Abstract
Adaptor protein-3 (AP-3) is an ubiquitous cytoplasmic complex that shuttles cargo proteins from the trans-Golgi and a tubular-endosomal compartment to endosome-lysosome–related organelles. Lack of the β3A subunit of this complex causes Hermansky-Pudlak syndrome type 2, an autosomal recessive disease characterized by partial albinism, prolonged bleeding tendency, and immunodeficiency. To investigate the pathogenesis of immunodeficiency, we studied natural killer (NK) cells and neutrophil functions in 2 previously unreported siblings affected by Hermansky-Pudlak type 2 syndrome. In both patients we observed a dramatic reduction of cytolytic activity of freshly isolated and of IL-2–activated NK cells. Levels of perforin were reduced in unstimulated NK cells, thereby accounting for the impairment of NK cytolitic activity. In addition, analysis of neutrophils in these patients demonstrated that intracellular elastase content was largely reduced while CD63 expression on plasma membrane was substantially increased. Taken together, these observations suggest that type 2 Hermansky-Pudlak syndrome is characterized by defects of innate immunity.
Introduction
Adaptor protein (AP) complexes play a fundamental role in vesicle formation and cargo selection in the vescicular trafficking system of the cell. AP-3 is a protein complex composed of 4 different subunits that are identified as β3A, μ3A, δ, and σ3.1-4 This heterotetrameric complex is ubiquitously expressed and mediates transmembrane proteins sorting from the endosomal and trans-Golgi network to lysosomes and endosome-lysosome–related organelles.5 As a coat protein, the AP-3 complex concentrates at the cytoplasmic surface of the donor membrane, selecting cargo proteins to be included in the forming vesicles through binding of a specific domain in the cytoplasmic tail of integral membrane cargo proteins.6-8 Upon direct or indirect interaction with AP-3, lysosomal and lysosome-related organelle transmembrane proteins, including CD63, Lamp-1, Lamp-2, tyrosinase, and CD1b, are sorted to lysosomes and to endosome-lysosome–related organelles, such as melanosome, platelet-dense bodies, antigen-processing compartments, and lytic granules. Altered trafficking of these proteins in AP-3–deficient cells results in redistribution of these proteins to the plasma membrane.9-12
Hermansky-Pudlak syndrome type 2 (HPS2) is an autosomal recessive inherited disease that is caused by disruption of the AP-3 complex. All 4 patients described to date present a mutations in ADTB3A, the gene encoding for the β subunit of the AP-3 complex.1,9,13-15 The absence of the β3A subunit results in the loss of stability of the heterotetrameric complex and leads to degradation of μ3A, to which β3A is directly bound, while the other subunits are variably affected.1,15 The disease is characterized by oculocutaneous albinism, platelet defects due to absence of platelet bodies (leading to a defect in the secondary aggregation response), and immunodeficiency.14,16
Although the AP-3 complex is ubiquitously expressed, its absence differentially affects vesicular trafficking in certain cells types, including melanocytes, platelets, cytotoxic T lymphocytes (CTL), and natural killer (NK) cells. In these cells, biogenesis of lysosome-related organelles and/or sorting of lysosome-specific proteins is altered, thereby leading to selective dysfunction. In melanocytes, the AP-3 complex disruption leads to a missorting of tyrosinase, thereby accounting for albinism of skin, retina, and iris of HPS2-affected patients.16-19 In platelets, dense granule formation is impaired, leading to storage pool deficiency and consequently to extended bleeding time.9,15
Disruption of the AP-3 complex in CTLs leads to mislocalization of the lysosomal protein CD63 to the plasma membrane and to loss of cytotoxic activity. CTLs are unable to kill target cells because of impaired microtubule-mediated mobilization of lytic granules to the immunologic synapse.1 Azurophil granules are another example of lysosome-related organelles; these organelles are present in myeloid progenitors and in mature neutrophils. Benson et al have shown that deficiency of AP-3 in canine cyclic hematopoiesis prevents normal trafficking of neutrophil elastase (NE) to granules, misdirecting it to the membrane. Because the processed form of NE interacts in vitro with the μ3A subunit through a tyrosine-based sorting signal in its cytoplasmic tail, it was hypothesized that AP-3 directs NE docking to azurophil granules in a nonredundant fashion.20
Neutropenia and impairment of cytotoxic activity have been reported in HPS2 patients1,13,15 and in other inherited conditions characterized by partial albinism and immunodeficiency such as Chediak-Higashi and Griscelli syndromes,21-27 but the mechanism involved in their pathogenesis in Hermansky-Pudlak type 2 has not been elucidated.
In this study we have analyzed the link between the defect of AP-3 and the immunologic defects of neutrophils and NK cells in HPS2 patients. We report defective cytolytic activity of NK cells and neutropenia in 2 siblings with HPS2 due to 2 novel mutations in the coding sequence of ADTB3A. Analysis of perforin and elastase staining in NK cells and neutrophils, respectively, demonstrates a reduction in the content of these proteins, suggesting that abnormal transport of these proteins may account for the functional defects of NK cells and for the reduced number of mature neutrophils that are observed in these patients.
Patients, materials, and methods
Patients
We have studied a family with 2 affected individuals, a 7-year-old girl (Pt 1) and her 4-year-old brother (Pt 2) born from nonconsanguineous parents, who presented genetic, clinical, and immunologic features of HPS2. Both affected children presented light skin color and blonde hair, nystagmus, and retinal hypopigmentation as assessed by ophthalmoscopy. Neutropenia was discovered at 4 months of age (0.445 × 109 cells per liter) in Pt 1 and at 3 months (0.178 × 109 cells per liter) in Pt 2. Assessment of polymorphonuclear cell (PMN) counts before G-CSF treatment showed variations ranging from 0.176 × 109/L to 0.785 × 109/L in Pt 1 and from 0.068 × 109/L to 0.422 × 109/L in Pt 2 (Table 1). Since birth, Pt 1 presented numerous skin, upper respiratory tract, and lymph node infections that were characterized by fever and neutropenia. At 3 months she presented with urinary tract infection due to Klebsiella pneumoniae. Other infectious episodes were observed at 4 months and at 10 months, which were characterized by cutaneous abscesses, lymphoadenopathy, and fever, and required treatment with intravenous antibiotics. After starting G-CSF treatment (5 μg/kg), the child still experienced recurrent sinusitis and pneumonia. At 1 year of life, immunologic investigations revealed normal lymphocyte subpopulations (CD3, 57%; CD4, 33%; CD8, 21%; CD19, 32%) and normal lymphoproliferative response to mitogens. Serum immunoglobulin determination showed 0.3 g/L IgG, 0.025 g/L IgM, and undetectable IgA, but these values increased up to normal levels in the following years (0.7 g/L IgG, 0.05 g/L IgA, 0.05 g/L IgM at 7 years). Granulocyte-specific autoantibodies were absent, while bone marrow aspirates showed mild granulocytic hypoplasia without evidence of hemophagocytosis. The child presented normal antibody response to asymptomatic CMV and EBV infections. Approval for these studies was obtained from the Spedali Civili Brescia institutional review board. Informed consent was provided according to the Declaration of Helsinki.
