-B) at the standard concentration of 250 μM. Treatment with the potent PDE4 LMWI at a concentration of 5 nM, which more physiologically increases endogenous cAMP levels in intact cells, also significantly repressed T-cell proliferation and IL-2 production (Figure 2A-B). In contrast, Rp cAMP, a direct competitor of cAMP that antagonistically interacts with PKA, had no inhibitory effect at the standard concentration of 1000 μM, but rescued the effect of the PDE4 LMWI in proliferation and IL-2 secretion (Figure 2A-B). This was consistent with the function of the Rp cAMP isomer as potent PKA inhibitor. H89, an extensively used enzymatic PKA inhibitor, was not able to rescue PDE4 LMWI effects, indicating lack of this PKA inhibition in intact cells (data not shown, Meja et al28 ). Therefore Rp cAMP but not H89 was used in this study.
T-cell activation in cAMP isomer– and PDE4 LMWI–treated cells. (A) Proliferative response and (B) IL-2 production of purified mature CD3+ T cells in the presence of the inhibitors as specified. The PKA activators (SP-8-Br-cAMP, 250 μM; PDE4 LMWI, 5 nM) reduce the proliferation and the IL-2 production significantly (P < .05). Cells were left unstimulated or were stimulated with anti-CD3 (precoated at a concentration of 10 μg mL–1) plus soluble anti-CD28 (1 μg mL–1), as indicated. Note the significant (P < .001 in the proliferation assay; P = .015 in the IL-2 assay) rescue of the PDE4 LMWI effect by the Rp-8-Br-cAMP (the PKA inhibitor used at 1000 μM). Results shown are the mean ± SD of at least 3 independent experiments.
T-cell activation in cAMP isomer– and PDE4 LMWI–treated cells. (A) Proliferative response and (B) IL-2 production of purified mature CD3+ T cells in the presence of the inhibitors as specified. The PKA activators (SP-8-Br-cAMP, 250 μM; PDE4 LMWI, 5 nM) reduce the proliferation and the IL-2 production significantly (P < .05). Cells were left unstimulated or were stimulated with anti-CD3 (precoated at a concentration of 10 μg mL–1) plus soluble anti-CD28 (1 μg mL–1), as indicated. Note the significant (P < .001 in the proliferation assay; P = .015 in the IL-2 assay) rescue of the PDE4 LMWI effect by the Rp-8-Br-cAMP (the PKA inhibitor used at 1000 μM). Results shown are the mean ± SD of at least 3 independent experiments.
Additive effects of PKC and PKA modulations in primary CD3+ T cells
Both of the PKA-activating compounds (Sp-8 cAMP isomer and PDE4 LMWI) as well as the panPKC LMWI significantly reduced proliferation and IL-2 production in activated CD3+ T cells (Figures 1, 2). Yet, when applied in combination, PDE4 LMWI and panPKC LMWI together acted marginally more effectively in inhibiting activation of primary CD3+ T cells than each compound by itself (Figure 3A-B). This indicated that inhibition of PKC and activation of PKA signaling may additively augment CD3+ T-cell inhibition processes.
Since such a potential PKC/PKA crosstalk has been delineated earlier using pharmacologic inhibition studies, we now aimed to investigate TCR/CD3 signaling functions in our established panel of PKC isotype–deficient T cells in combination with the very selective PDE4 LMWI27 as cAMP/PKA pathway activator. Both PKCθ4 and, as very recently observed by us, PKCα43 are shown to take nonredundant and critical parts in signaling pathways necessary for full antigen receptor–mediated T-cell activation in vitro and T-lymphocyte–dependent immunity in vivo. In contrast, PKCβ, ϵ, δ, and ζ had been recently shown by us to be dispensable in T-cell signaling.20-23
Impaired proliferation and IL-2 secretion in pharmacologic cotreatment conditions. (A) Proliferative response and (B) IL-2 production of purified mature CD3+ T cells in the presence of inhibitors as specified. The panPKC LMWI and the PKA activator PDE4 LMWI reduce the proliferative and the IL-2 response significantly (P < .05). In combination, the additive effect on proliferation of the PDE4 LMWI and the panPKC LMWI (P = .067) is even stronger but not significantly different from the single compounds. Cells were left unstimulated or were stimulated with anti-CD3 (precoated at a concentration of 10 μg mL–1) plus soluble anti-CD28 (1 μg mL–1) or PDBu/ionomycin, as indicated. Results shown are the mean ± SD of at least 3 independent experiments.