PMN cell counts in patients with Hermansky-Pudlak 2
Pt 1 . | . | Pt 2 . | . | ||
|---|---|---|---|---|---|
| Age, wk . | PMN cells, × 109/L . | Age, wk . | PMN cells, × 109/L . | ||
| 16 | 0.445 | 13 | 0.162 | ||
| 17 | 0.768 | 22 | 0.401 | ||
| 18 | 0.176 | 30 | 0.341 | ||
| 19 | 0.738 | 39 | 0.068 | ||
| 33 | 0.785 | 58 | 0.422 | ||
Pt 1 . | . | Pt 2 . | . | ||
|---|---|---|---|---|---|
| Age, wk . | PMN cells, × 109/L . | Age, wk . | PMN cells, × 109/L . | ||
| 16 | 0.445 | 13 | 0.162 | ||
| 17 | 0.768 | 22 | 0.401 | ||
| 18 | 0.176 | 30 | 0.341 | ||
| 19 | 0.738 | 39 | 0.068 | ||
| 33 | 0.785 | 58 | 0.422 | ||
Determination of PMN cell counts in HPS2 children when they were without infections demonstrates that the extent of neutropenia is variable in these patients.
In Pt 2, neutropenia, partial albinism, and nystagmus were discovered in the first months of life. At 1 year, immunologic investigations demonstrated normal lymphocyte subpopulations (CD3, 74%; CD4, 61%; CD8, 11%; CD19, 14%) and normal lymphoproliferative response to mitogens. Immunoglobulin levels were slightly reduced (0.14 g/L IgG, 0.009 g/L IgA, 0.02 g/L IgM) but became normal at 2 years (1.1 g/L IgG, 0.08 g/L IgA, 0.025 g/L IgM). At 5 months, while neutropenia was observed, the bone marrow aspirates showed the presence of mature PMN cells and of all myeloid precursors. Later, the recurrence of acute otitis and bacterial skin infections prompted us to start G-CSF therapy. At 15 months, the patients presented fever, rash, diarrhea, splenomegaly, and pancytopenia (white blood cell [WBC] count, 2.2 × 109/L; PMN count, 0.16 × 109/L; red blood cell [RBC] count, 3.78 × 1012/L; hemoglobin, 76 g/L [7.6 g/dL]; platelet count, 54 × 109/L), while C-reactive protein, liver enzymes, ferritin, cholesterol, and triglycerides were normal. Analysis of lymphocyte subpopulations revealed a marked increase of the CD8 subset (CD3, 41%; CD4, 17%; CD8, 20%). After detection of CMV-DNA and high levels of anti-CMV IgG and IgM, we started a treatment with the antiviral drug foscarnet. This therapy led to complete recovery, while CMV-DNA became undetectable in the blood.
Investigation of NK cells in the 2 patients demonstrated a reduction of NK cytolytic activity, while their blood numbers (CD16: Pt 1, 10%; Pt 2, 8%) were normal or slightly reduced as compared with control subjects (CD16 normal range, 8% to 20%). While Pt 1 never showed recurrent epistaxis or other hemorrhagic episodes, Pt 2 presented prolonged bleeding after tooth removal. In both patients, platelet aggregation tests were abnormal upon stimulation with collagen and adenosine diphosphate but normal with ristocetin and epinephrine. Molecular analysis of the ELA2 and RAB27A genes, which are responsible, respectively, for severe chronic neutropenia and Griscelli syndrome, ruled out these 2 conditions.
For each experiment, blood was drawn when the patients were free of infections. For each experiment performed, at least one healthy subject and/or one age-matched child, who was admitted to the hospital for minor head trauma, were included for comparison.
Mutational analysis
DNA was extracted from peripheral blood leukocytes using standard techniques. All 27 exons of ADTB3A and at least 15 bases of flanking regions were amplified by polymerase chain reaction (PCR) (primers and amplification conditions available upon request). PCR products were purified and bidirectionally sequenced as previously described28 using Big Dye Terminator Chemistry (Applied Biosystems, Weiterstadt, Germany) on an ABI PRISM 310 Genetic Analyzer (Applied Biosystems). For each new mutation found, at least 50 healthy unrelated controls were screened using PCR amplification and direct sequencing. Primers and PCR conditions used for this analysis are available upon request.
Western blotting analysis
Peripheral neutrophil cells were purified by Ficoll-Hypaque separation density gradient centrifugation (Amersham Pharmacia Biotech, Uppsala, Sweden), followed by red cell lysis (NH4Cl, 0.829%; EDTA, 0.125 mM; NaH2CO3, 0.1%) and washing with PBS. Neutrophil lysates were obtained after incubation of cells with 1 mM DFP (Sigma-Aldrich, St. Louis, MO) and lysed as previously described.29 NK lysates were obtained as described.1
Proteins were separated using denaturing polyacrylamide gel electrophoresis (SDS-PAGE) and transferred to nitrocellulose membrane for immunoblotting. Primary antibodies were used at 1:1000 for rabbit polyclonal antibodies to human NE (Calbiochem, San Diego, CA), 1:500 anti-σ, 1:200 anti-δ, 1:200 anti-μ3A, and 1:100 anti-β3A (gifts from M. S. Robinson, Cambridge Institute for Medical Research, United Kingdom). Secondary detection was performed by adding a 1:10 000 dilution of peroxidase-conjugated antirabbit or antimouse antibody (Jackson ImmunoResearch Laboratories, Bar Harbor, ME) using enhanced chemiluminescence (ECL) (Amersham Pharmacia Biotech). The blots were stripped and reprobed with mouse mAb to human β-actin (Sigma-Aldrich) to standardize for variations in protein loading.