Impaired proliferation and IL-2 secretion in pharmacologic cotreatment conditions. (A) Proliferative response and (B) IL-2 production of purified mature CD3+ T cells in the presence of inhibitors as specified. The panPKC LMWI and the PKA activator PDE4 LMWI reduce the proliferative and the IL-2 response significantly (P < .05). In combination, the additive effect on proliferation of the PDE4 LMWI and the panPKC LMWI (P = .067) is even stronger but not significantly different from the single compounds. Cells were left unstimulated or were stimulated with anti-CD3 (precoated at a concentration of 10 μg mL–1) plus soluble anti-CD28 (1 μg mL–1) or PDBu/ionomycin, as indicated. Results shown are the mean ± SD of at least 3 independent experiments.
PKCθ–/– T cells already intrinsically demonstrated reduced IL-2 secretion.4 Therefore, and for direct comparison of CD3/CD28-induced IL-2 production, the DMSO controls of wild-type (wt) and PKCθ-deficient T cells were normalized to each other and set as 100%. The titration curve of PDE4 LMWI demonstrates a strong additive effect of PDE4 LMWI in PKCθ-deficient T cells (Figure 4A). This was especially obvious at suboptimal concentration of PDE4 LMWI. Consistently, when using even such a suboptimal concentration as 0.4 nM PDE4 LMWI, this selectively augmented the defects in IL-2 production of PKCθ-deficient T cells (Figure 4D-E). Activation-induced IL-2 secretion was completely abrogated in the PKCθ-deficient CD3+ T cells, once tested in combination with the PDE4 LMWI at 0.4 nM, while no significant effect could be observed in the wild-type T-cell controls. Of note, CD28 costimulation not only enhanced the level of anti-CD3 mAb-induced IL-2 secretion but also mostly overcame the immunosuppressive effects of the cAMP-elevating agents in wild-type T cells. The order of potency of the stimulatory signals in reversing the inhibitory effects of cAMP-elevating agents on induced IL-2 secretion was (1) anti-CD3/anti-CD28 (approximately 5% inhibition) and (2) anti-CD3 (approximately 85% inhibition) (Figure 4D and not shown). Thus, this difference in the ability of the wild-type versus PKCθ–/– T cells to be inhibited by PDE4 LMWI was observed only in physiologically more relevant anti-CD3/anti-CD28 double-stimulation conditions. Activation-induced proliferation rates in both genotypes, however, were less significantly affected by the simultaneous combination with the PDE4 LMWI (Figure 4B-C). Taken together, the complete abrogation of CD3/CD28-induced IL-2 secretion in PKCθ-deficient CD3+ T cells was achieved by a simultaneous coactivation of the cAMP/PKA pathway.
T-cell activation in PDE4 LMWI–treated wild-type and PKCθ–/– T cells. (A) Titration curve of the PDE4 LMWI with normalized percent of CD3/CD28-induced IL-2 production of CD3+ wild-type and PKCθ-deficient T cells (DMSO control was set as 100% in each genotype). (B-C) Proliferative response and (D-E) IL-2 production of purified mature CD3+ T cells in the presence or absence of PDE4 LMWI inhibitor as specified. Cells were left unstimulated or were stimulated with anti-CD3 (precoated at a concentration of 10 μg mL–1) plus soluble anti-CD28 (1 μg mL–1) or PDBu/ionomycin, as indicated, and analysis was done by using standard procedures. Results shown are the mean ± SD of at least 3 independent experiments. (C, inset) Western blot of CD3+ T-cell lysates immunostained for the endogenous PKCθ isotype and fyn, as indicated. Note the complete breakdown of IL-2 production in the PKCθ–/– T cells when stimulated with anti-CD3 plus anti-CD28. The suboptimal low concentration of 0.4 nM PDE4 LMWI reduces neither the proliferation nor the IL-2 production in the wild-type significantly, but does so in the PKCθ–/– T cells (P = .008 in the proliferation assay; P = .002 in the IL-2 assay; t test).
T-cell activation in PDE4 LMWI–treated wild-type and PKCθ–/– T cells. (A) Titration curve of the PDE4 LMWI with normalized percent of CD3/CD28-induced IL-2 production of CD3+ wild-type and PKCθ-deficient T cells (DMSO control was set as 100% in each genotype). (B-C) Proliferative response and (D-E) IL-2 production of purified mature CD3+ T cells in the presence or absence of PDE4 LMWI inhibitor as specified. Cells were left unstimulated or were stimulated with anti-CD3 (precoated at a concentration of 10 μg mL–1) plus soluble anti-CD28 (1 μg mL–1) or PDBu/ionomycin, as indicated, and analysis was done by using standard procedures. Results shown are the mean ± SD of at least 3 independent experiments. (C, inset) Western blot of CD3+ T-cell lysates immunostained for the endogenous PKCθ isotype and fyn, as indicated. Note the complete breakdown of IL-2 production in the PKCθ–/– T cells when stimulated with anti-CD3 plus anti-CD28. The suboptimal low concentration of 0.4 nM PDE4 LMWI reduces neither the proliferation nor the IL-2 production in the wild-type significantly, but does so in the PKCθ–/– T cells (P = .008 in the proliferation assay; P = .002 in the IL-2 assay; t test).
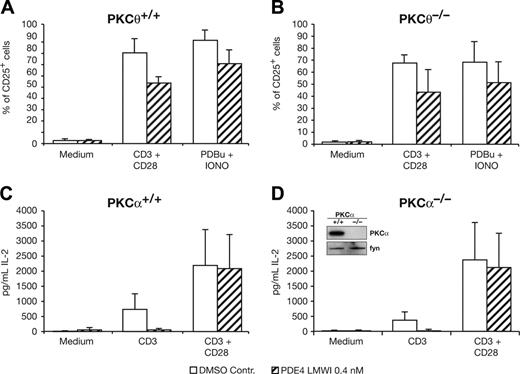
TCR-induced S-phase entry of resting T cells is known to promote transcriptional up-regulation of both IL-2 and IL-2 receptor α-chain (CD25) genes, thereby constituting the autocrine cycle of IL-2 cytokine and its high-affinity receptor. However, albeit treatment with PDE4 LMWI slightly reduces CD25 and CD69 expression in activated CD3+ T cells, no additive effect of PDE4 LMWI and PKCθ gene ablation was observed. PDE4 LMWI treatment of PKCθ-deficient T cells induced comparable CD25 and CD69 surface expression when compared with wild-type T cells (Figure 5A-B and data not shown). Consistently, CD3/CD28 ligation–induced expression of CD25 (as well as the activation marker CD69, not shown) was reported to be normal in PKCθ–/– T cells.4 This indicated that the PKA/PKCθ crosstalk acts in a unique pathway specific for TCR-mediated IL-2 expression that is distinct from pathways used for CD25 und CD69 up-regulation.
PKA activation in PKCθ-deficient T cells resulted in pronounced decrease of IL-2 secretion (Figure 4D-E). Of importance, however, no such combinatorial effect can be observed when using the PKCα-deficient T cells.43 In response to either of the stimuli, neither proliferation nor IL-2 secretion of CD3+ T cells from the PKCα–/– mice was further reduced in the presence of PDE4 LMWI relative to that of wild-type T cells (Figure 5C-D). The normalized effects of PDE4 LMWI in percent induction of CD3/CD28-induced proliferation, and IL-2 production of CD3+ wild-type and PKCθ- or PKCα-deficient T cells (DMSO control was set as 100% in each genotype for direct comparison purposes), are shown (Table 2). Similarly to PKCα–/– T cells, no significant additive PDE4 LMWI defect in either proliferation or IL-2 secretion was obtained with our PKCβ–/– T cells (Thuille et al22 and not shown). Consistently, when testing PKCϵ, δ, and ζ KO lines (data not shown), none of these other PKC isotypes was nonredundantly involved in the counterregulation of cAMP/PKA-mediated suppression of IL-2 responses. These genetic data clearly excluded any functional crosstalk of PKC isotypes, except PKCθ, with PKA in these pathways (Figures 4, 5 and not shown).