PBMCs, NK cells, and neutrophil purification and culture
Peripheral blood mononuclear cells (PBMCs) were obtained from heparinized blood by density gradient centrifugation over Ficoll (Sigma-Aldrich). PBMCs were resuspended in RPMI 1640 medium; supplemented with 2 mM glutamine, 50 μg/mL penicillin, 50 μg/mL streptomycin, and 10% heat-inactivated FCS (PAA Laboratories, Linz, Austria); and cultured in the presence of 100 IU rIL-2 (aldesleukin; Chiron, Emeryville, CA) during overnight incubation.
NK cells were purified by NK-cell separation cocktails (Rosette Sep; StemCell Technologies, Vancouver, BC, Canada). The purity of NK cells was more than 96% as assessed by flow cytometric analysis of cells stained with a mixture of CD56-PC5 and CD3-FITC (Beckman Coulter, Immunotech, Marseille, France). CD3 contamination in purified NK cells was less than 1%.
Purified NK cells were cultured on irradiated feeder cells in the presence of 100 U/mL rIL-2 and 1.5 ng/mL PHA (Gibco, Paisley, Scotland) to obtain activated polyclonal NK-cell populations.
Neutrophils were purified by Ficoll-Hypaque separation density gradient centrifugation (Amersham Pharmacia Biotech) followed by red cell lysis (NH4Cl, 0829%; EDTA, 0.125 mM; NaH2CO3, 0.1%) and washing with PBS.
Monoclonal antibodies and cytofluorimetric analysis
The following mAbs, produced in one of our laboratories, were used in this study: BAB281 and KL247 (IgG1 and IgM, respectively, anti-NKp46), Z25 and F252 (IgG1 and IgM, respectively, anti-NKp30), ON72 (IgG1, anti-NKG2D), c127 (IgG1, anti-CD16), c218 and FS280 (IgG1 and IgG2a, respectively, anti-CD56), PP35 (IgG1, anti-CD244), A6/136 (IgM, anti-HLA class I), 3C8 (IgM, anti-CD63). A mixture of PC5-conjugated anti-CD56 mAb and FITC-conjugated anti-CD3 mAb was purchased from Beckman Coulter, Immunotech.
Perforin and granzyme B cytofluorimeter expression analysis in NK cells was performed by staining with purified antiperforin mAb (Ancell, Bayport, MN) and purified anti–granzyme B mAb (Alexis Biochemicals, San Diego, CA), respectively, after the cells were fixed in 1% paraformaldehyde and permeabilized. For 1- or 2-color cytofluorimetric analysis, cells were stained with the appropriate mAbs followed by PE- or FITC-conjugated isotype-specific goat antimouse secondary antibody (Southern Biotechnology, Birmingham, AL). Cell acquisition was performed on a FACScan flow cytometer (Becton Dickinson, Mountain View, CA) and data analyzed using the CellQuest software (Becton Dickinson, Mountain View, CA).
Neutrophils were incubated at 4°C with the murine monoclonal PE-conjugated anti-CD63 antibody or an isotype-matched monoclonal antibody, both from Becton Dickinson (Mountain View, CA). Cells were washed twice with PBS plus 0.5% calf serum albumin and analyzed with FACSCalibur with the CellQuest software from Becton Dickinson (Mountain View, CA). At least 500 000 events were accumulated for fluorescence analysis.
Real-time PCR
RNA was purified from whole frozen NK cells using the guanidium thiocyanate-phenol-chloroform method according to the instruction manual (RNAwiz; Ambion, Austin, TX). One microgram of total RNA was used to synthesize the first strand of cDNA using the GeneAmpRNA PCR kit (Applied Biosystems). For real-time PCR analysis, Assays-on-Demand Products (20X) and Taqman Master Mix (2X) from Applied Biosystems were used to amplify perforin and RNAse P mRNAs according to the instruction manual. Reactions were run on ABI Prism 7700 Sequence Detection System (Applied Biosystems) in a final volume of 25 μL for 50 cycles. Perforin expression was normalized to RNAse P levels in each sample.
Cytolytic activity
PBMCs (exposed or not to rIL-2) and polyclonal rIL-2–activated NK cells were tested for cytolytic activity against various NK-susceptible tumor target cells including K562 and LCL 721.221 in a 4-hour 51Cr-release assay as previously described.30 In other experiments their cytolytic activity was evaluated against autologous or heterologous PHA blasts obtained as previously described.31 The concentration of anti-HLA class I mAb used for these experiments was 10 μg/mL. The effector-target (E/T) ratios are indicated in the figure legends.
Immunofluorescence staining
PMN and NK cells were obtained as reported in “PBMCs, NK cells, and neutrophil purification and culture.” Cells were counted and used for cytospin preparations. Slides were air-dried and used for immunofluorescence staining. Primary antibodies included in this study included anti–human NE mAb clone NP57 at dilution 1:25 (Dako Cytomation, Glostrup, Denmark), anti-NE rabbit polyclonal (Calbiochem) at dilution 1:300, anti–human perforin (1:500, clone dG9; Becton Dickinson, Oxford, United Kingdom), rabbit anti–cathepsin D (Upstate Biotechnology, Lake Placid, NY), and rabbit anti–Lamp-2 (AS120, 1:200) and a pool of anti–human granzyme B (clone GRB7, 1:20, Valter Occhiena, Milan, Italy; clone GZB01, 1:20, Biocarta, Hamburg, Germany; clone 11F1, 1:20, Novocastra, Newcastle upon Tyne, United Kingdom). For double immunofluorescence of PMN cells, rabbit anti–human elastase and mouse anti-CD43 (1:25, clone MT1; Novocastra) were used; elastase was revealed with swine antirabbit FITC-conjugated antibody (1:25; Dako Cytomation) and CD43 with Texas-Red–conjugated goat anti–mouse IgG1 (1:75; Southern Biotechnology Associates). For immunofluorescence of NK cells confocal microscopy was performed as described.1 Briefly, cells were attached to glass slides in serum-free medium for 10 to 20 minutes, fixed in –20°C methanol for 5 minutes, rinsed in PBS, preblocked in PBS, 1% normal goat serum for 15 minutes, and incubated with primary antibodies in PBS, 1% BSA for 40 minutes at room temperature. Cells were washed 3 to 4 times in PBS, 1% BSA and incubated with secondary antibody for 30 minutes at room temperature, washed 5 to 6 times in PBS, 1% BSA, and mounted in PBS, 90% glycerol 2.5% DABCO.