Effects of PDE4 LMWI on relative percent of CD3/CD28-induced proliferation and IL-2 production of CD3+ wild-type and PKCθ- or PKCα-deficient T cells
. | Proliferation . | . | IL-2 secretion . | . | ||
|---|---|---|---|---|---|---|
. | DMSO control . | 5 nM PDE4 LMWI . | DMSO control . | 5 nM PDE4 LMWI . | ||
| wt+/+ | 100 | 35 ± 17 | 100 | 97 ± 73 | ||
| PKCα-/- | 100 | 38 ± 10 | 100 | 89 ± 48 | ||
| PKCθ-/- | 100 | 36 ± 15 | 100 | 33 ± 38 | ||
. | Proliferation . | . | IL-2 secretion . | . | ||
|---|---|---|---|---|---|---|
. | DMSO control . | 5 nM PDE4 LMWI . | DMSO control . | 5 nM PDE4 LMWI . | ||
| wt+/+ | 100 | 35 ± 17 | 100 | 97 ± 73 | ||
| PKCα-/- | 100 | 38 ± 10 | 100 | 89 ± 48 | ||
| PKCθ-/- | 100 | 36 ± 15 | 100 | 33 ± 38 | ||
Effects of PDE4 LMWI (at 5 nM) on relative percent of CD3/CD28-induced proliferation and IL-2 production of CD3+ wild-type and PKCθ- or PKCα-deficient T cells (DMSO control was set as 100% in each genotype for direct comparison purposes). Basically similar results have been obtained with PDE4 LMWI at 0.4 nM (not shown). Statistical analysis of 3 experiments is shown.
CD25 surface expression in PKCθ–/– and T-cell activation in PKCα–/– T cells is not affected by PDE4 LMWI. (A-B) Flow cytometric analysis of expression of CD25 wild-type PKCθ+/+ and PKCθ–/– T cells. Single-cell suspensions of purified mature CD3+ T cells, stimulated or not for 16 hours with anti-CD3 and anti-CD28, were stained with anti-CD25. Percentages of positive cells are indicated. Experiments were repeated at least 3 times with similar results. (C-D) IL-2 production of purified mature CD3+ T cells in the presence of inhibitors as specified. Cells were left unstimulated or were stimulated with anti-CD3 (precoated at a concentration of 10 μg mL–1) plus soluble anti-CD28 (1 μg mL–1) or PDBu/ionomycin, as indicated. Results shown are the mean ± SD of at least 3 independent experiments. (D, inset) Western blot of CD3+ T-cell lysates immunostained for the endogenous PKCα isotype and fyn, as indicated.
CD25 surface expression in PKCθ–/– and T-cell activation in PKCα–/– T cells is not affected by PDE4 LMWI. (A-B) Flow cytometric analysis of expression of CD25 wild-type PKCθ+/+ and PKCθ–/– T cells. Single-cell suspensions of purified mature CD3+ T cells, stimulated or not for 16 hours with anti-CD3 and anti-CD28, were stained with anti-CD25. Percentages of positive cells are indicated. Experiments were repeated at least 3 times with similar results. (C-D) IL-2 production of purified mature CD3+ T cells in the presence of inhibitors as specified. Cells were left unstimulated or were stimulated with anti-CD3 (precoated at a concentration of 10 μg mL–1) plus soluble anti-CD28 (1 μg mL–1) or PDBu/ionomycin, as indicated. Results shown are the mean ± SD of at least 3 independent experiments. (D, inset) Western blot of CD3+ T-cell lysates immunostained for the endogenous PKCα isotype and fyn, as indicated.
Counteraction between the positive PKCθ and the negative cAMP/PKA pathways in primary CD3+ T cells
cAMP/PKA and PKC pathways have been discussed as direct antagonists maintaining a balance for signaling responses downstream of the TCR. Consistently, the effect of the panPKC LMWI was significantly rescued by a PKA inhibitor (Rp cAMP; Figure 6A,C), indicating that once the negative signals from PKA were missing, the activated T cells can mostly overcome pharmacologic PKC inhibition. However, Rp cAMP treatment by itself had no additional effect (Figure 2 and not shown). Yet in PKCθ–/– T cells, where no PKCθ protein is expressed, the PKA inhibitor Rp cAMP failed to rescue activation-induced IL-2 secretion (Figure 6B,D). The PKA inhibitor Rp cAMP is able to rescue the effect only in panPKC LMWI–treated wild-type, but not in the PKCθ-deficient, CD3+ T cells. This finding again clearly indicates that among the PKC family members in T cells, the PKCθ isotype plays the critical and nonredundant role in counteracting the cAMP/PKA-negative signaling during T-cell activation.
PKCθ/PKA crosstalk converges at the level of TCR-induced NF-AT activation
To further elucidate the molecular basis of the functional PKCθ/PKA interaction, we analyzed the NF-κB, AP-1, CREB, and NF-AT pathways, known to be critical in TCR/CD28-induced IL-2 cytokine expression.29 As reported, electrophoretic mobility shift assays (EMSAs) demonstrated a significant decrease in NF-κB, AP-1, and NF-AT activation in PKCθ–/– T cells.3-5 Consistently, CD3/CD28 cross-linking failed to fully activate the NF-κB, AP-1 (Figure 7A-B), and NF-AT (Figure 8A) pathways in PKCθ-deficient CD3+ cells. Yet, when using 5-fold more of nuclear extracts from the PKCθ-deficient CD3+ cells, relative to the wild-type extracts, the residual CD3/CD28-induced DNA binding was clearly detectable (Figure 7C for AP-1 and Figure 8B for NF-AT).