Results
Identification of 2 novel mutations in β3A gene and immunoblotting analysis of AP-3 complex subunits
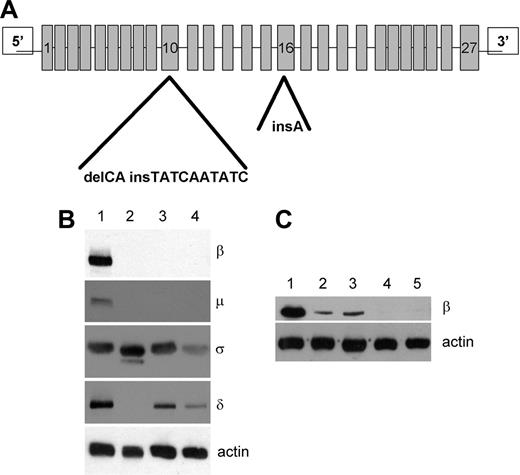
Molecular analysis of the 27 exons of the β3A gene (ADTB3A) showed that the 2 siblings were compound heterozygous for 2 novel mutations. The same mutations were also identified in the heterozygous state in the parents. (Figure 1A). In the mother we have detected a deletion of the dinucleotide CA at position 1063-1064 of the coding region and substitution with the sequence TATCAATATC. The deletion/insertion mutation leads to a frame shift in the coding sequence and consequently to premature termination of protein synthesis (Q355fsX360). In both patients and in their father, we have identified a single base insertion (A) in position 1789-1790 of the coding region (exon 16), leading to frame shift and to generation of a stop codon (I597fsX608). Molecular analysis of the μ3A gene did not reveal any mutations in the coding regions of both patients.
To evaluate protein expression of the AP-3 complex subunits at the protein level, we performed immunoblotting analysis of cell lysates of CTLs with antibodies directed against each subunit of the complex. We found that the β3A and μ3A subunits were undetectable in lysates from both affected children. Analysis of δ and σ3 subunits in the same lysates showed that these 2 components of AP-3 complex were present at reduced levels in the HPS2 patients (Figure 1B, lanes 3 and 4) as compared with the control (Figure 1B, lane 1). In contrast, only the σ3 subunit could be detected in a previously reported HPS2 patient.1 Using increased levels of protein, very low levels of β3A were detected in the previously reported patient (Figure 1C, lanes 2 and 3), while Pt 1 and Pt 2 from this study show a complete absence of β3A, consistent with the genetic mutations identified.
Composite heterozygousADTB3Amutation in 2 novel HPS2 patients. (A) Mutational analysis of ADTB3A in 2 patients (Pt 1 and Pt 2) and their parents showed 2 novel mutations. The mother and both the children (Pt 1, Pt 2) present a deletion/insertion in exon 10 at position 1063-1064 of the coding region. C and A are substituted by a 10-base sequence: TATCAATATC. The frame shift in the coding sequence (from the Q at 355 position) leads to a stop codon at position 360 (Q355fsX360). The father and the 2 patients carry a single A insertion at position 1789-1790 in the exon 16, leading to a frame shift (from I at 597 position) and to a stop codon at amino acidic residue 608 (I597fsX608). (B) Cell lysates from both HPS2 Pt 1 and Pt 2 (lanes 3 and 4), a previously identified HPS2 patient1 (lane 2), and a control subject (lane 1) were separated by SDS-PAGE and probed for the AP-3 subunits (see “Patients, materials, and methods”). Lysates contained 2 × 107 cells per milliliter. β-actin was used to compare protein levels. (C) Western blot probed with anti-β3A using lysates from control (lane 1), the previously identified HPS2 patient1 using lysates with 4 × 107 (lane 2) and 8 × 107 (lane 3) cells per milliliter, and 4 × 107 from HPS2 patients Pt 1 (lane 4) and Pt 2 (lane 5). β-actin was used to compare protein levels.
Composite heterozygousADTB3Amutation in 2 novel HPS2 patients. (A) Mutational analysis of ADTB3A in 2 patients (Pt 1 and Pt 2) and their parents showed 2 novel mutations. The mother and both the children (Pt 1, Pt 2) present a deletion/insertion in exon 10 at position 1063-1064 of the coding region. C and A are substituted by a 10-base sequence: TATCAATATC. The frame shift in the coding sequence (from the Q at 355 position) leads to a stop codon at position 360 (Q355fsX360). The father and the 2 patients carry a single A insertion at position 1789-1790 in the exon 16, leading to a frame shift (from I at 597 position) and to a stop codon at amino acidic residue 608 (I597fsX608). (B) Cell lysates from both HPS2 Pt 1 and Pt 2 (lanes 3 and 4), a previously identified HPS2 patient1 (lane 2), and a control subject (lane 1) were separated by SDS-PAGE and probed for the AP-3 subunits (see “Patients, materials, and methods”). Lysates contained 2 × 107 cells per milliliter. β-actin was used to compare protein levels. (C) Western blot probed with anti-β3A using lysates from control (lane 1), the previously identified HPS2 patient1 using lysates with 4 × 107 (lane 2) and 8 × 107 (lane 3) cells per milliliter, and 4 × 107 from HPS2 patients Pt 1 (lane 4) and Pt 2 (lane 5). β-actin was used to compare protein levels.
These results therefore suggest that the σ3 and δ can interact and constitute a stable σ3-δ complex when the β3A subunit is completely absent, but the presence of a residual amount of β3A might interfere with the interaction between σ3 and δ, thereby leading to degradation of the δ subunit. These results are consistent with previous reports that have demonstrated that the σ3 subunit has a direct interaction with the δ subunit.1,9,13,15,32
Altered expression of CD63 and neutrophil elastase in circulating neutrophils of HPS2 patients
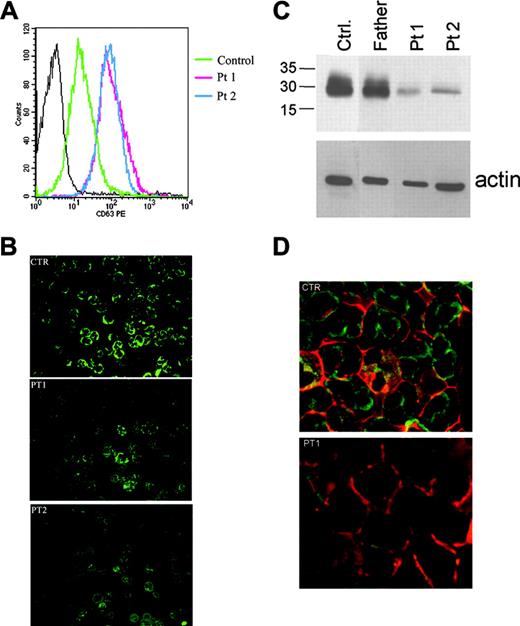
CD63 is expressed in neutrophils as a membrane protein of azurophil granules and is mobilized to the plasma membrane after in vitro chemoattractant-induced stimulation and degranulation.33 Previous studies performed in fibroblasts and in CTLs of HPS2 patients showed increased levels of this membrane protein in the plasma membrane.1,9,15 Therefore, we analyzed cell surface levels of CD63 in neutrophils of HPS2 patients by flow cytometry. In both patients, we observed a remarkable increase of steady-state levels of CD63 on the cell surface as compared with control subjects (Figure 2A). This observation suggests that disruption of the AP-3 complex may lead to direct routing of CD63 to the plasma membrane without transit through azurophil granules.
Because NE is stored in the azurophil granules and is required for normal differentiation of myeloid progenitors to mature neutrophils, we analyzed NE expression in cells of HPS2 patients by immunofluorescence. After PMN separation and cytospin preparation, cells were stained with anti-NE polyclonal antibody. Analysis of PMN cells obtained from both HPS2 patients revealed few NE-positive granules scattered in the cytoplasm of neutrophils from HPS2 patients (Figure 2B). In contrast, immunofluorescence staining of normal cells showed a strong cytoplasmic reactivity and multiple NE-positive intracytoplasmic granules.
Increased cell surface expression of CD63 and reduced elastase levels in HPS2 patients. (A) Circulating neutrophils were separated as described in “Patients, materials, and methods,” washed twice, and analyzed by a flow cytometer for expression of CD63. CD63 staining (thick line) in comparison with mouse IgG antibody (thin line) is presented on a histogram plot. Red fluorescence intensity is shown on the x-axis expressed in a log scale; the number of cells per channel is shown on the y-axis. Experiment shown is representative of 3 independent experiments performed. (B) Immunofluorescence staining for NE in circulating neutrophils from HPS2 patients. PMN cells were obtained from peripheral blood, cytocentrifuged, and stained with anti-NE. In cells from a control subject, a strong expression of NE is observed in the cytoplasm with the presence of cytoplasmic dots (top panel). In patients (Pt 1 and Pt 2), only scattered NE-positive dots are evident (middle and bottom panels) in rare PMN cells. NE was revealed using FITC-conjugated secondary antibody. Experiment shown is representative of 2 performed. (C) Western blot analysis for NE in circulating neutrophil content for HPS2 patients. Cell lysates from separated neutrophils of Pt 1, Pt 2, their father, and a healthy control were separated by SDS-PAGE and probed with NE antibody (see “Patients, materials, and methods”). β-actin was used to compare protein levels. (D) Confocal microscopy analysis of double immunofluorescence staining of PMN cells from HPS Pt 1 with antielastase (green) and anti-CD43 (red) was performed as described in “Patients, materials, and methods.” Experiment shown is representative of 2 performed. Sections were examined using an Olympus BX60 fluorescence microscope and objectives with numeric apertures of 0.40 (10 ×), 0.70 (20 ×), 0.85 (40 ×), and 0.90 (60 ×), equipped with a DP-70 Olympus digital camera (Olympus, Melville, NY). Images were acquired using analySIS Image Processing software (Soft Imaging System, Münster, Germany).
Increased cell surface expression of CD63 and reduced elastase levels in HPS2 patients. (A) Circulating neutrophils were separated as described in “Patients, materials, and methods,” washed twice, and analyzed by a flow cytometer for expression of CD63. CD63 staining (thick line) in comparison with mouse IgG antibody (thin line) is presented on a histogram plot. Red fluorescence intensity is shown on the x-axis expressed in a log scale; the number of cells per channel is shown on the y-axis. Experiment shown is representative of 3 independent experiments performed. (B) Immunofluorescence staining for NE in circulating neutrophils from HPS2 patients. PMN cells were obtained from peripheral blood, cytocentrifuged, and stained with anti-NE. In cells from a control subject, a strong expression of NE is observed in the cytoplasm with the presence of cytoplasmic dots (top panel). In patients (Pt 1 and Pt 2), only scattered NE-positive dots are evident (middle and bottom panels) in rare PMN cells. NE was revealed using FITC-conjugated secondary antibody. Experiment shown is representative of 2 performed. (C) Western blot analysis for NE in circulating neutrophil content for HPS2 patients. Cell lysates from separated neutrophils of Pt 1, Pt 2, their father, and a healthy control were separated by SDS-PAGE and probed with NE antibody (see “Patients, materials, and methods”). β-actin was used to compare protein levels. (D) Confocal microscopy analysis of double immunofluorescence staining of PMN cells from HPS Pt 1 with antielastase (green) and anti-CD43 (red) was performed as described in “Patients, materials, and methods.” Experiment shown is representative of 2 performed. Sections were examined using an Olympus BX60 fluorescence microscope and objectives with numeric apertures of 0.40 (10 ×), 0.70 (20 ×), 0.85 (40 ×), and 0.90 (60 ×), equipped with a DP-70 Olympus digital camera (Olympus, Melville, NY). Images were acquired using analySIS Image Processing software (Soft Imaging System, Münster, Germany).
For quantitative analysis of NE content of PMN cells from HPS2 patients, we determined protein levels by immunoblotting. We found a dramatic reduction in NE content in HPS2 neutrophils in comparison with cells from healthy donors (Figure 2C). Taken together, these data suggest that loss of the AP-3 complex leads to impaired expression of NE.
To determine cellular localization of NE we performed double immunofluorescence staining with FITC-conjugated anti-NE combined with the cell surface marker CD43 conjugated to Texas-Red in PMN cells of HPS2 patients. We found that in PMN cells of control subjects NE was predominantly located in the perinuclear cytoplasmic area, whereas in HPS2 patients it was mostly confined to the cell membrane and submembranous area, where it colocalized with CD43 (Figure 2D).