Proliferation and IL-2 secretion in cotreatment conditions in wild-type and PKCθ–/– T cells. (A-B) Proliferative response and (C-D) IL-2 production of purified mature CD3+ T cells in the presence of inhibitors as specified. The panPKC LMWI reduces the proliferation of wild-type but not PKCθ–/– T cells significantly (P < .05), whereas the IL-2 production is significantly reduced in both genotypes. Cells were left unstimulated or were stimulated with anti-CD3 (precoated at a concentration of 10 μg mL–1) plus soluble anti-CD28 (1 μg mL–1) as indicated. Arrows mark the rescue result occurring in wild-type PKCθ+/+ (significantly in the IL-2 assay; P = .037) but not PKCθ–/– T cells. Results shown are the mean ± SD of at least 3 independent experiments.
Proliferation and IL-2 secretion in cotreatment conditions in wild-type and PKCθ–/– T cells. (A-B) Proliferative response and (C-D) IL-2 production of purified mature CD3+ T cells in the presence of inhibitors as specified. The panPKC LMWI reduces the proliferation of wild-type but not PKCθ–/– T cells significantly (P < .05), whereas the IL-2 production is significantly reduced in both genotypes. Cells were left unstimulated or were stimulated with anti-CD3 (precoated at a concentration of 10 μg mL–1) plus soluble anti-CD28 (1 μg mL–1) as indicated. Arrows mark the rescue result occurring in wild-type PKCθ+/+ (significantly in the IL-2 assay; P = .037) but not PKCθ–/– T cells. Results shown are the mean ± SD of at least 3 independent experiments.
EMSA analysis of NF-κB and AP-1 in wild-type and PKCθ–/– T cells. (A) Nuclear extracts were prepared from purified mature CD3+ wild-type and PKCθ–/– T cells, stimulated for 16 hours with medium alone or plate-bound anti-CD3 plus soluble anti-CD28, as indicated. Gel mobility shift assays were performed using radiolabeled probes containing either (A) NF-κB or (B-C) AP-1 binding site sequences. (C) To study potential additive effects in PKCθ-deficient T cells, 5-fold more PKCθ–/– nuclear extracts had been used. The specificity of p50 NF-κB as well as fos was confirmed by supershifting the electrophoretic mobility shift with antibodies, as indicated by the arrow. Experiments were repeated at least 3 times with similar results.
EMSA analysis of NF-κB and AP-1 in wild-type and PKCθ–/– T cells. (A) Nuclear extracts were prepared from purified mature CD3+ wild-type and PKCθ–/– T cells, stimulated for 16 hours with medium alone or plate-bound anti-CD3 plus soluble anti-CD28, as indicated. Gel mobility shift assays were performed using radiolabeled probes containing either (A) NF-κB or (B-C) AP-1 binding site sequences. (C) To study potential additive effects in PKCθ-deficient T cells, 5-fold more PKCθ–/– nuclear extracts had been used. The specificity of p50 NF-κB as well as fos was confirmed by supershifting the electrophoretic mobility shift with antibodies, as indicated by the arrow. Experiments were repeated at least 3 times with similar results.
As a result, activation of the cAMP/PKA pathway (via PDE4 LMWI) did not augment defects of NF-κB (Figure 7A) nor did it significantly enhance AP-1 transactivation defects in PKCθ-deficient CD3+ T cells (Figure 7C). Consistently, Western blot analysis revealed no profound differences in activated phospho-ERK1/2 in wild-type and PKCθ-deficient CD3+ T cells during PDE4 LMWI cotreatment (not shown). Yet, upon PDE4 LMWI treatment, an enhanced defect of NF-AT binding in PKCθ–/– T cells had been reproducibly observed (Figure 8B): PDE4 LMWI treatment reduced NF-AT transactivation below the detection limit only in PKCθ-deficient CD3+ T cells. Consistently, upon PDE4 LMWI treatment, nuclear translocation of NF-AT was further impaired in PKCθ–/– T cells (Figure 8C). The activation-dependent induction of the 3 prominent isoforms of NF-ATc in whole-cell extracts was not altered in wild-type and PKCθ–/– T cells, treated with either PDE4 LMWI or DMSO buffer control (not shown), excluding signaling defects caused simply by different NF-AT expression levels. Taken together, this additive transactivation defect on NF-AT signaling was consistent with the reported role of PKA to modulate nuclear entry of NF-AT16 and with the observed additive effects of PKA activation in PKCθ–/– T cells (Figures 5, 6).