Defective cytolytic activity by NK cells of HPS2 patients
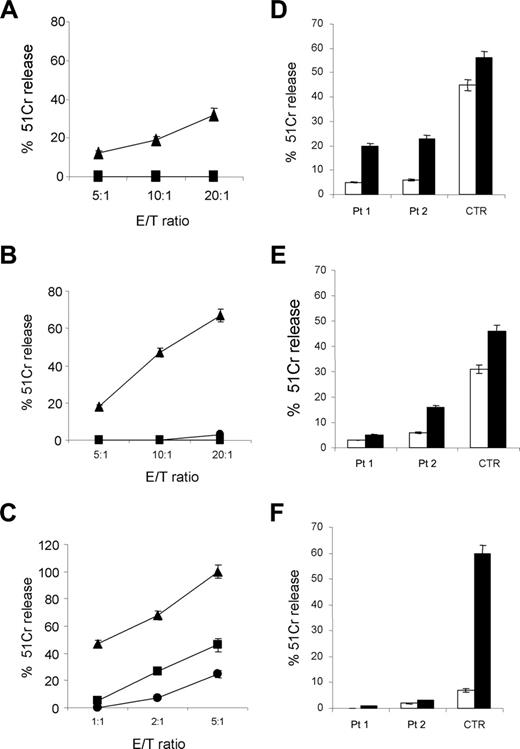
Freshly isolated PBMCs from Pt 1 and Pt 2 were analyzed for cytolytic activity before and after overnight culture in the presence of rIL-2 against the NK-susceptible erythroleukemia cell line K562 (Figure 3A-B, respectively). Remarkably, the cytolytic activity of both of these cells was dramatically reduced when compared with that of a representative healthy control. Because it has been shown that low NK-mediated cytolytic activity may correlate with reduced expression of certain activating receptors,34 we evaluated the surface density of NKp30, NKp46, NKG2D, and CD244 (2B4) molecules in purified HPS2 patients' NK cells that had been cultured in the presence of rIL-2 for 3 weeks. These polyclonal rIL-2–activated NK cells did not display significant phenotypic variations as compared with NK cells derived from healthy donors cultured under the same conditions (data not shown). The same rIL-2–activated NK-cell populations, tested against the LCL 721.221 cell line, displayed a strongly reduced cytolytic activity as compared with a representative healthy control (Figure 3C).
Next, we evaluated the ability of cultured patient's NK cells to kill autologous or heterologous PHA blasts in the presence or absence of anti-HLA class I mAbs. In all instances, NK cells from healthy controls and from patients were unable to kill autologous PHA blasts (Figure 3D-F).
Notably, however, while the cytolytic activity of control NK cells could be strongly restored in the presence of anti-HLA class I mAbs (Figure 3F), only little increases were detected with HPS2 NK cells (Figure 3D-E). Moreover, HPS2 NK cells, unlike control cells, were poorly lytic also against allogeneic PHA blasts both in the absence or in the presence of anti-HLA class I mAbs. Altogether these results indicate that NK cells from Pt 1 and Pt 2 are characterized by a significantly reduced capability to mediate cytolytic activity although displaying normal levels of surface triggering receptors.
Reduced perforin content of NK cells in HPS2 patients
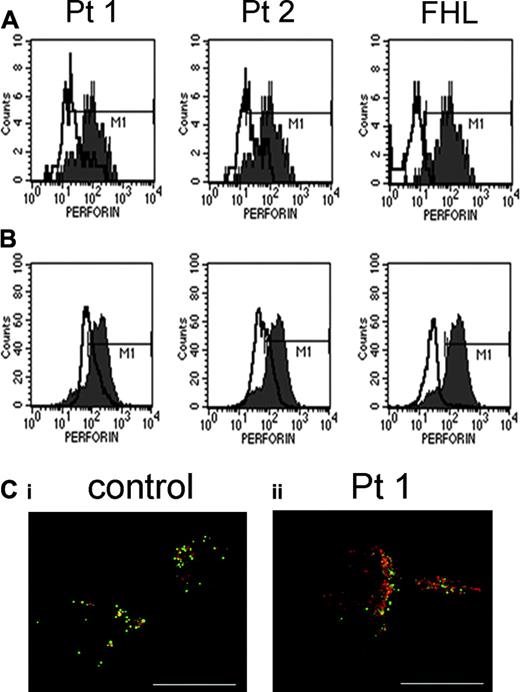
We have quantitatively examined the levels of perforin in freshly isolated and in cultured HPS2 polyclonal NK cells by intracellular staining and flow cytometry. As shown in Figure 4, resting NK cells (Figure 4A) and activated NK cells (Figure 4B) from HPS2 patients and from a perforin-deficient subject displayed a significant reduction in perforin content as compared with a representative control. Notably, the perforin content of NK cells from HPS2 patients was lower than control NK cells yet higher than perforin levels detected in a previously described perforin-deficient individual who completely lacked the expression of this molecule,35 whereas the levels of granzyme B did not display detectable variations (data not shown). The difference in perforin levels is less marked in activated NK cells as seen by flow cytometry (Figure 4B) and is not detectable by the less sensitive immunofluorescence microscopy (Figure 4C). Consistent with this finding, evaluation of perforin expression by real-time PCR in activated NK cells of HPS2 patients did not show differences in mRNA levels in cells from control subjects.
Impairment of cytolytic activity of fresh and IL-2–stimulated NK cells in HPS2 patients. Defective cytolytic activity of HPS2 patients against NK-susceptible target cells. Freshly isolated PBMCs derived from Pt 1 (•) or Pt 2 (▪) were tested against the K562 target cells either before (A) or after overnight incubation in the presence of rIL-2 (B) and compared with a representative healthy donor (▴) at different E/T ratios. Purified polyclonal rIL-2–activated NK cells, derived from Pt 1 (•) or Pt 2 (▪) or a healthy donor (▴), were tested against the NK-susceptible LCL 721.221 target cells at different E/T ratios (C). These experiments are representative of 6 independent experiments. Defective killing of autologous or heterologous PHA blasts by HPS2 patients' NK cells. The cytolytic activity of purified polyclonal rIL-2–activated NK cells was evaluated against autologous or heterologous PHA blasts derived from Pt 1 (D) or Pt 2 (E) or a representative healthy donor (F) at an E/T ratio of 25:1, either in the absence (□) or in the presence (▪) of anti-HLA class I mAb. These experiments are representative of 10 independent experiments. Data indicate the mean ± SD of 3 replicates.
Impairment of cytolytic activity of fresh and IL-2–stimulated NK cells in HPS2 patients. Defective cytolytic activity of HPS2 patients against NK-susceptible target cells. Freshly isolated PBMCs derived from Pt 1 (•) or Pt 2 (▪) were tested against the K562 target cells either before (A) or after overnight incubation in the presence of rIL-2 (B) and compared with a representative healthy donor (▴) at different E/T ratios. Purified polyclonal rIL-2–activated NK cells, derived from Pt 1 (•) or Pt 2 (▪) or a healthy donor (▴), were tested against the NK-susceptible LCL 721.221 target cells at different E/T ratios (C). These experiments are representative of 6 independent experiments. Defective killing of autologous or heterologous PHA blasts by HPS2 patients' NK cells. The cytolytic activity of purified polyclonal rIL-2–activated NK cells was evaluated against autologous or heterologous PHA blasts derived from Pt 1 (D) or Pt 2 (E) or a representative healthy donor (F) at an E/T ratio of 25:1, either in the absence (□) or in the presence (▪) of anti-HLA class I mAb. These experiments are representative of 10 independent experiments. Data indicate the mean ± SD of 3 replicates.
Confocal microscopy showed that perforin staining colocalized with the lysosomal membrane protein, Lamp-2, in activated NK cells (Figure 4C) demonstrating that perforin is correctly sorted to lysosomes of NK cells from HPS2 patients. Western blot analysis revealed that the mature processed form is present in both controls and HPS2 NK lysates, demonstrating that biosynthetic processing is normal in the patients (data not shown).
Reduced perforin expression in resting and activated NK cells of HPS2 patients. Expression profiles of perforin (mAb deltaG9) in unstimulated (A) and activated NK cells (B) from HPS2 patients (empty histograms) and from a perforin-deficient patient were overlaid with that of a healthy donor (filled histogram) to directly compare their fluorescence's mean. Pt 1: left panels; Pt 2: middle panels; perforin-deficient patient (FHL): right panels. Isotype-matched mouse IgG stained less than 0.1 % of cells. Expression of perforin was evaluated in parallel in NK cells from 10 healthy individuals. These experiments are representative of 5 independent experiments. (C) Confocal microscopy of perforin in IL-2–activated NK cells of HPS2 patients. NK cells from control donor (i) and Pt 1 (ii) were stained with antibodies against perforin (green) and Lamp-2 (red) as described in “Patients, materials, and methods.” Scale bars, 10 μm. Samples were analyzed using a Zeiss Axioplan 2 microscope (Carl Zeiss, Hertfordshire, United Kingdom) with Zeiss Plan-NEOFLUAR 100/1.3NA lenses mounted with a CoolSnap HQ camera (Roper Scientific, Tucson, AZ). Images were processed using Metamorph software (Molecular Devices, Downingtown, PA) and AutoDeblur + Autovisualize software (AutoQuant Imaging, Watervliet, NY).
Reduced perforin expression in resting and activated NK cells of HPS2 patients. Expression profiles of perforin (mAb deltaG9) in unstimulated (A) and activated NK cells (B) from HPS2 patients (empty histograms) and from a perforin-deficient patient were overlaid with that of a healthy donor (filled histogram) to directly compare their fluorescence's mean. Pt 1: left panels; Pt 2: middle panels; perforin-deficient patient (FHL): right panels. Isotype-matched mouse IgG stained less than 0.1 % of cells. Expression of perforin was evaluated in parallel in NK cells from 10 healthy individuals. These experiments are representative of 5 independent experiments. (C) Confocal microscopy of perforin in IL-2–activated NK cells of HPS2 patients. NK cells from control donor (i) and Pt 1 (ii) were stained with antibodies against perforin (green) and Lamp-2 (red) as described in “Patients, materials, and methods.” Scale bars, 10 μm. Samples were analyzed using a Zeiss Axioplan 2 microscope (Carl Zeiss, Hertfordshire, United Kingdom) with Zeiss Plan-NEOFLUAR 100/1.3NA lenses mounted with a CoolSnap HQ camera (Roper Scientific, Tucson, AZ). Images were processed using Metamorph software (Molecular Devices, Downingtown, PA) and AutoDeblur + Autovisualize software (AutoQuant Imaging, Watervliet, NY).
Discussion
Although the AP-3 complex is ubiquitously expressed, its absence leads to selected dysfunction of cells in the hematopoietic system and skin.6-8 Other immunodeficiencies such as Chediak-Higashi syndrome (CHS) and Griscelli syndrome (GS) are characterized by the association of albinism with functional defects of neutrophils and NK cells.21-27 Similar to melanocytes, certain hematopoietic cells such as NK cells and neutrophils display a well-organized array of cytoplasmic organelles and secretory lysosomes that require a complex machinery for lysosomal biogenesis and mobilization. Both CHS and GS are characterized by a generalized defect of biogenesis and/or mobilization of lysosomes that affect the intracellular trafficking of all lysosome-associated glycoproteins.36 In contrast, Hermansky-Pudlak syndrome type 2 is characterized by a selective defect in the AP-3 complex that is essential for protein sorting from the trans-Golgi network to lysosomes or to lysosome-like organelles.6-12 Mutations of the ADTB3A gene in patients with HPS2 resulting in loss or absence of the β3A subunit lead to loss of stability of the complex and loss of expression of other subunits.1,9,15,32 In the absence of a functional AP-3 as the tetraspanin CD63, which is normally targeted to lysosomes or to lysosome-like vesicles such as azurophil granules, traffics to the plasma membrane.37 Previous observations that cell-surface expression of CD63 is increased in fibroblasts and CTLs of HPS2 patients suggest that CD63 is routed to lysosome-like organelles by interaction with AP-3 in all these cell types.1,9,15 In neutrophils of healthy subjects, CD63 is retained in the membranes of cytoplasmic azurophil granules, suggesting that lack of AP-3 results in change in the steady-state distribution of the membrane protein between intracellular vesicles and the plasma membrane.20 In an alternative hypothesis, missorting of CD63 in neutrophils of AP-3–deficient patients might be caused by dysfunction of an endocytic pathway that requires the AP-3 complex to endocytose CD63 from the plasma membrane. The hypothesis that CD63 might be delivered to azurophil granules by AP-3 is in agreement with the observation made in granulocytes of the gray collie that AP-3 directs another protein associated to azurophil granules, NE, through the μ3A sorting signal. In these dogs, which have hypopigmented coats and cyclic neutropenia resembling Hermansky-Pudlak syndrome type 2, Benson et al20 have reported that absence of the β3A subunit of the AP-3 complex causes mislocation of NE to the plasma membrane. In our 2 patients affected with HPS2, we have observed a severe defect of NE expression as measured by immunofluorescence and by Western blot analysis and its colocalization with the cell surface marker CD43. These novel findings provide an explanation for the neutropenia that is observed in HPS2 patients. It is likely that in cells lacking the AP-3 transport machinery, abnormal trafficking of NE might lead to early degradation of the protein, thereby accounting for the quantitative reduction in protein expression.