The PDE4 LMWI activates the cAMP/PKA plus the cAMP/Epac/Rap1 pathway. In order to address which of the 2 distinct pathways is affected, we used the cAMP isomer agonists, Sp-8-Br-cAMP and 8-pCPT-2′-O-Me-cAMP, which selectively activate the cAMP/PKA or the cAMP/Epac/Rap1 pathways,30 respectively. As a result, the NF-AT transactivation of activated wild-type and PKCθ-deficient T cells appears to be independent of the cAMP/Epac/Rap1 pathway under the experimental conditions used: When analyzing Epac cAMP isomer (8-pCPT-2′-O-Me-cAMP)–treated cells for TCR-induced NF-AT activation, no inhibiting effect could be seen with this cAMP isomer (Figure 8D and not shown), while NF-AT DNA binding was strongly reduced by the Sp cAMP isomer in parallel samples. As further control, we defined the phosphostatus of CREB as the marker of PKA activation using immunoblotting: Phosphorylation of CREB was found to be inducible upon CD3/CD28 stimulation (Figure 8E) as well as by the treatment with Sp cAMP (but not Epac cAMP) in CD3+ T cells (not shown), consistent with a selective activation of the cAMP/PKA pathway. Of importance for our hypothesis, phosphorylation of CREB was found to be similarly induced in wild-type and PKCθ-deficient T cells upon CD3/CD28 ligation (Figure 8E). Sp cAMP (but not Epac cAMP) slightly enhanced the stimulus-induced phosphorylation of CREB, confirming the selective activity of these distinct cAMP isomers, Sp cAMP and Epac cAMP. Taken together, these experiments validate the cAMP/PKA crosstalk, as the negative cAMP signaling pathways physiologically counteract the antigen receptor–induced NF-AT but not the NF-κB, AP-1, or CREB pathways.
EMSA and nuclear translocation analysis of NF-AT in wild-type and PKCθ–/– T cells. Nuclear extracts were prepared from purified mature CD3+ wild-type and PKCθ–/– T cells, stimulated for 16 hours with medium alone or plate-bound anti-CD3 plus soluble anti-CD28 in combination with the PDE4 LMWI, the Sp-8-Br-cAMP, and the Epac-specific activator (8-pCPT-2′-O-Me-cAMP), as indicated. In EMSA (A,B,D), the specificity of NF-ATc was confirmed by supershifting the electrophoretic mobility shift with antibodies, as indicated by the arrow. To study potential additive effects using EMSA methodology in PKCθ-deficient T cells, 5-fold more PKCθ–/– nuclear extracts had been used (B), as PKCθ gene ablation already strongly reduced NFAT levels (A). Activation-induced translocation of NF-AT or phosphorylation of CREB was determined by immunoblotting of nuclear extracts (C,E) for NF-ATc, (p)CREB and panCREB, respectively, as indicated. Experiments were repeated at least 3 times with similar results.
EMSA and nuclear translocation analysis of NF-AT in wild-type and PKCθ–/– T cells. Nuclear extracts were prepared from purified mature CD3+ wild-type and PKCθ–/– T cells, stimulated for 16 hours with medium alone or plate-bound anti-CD3 plus soluble anti-CD28 in combination with the PDE4 LMWI, the Sp-8-Br-cAMP, and the Epac-specific activator (8-pCPT-2′-O-Me-cAMP), as indicated. In EMSA (A,B,D), the specificity of NF-ATc was confirmed by supershifting the electrophoretic mobility shift with antibodies, as indicated by the arrow. To study potential additive effects using EMSA methodology in PKCθ-deficient T cells, 5-fold more PKCθ–/– nuclear extracts had been used (B), as PKCθ gene ablation already strongly reduced NFAT levels (A). Activation-induced translocation of NF-AT or phosphorylation of CREB was determined by immunoblotting of nuclear extracts (C,E) for NF-ATc, (p)CREB and panCREB, respectively, as indicated. Experiments were repeated at least 3 times with similar results.
Discussion
On the basis of pleiotropic pharmacologic inhibition studies, several examples of crosstalk between the cAMP/PKA and PKC pathways are described.31-33 It appears strictly cell-type dependent, whether the crosstalk between PKA and PKC thereby counteract or potentiate each other: In platelets and neutrophils, the PKC pathway activates cellular functions, such as proliferation, but the cAMP signaling system antagonizes this activation. Conversely, in lymphoma cells, PKC activation potentiates cAMP production and stimulation of PKC, and the cAMP/PKA pathway strongly activates binding of CREB to its DNA binding site, CRE. This enhancer element then positively modulates the expression of CREB-mediated activation genes. In primary T lymphocytes, however, cAMP is produced after stimulation, suggesting the cAMP-mediated repression of T-cell activation following TCR/CD3 ligation represents a negative feedback control mechanism.10 Consequently, suppression of cAMP signaling is strictly required for a biologic T-cell response.11 cAMP levels in the T cell are the results of adenylate cyclases, which synthesize cAMP and phosphodiesterases (PDEs) that degrade cAMP. The PDE4 isotype thereby mainly controls cAMP levels during T-cell activation.13
The most intriguing result of our study is that during TCR activation of primary CD3+ T cells, the positive and the negative signaling cascades of PKCθ and PKA act in an yin/yang mode on the regulation of IL-2 expression. Consistently, combined increase in PKA and decrease in PKCθ activity (via gene ablation of PKCθ, Figure 4) completely abrogated the IL-2 production in primary CD3+ T cells. Thus, activating the cAMP/PKA pathway has an enhanced inhibitory effect on T cells, once the signaling cascade from the TCR is specifically disturbed by PKCθ loss-of-function. Conversely, panPKC LMWI–inhibited T cells, PKA inhibition via Rp cAMP mostly rescues IL-2 expression (Figure 6C), since the residual PKCθ activity (inaccessible for the PKC inhibitor) then allows a sufficient signaling threshold to occur in the absence of the PKA antagonism. However and of importance, once no PKCθ at all is present in the activated cell (as in the T cells derived from the PKCθ-KO mouse line4 ), no positive PKC signaling is available. As a consequence, inhibition of the negative PKA signal then has no rescue effect (Figure 6D). This is interpreted as strong evidence that PKCθ (but no other PKC isotype) nonredundantly attenuates PKA-mediated negative signaling in T cells. Consistently, when testing other PKC KO lines (Figure 5C-D, Table 2, and data not shown), we were able to conclude that no other PKC isotype is nonredundantly involved in the counterregulation of cAMP/PKA-mediated suppression of IL-2 responses.
NF-AT is an established site of integration of multiple signaling pathways. Thus, NF-AT ensures correct responses to complex biologic stimuli. The cAMP/PKA type I pathway thereby is known to induce Csk activation,34 the major negative regulator of the Src-PTK Lck.15 Additionally, PKA has been reported to directly phosphorylate NF-AT and thus inhibits nuclear entry of NF-AT via association with 14-3-3 proteins.16 Consistently, overexpression of NF-AT antagonizes the inhibitory effect of PKA on IL-2 gene expression. NF-AT is negatively regulated by several NF-AT kinases such as glycogen synthase kinase 3 (GSK3). These are constitutive NF-AT protein kinases that promote NF-AT nuclear export35,36 ; however, phosphorylation by GSK3 requires prior phosphorylation by a priming kinase such as PKA. Consistently, NF-AT mutants of the PKA phosphorylation sites lost 14-3-3 binding, translocated to the nucleus, and became transcriptionally active.37 In contrast, upon TCR stimulation, NF-AT is dephosphorylated by calcineurin, which is established to functionally cooperate with PKCθ38,39 in this pathway. This Ca2+/calcinerurin/PKCθ pathway leads to activation and nuclear entry of NF-AT and subsequent IL-2 production of the activated T cells. Thus, cAMP/PKA-mediated Csk activation (and subsequent abrogation of the PLCγ1-derived calcium fluxes, an upstream requirement of the Ca2+/calcineurin/NF-AT activation) as well as the direct NF-AT protein phosphorylation by PKA (as priming kinase for GSK3) provides molecular mechanisms for the counteraction of the Ca2+/calcinerurin/PKCθ/NF-AT signaling pathways.
Consistent with the negative role for cAMP/PKA in TCR signaling (reviewed in Torgersen et al9 ), PKCθ inhibition acts additively in the modulation of NF-AT (Figure 8). Combined increase in PKA (via PDE4 LMWI) and decrease in PKCθ (via gene ablation of PKCθ) activity abrogated NF-AT nuclear translocation (Figure 8C) and DNA-binding (Figure 8B) in primary CD3+ T cells. As inhibitory effects of pharmacologic elevations in cAMP in T cells may not strictly require PKA activity,40 we tested the possibility that the cAMP-Epac-Rap1 pathway is responsible for a reduced NF-AT binding and subsequent reduced IL-2 production in wild-type CD3+ T cells (Figure 8D). However, we could not observe a decreased NF-AT binding using this specific Epac cAMP isomer, 8-pCPT-2′-O-Me-cAMP.30 NF-AT binding was reduced only when using the PDE4 LMWI or the specific PKA cAMP isomer, Sp-8-Br-cAMP. Conversely, the PKA/PKCθ signaling crosstalk had no significant effect on NF-κB (Figure 7A) and CREB transactivation pathways (Figure 8E). Opposite effects on T-cell signaling thresholds have also been correlated with opposite effects of PKAand PKC on the Raf/MEK/ERK pathway.30 However, when analyzing primary mouse CD3+ cells, no profound differences in activated phospho-ERK1/2 and AP-1 DNA binding activity (data not shown and Figure 7C) in wild-type and PKCθ-deficient CD3+ T cells during PDE4 LMWI cotreatment were revealed.
PKCθ and PKA, unlike the more proximally acting Lck and ZAP70 protein tyrosine kinases, may not serve as triggers of the immune response but instead may further refine lymphocyte signaling by acting as critical signal threshold regulators of NF-AT activation (ie as rate-limiting steps in triggering a full T-cell IL-2 production during antigenic stimulation). Full and sustained NF-AT activation must be maintained to induce an irreversible commitment to T-cell activation, particularly at lower antigenic peptide concentrations. Along this line of argumentation, PKCθ-deficient T cells generate still detectable, albeit significantly reduced, nuclear localization of NF-ATc family members (Figure 8C). Given the importance of the sustained NF-AT translocation, this partial reduction appears to correlate with an inability of the stimulus to induce full IL-2 gene expression and T-cell proliferation in these T cells.4 Consistently, agents that raise PKA activity in T cells, such as PDE4 LMWI and Sp cAMP, counteract PKCθ activation signaling by this mechanism (Figures 2,6). Given that upstream regulatory regions of many genes contain NF-AT binding sites,41 the described PKCθ and PKA interpathway integration may modulate a number of genes during an effective immune response. Indeed, other cytokines, in particular IL-4 and IL-10, were found to be inhibited by PKA activation in these T cells (data not shown). This is consistent with recent reports that PKCθ is required for the development of a robust immune response controlled by TH2 cells.42 Although the antagonistic roles of PKA- and PKCθ-dependent signaling cascades are defined here, the exact biochemical mechanism of how positive PKCθ and the negative PKA signaling pathways regulate the fine-tuning of the critical NF-AT responses is still speculative.
In primary mouse CD3+ T cells, a bidirectional PKA/PKC control model exists. The isotype-selective combination of PKCθ inhibition and PKA activation completely abrogates the level of TCR/CD28-induced IL-2 expression. Mechanistically, activation of the cAMP/PKA pathway in combination with PKCθ gene ablation resulted in a selective block of NF-AT transactivation. Thus, PKCθ is the essential part of a physiologic signaling cascade that is necessary to counteract the inhibitory cAMP/PKA pathway during sustained clonotypic T-cell expansion. This antagonistic crosstalk between the PKCθ-derived positive signals and the PKA-derived negative signals may represent one mechanism of how the antigen receptor–dependent fine-tuning of the amplitude of T-lymphocyte activation works. Consequently, a combined increase in PKA and decrease in PKCθ activity might serve as an innovative combinatorial drug treatment concept in order to manifest improved efficacy and selectivity in therapeutic options for different immune disorders.
Prepublished online as Blood First Edition Paper, March 2, 2006; DOI 10.1182/blood-2005-10-4044.
Supported by grants from the Austrian Science Foundation (FWF; P16229 and SFB021) and by a cooperation agreement with ALTANA Pharma (Konstanz, Germany).
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 U.S.C. section 1734.
We are grateful to H. Dietrich, N. Krumböck, and G. Böck (all from Innsbruck) for animal housekeeping, expert technical assistance, and FACS analysis, respectively. All experiments comply with the current laws of Austria.







This feature is available to Subscribers Only
Sign In or Create an Account Close Modal