Taken together, these results suggest that normal expression and correct sorting of NE in azurophil granules of myeloid progenitors constitutes an essential step in neutrophil maturation. Accordingly, in severe congenital neutropenia, mutations of ELA2 lead to synthesis of an altered protein that cannot interact with the AP-3 complex, thereby leading to a maturation block in myeloid differentiation exactly at the stage when azurophil granules are formed.20
Although neutropenia and recurrent infections were observed in all the HPS2 patients identified so far,13,15 it is interesting that in the 2 patients that were reported by Shotelersuk et al13 diagnosis of Hermanksy-Pudlak type 2 was made in adulthood, suggesting that their clinical manifestations of immunodeficiency were not severe. It is conceivable that the heterogeneity in the age of onset of the disease might reflect the different mutations of ADTB3A that have been identified in these cases. In fact, the child described by Huizing et al15 as well as our 2 HPS2 patients presented severe mutations, including deletion and nonsense mutations that lead to complete loss of protein synthesis. In contrast, the patients described by Shotelersuk et al13 presented a deletion (1166A∼1228C del 63 bp [in frame]) in 1 allele and a missense mutation (1739T>G) leading to amino acid substitution (L580R) in the other allele, possibly accounting for the leaky phenotype and for the late diagnosis in these HPS2 patients.
Besides a quantitative defect of neutrophils in HPS2 patients, we have also observed a reduced capability of NK cells to mediate cytolytic activity. Previous studies of NK-cell activities in patients affected by HPS2 have shown conflicting results; while systematic assessment of immunologic functions in large cohorts of HPS patients failed to reveal abnormal leukocyte counts or NK cytolytic activity,38 a patient with recurrent infections and impairment of NK functions has also been reported.39 Because the cohort studies were performed evaluating genetically uncharacterized patients showing oculocutaneous albinism and bleeding disorders, lacking symptoms of immunodeficiency, this suggests that many of them were suffering from other forms of HPS2. In our patients, we found that NK-cell defect was especially evident in freshly isolated NK cells evaluated against susceptible targets34 while it was less severe when IL-2–activated NK cells were analyzed. Moreover, NK cells of both HPS2 patients did not show abnormal expression of activating receptors, suggesting that an intrinsic defect of NK cytolytic machinery might account for this functional defect.40 Investigation of lysosomal protein content in NK cells of HPS2 patients demonstrated decreased levels of perforin in freshly isolated and, at a lower extent, in activated NK cells. This does not appear to reflect a targeting defect because perforin colocalizes with Lamp-2 and is fully processed to the mature form, a step that requires proteolytic cleavage and most likely occurs in the granule. Loss of lysosomal polarization was observed in CTLs of HPS2 patients, suggesting that AP-3–sorted lysosomal proteins are required for mediating movement of secretory lysosomes toward the immunologic synapse.1
Comparison of perforin content in NK cells of HPS2 patients with levels detected in a patient with familial hemophagocytic lymphohistiocytosis (FHL) due to perforin deficiency35 reveals that HPS2 patients display a partial defect of the protein. This is reflected in the incomplete defect of cytolytic activity and in the preserved immune response against viral infections. Nevertheless, 1 of the 2 HPS2 patients displayed an episode of pancytopenia after CMV infection that was associated to expansion of the CD8 subset. Although hemophagocytosis was never observed in these patients, these manifestations suggest that HPS2 patients have a broad defect of innate immunity that results in wide-ranging susceptibility to bacterial and viral infection. Careful follow-up of these patients will be important to evaluate whether the therapy with G-CSF is sufficient for prophylaxis of infections or other therapeutic measures are needed.
The ubiquitous expression of AP-3 and its role in protein sorting in exocytic and endocytic pathways contrasts with clinical manifestations of HPS2 that are selectively restricted to skin pigmentation and to differentiation and function of neutrophils, CTLs, and NK cells. It is interesting that phylogenetic analysis of adaptor protein complexes demonstrates that these important cytosolic proteins evolved early but then were lost in some organisms, perhaps because of lack of selective pressure.3,41 In vertebrates, these intracellular transporters of secretory proteins may have acquired specialized nonredundant functions in trafficking of proteins of hematopoietic cells of the innate immune system, owing to the increasing pressure of microbial infections in evolved organisms. This hypothesis may account for the link between albinism and immunodeficiency that has been observed in many inherited conditions including HPS2.
Prepublished online as Blood First Edition Paper, February 28, 2006; DOI 10.1182/blood-2005-11-4398.
Supported by grants from the Ministero dell'Università e della Ricerca Scientifica e Tecnologica (MIUR) Cofin 2004; European Union policy-oriented and harmonising research activities in the field of primary immunodeficiencies (EURO-POLICY-PID) contract S823-CT-2005-006411 (Luigi D.N.); MIUR (Centro per l'Innovazione Diagnostica e Terapeutica [IDET]), Cofin 2005 (R.B.); Fondo per gli Investimenti della Ricerca di Base (FIRB) (Luigi D.N.); Fondazione Berlucchi (Luigi D.N.); Istituto Superiore di Sanità (ISS) grant 40F.37 (F.F.); European Union grant QLR-2000-01395; and the Associazione Italiana per la Ricerca sul Cancro (AIRC), ISS, Ministero della Sanità, MIUR, the European Union FP6, LSHB-CT-2004-503319-AlloStem. In addition, the financial support of Fondazione Compagnia di San Paolo, Turin, Italy, is gratefully acknowledged. G.M.G. is supported by the Wellcome Trust, UK.
S.F. and S.P. contributed equally to this work.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 U.S.C. section 1734.
We are grateful to Silvia Costa for help in neutrophil separation and Amerigo Santoro for his superb support with confocal microscopy.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal