Abstract
The mechanism by which paroxysmal nocturnal hemoglobinuria (PNH) clones expand is unknown. PNH clones harbor PIGA mutations and do not synthesize glycosylphosphatidylinositol (GPI), resulting in deficiency of GPI-linked membrane proteins. GPI-deficient blood cells often expand in patients with aplastic anemia who sustain immune-mediated marrow injury putatively induced by cytotoxic cells, hence suggesting that the injury allows PNH clones to expand selectively. We previously reported that leukemic K562 cells preferentially survived natural killer (NK) cell-mediated cytotoxicity in vitro when they acquired PIGA mutations. We herein show that the survival is ascribable to the deficiency of stress-inducible GPI-linked membrane proteins ULBP1 and ULBP2, which activate NK and T cells. The ULBPs were detected on GPI-expressing but not on GPI-deficient K562 cells. In the presence of antibodies to either the ULBPs or their receptor NKG2D on NK cells, GPI-expressing cells were as less NK sensitive as GPI-deficient cells. NK cells therefore spared ULBP-deficient cells in vitro. The ULBPs were identified only on GPI-expressing blood cells of a proportion of patients with PNH but none of healthy individuals. Granulocytes of the patients partly underwent killing by autologous cytotoxic cells, implying ULBP-associated blood cell injury. In this setting, the lack of ULBPs may allow immunoselection of PNH clones.
Introduction
Paroxysmal nocturnal hemoglobinuria (PNH) is an acquired stem cell disorder of clonal nature characterized by intravascular hemolysis, venous thrombosis, bone marrow (BM) dysfunction, and infrequent development of leukemia.1-4 In the last 2 decades, virtually the entire mechanism leading to PNH hemolysis has been elucidated.5-8 PNH stem cells acquire PIGA mutations and do not generate glycosylphosphatidylinositol (GPI), resulting in a deficiency of a series of GPI-linked membrane proteins, including complement regulatory molecules such as decay-accelerating factor (DAF) and CD59. PNH cells are then vulnerable to autologous complement. For example, PNH erythrocytes undergo complement-mediated hemolysis. Soon after, the molecular events leading to clinically serious hemolytic precipitation induced by infection were clarified.9 On the other hand, more than half of patients with PNH show various cytopenias and decreased CD34+ hematopoietic cells.1-4,10-12 PNH closely associates with aplastic anemia and myelodysplastic syndromes (MDSs) that share BM failure and development of leukemia.1,12,13 It has been indicated that immune-mediated BM injury underlies at least a part of the diseases.1,12 Indeed, immunosuppressive therapy ameliorates their marrow failure.1,12,14,15 Of interest, combination therapy with antithymocyte globulin and cyclosporine A, these immunosuppressants having individual target spectra,16,17 gives better results than therapy with each 1 of the 2 immunosuppressants.12,18 In general, both cytotoxic T lymphocytes (CTLs) of adaptive immunity and natural killer (NK) cells of innate immunity operate in combination rather than independently.19-22 It is then conceivable that both cytotoxic cells exert critical roles in BM injury,12,23-26 although real features of the autoimmunity have not been delineated.
The marked progress in understanding of PNH pathophysiology evokes the next concern about the etiology of PNH, and the mechanisms of both selective expansion of PNH clones27 and development of leukemia.28 Above all, we have focused on the expansion of affected cells to manifest PNH symptoms. Increasing evidence suggests that the expansion is not simply attributable to PIGA mutations alone.27,29 For example, blood cells with PIGA mutations, despite extremely low population, are present even in healthy individuals.11,30 Moreover, PIGA mutant cells do not expand in the murine Piga knockout models.31-33 Of clinical note, blood cells with PNH phenotype (GPI-deficient or GPI- cells) are frequently detected in patients with BM failure syndromes such as aplastic anemia34,35 and MDS.13 As expected, some of the patients really develop hemolytic PNH.35 The observations suggest that GPI- cells survive immune-mediated BM injury putatively caused by cytotoxic cells such as NK cells and CTLs (so-called immuno-selection).27,36,37 In support, we previously reported that cultured human leukemic K562 cells became relatively resistant to NK cell-mediated cytotoxicity after acquisition of PIGA mutations in vitro.38 In addition, the enzymatic liberation of GPI-linked membrane proteins decreased the sensitivity of human tumor cell lines to NK cells.39 These findings suggested that the NK resistance is attributable to the lack of some GPI-linked membrane protein(s) that activate NK cells. The immunoselection of GPI- cells was also demonstrated using CTLs instead of NK cells in a mouse model from another independent laboratory,40 although there is still controversy.41 Immunoselection is therefore now considered to be essential for the selective expansion of PNH clones.27,29
As for potential candidates for the GPI-linked membrane proteins which activate NK cells, we are reminded of ULBP and CD48.42,43 However, our K562 cells express the former alone. ULBP indicates cytomegalovirus glycoprotein UL16-binding protein, which is classified into 3 molecules, ULBP1, ULBP2, and ULBP3.42 Similar to the major histocompatibility complex (MHC) class I homologs, MHC class I chain-related molecule A (MICA) and MICB,44,45 ULBPs are stress-inducible proteins that appear on the membrane when cells undergo stress such as infection and transformation.42,46 MICA/B are peptide-anchored but not GPI-linked membrane proteins.44 Once the stress-inducible proteins emerge on the cell surface, cytotoxic cells such as NK cells and CTLs catch the molecules using their activating receptor NKG2D and eliminate the cells exposed to stress.42,47,48 Both ULBP and MICA/B share NKG2D as a receptor.42,48 The receptor is present on human NK and T cells (CD8+ T, γδ T, and a part of CD4+ T cells).42,45,48,49 The NK activation signal from the NKG2D ligands overrides the NK inhibition signal mediated by the killer cell immunoglobulin-like receptor (KIR)-MHC class I engagement.42,45 Accordingly, it is conceivable that affected cells missing stress-inducible membrane proteins such as ULBPs and MICA/B preferentially survive in the setting of immune attack by cytotoxic cells expressing NKG2D.
In the present study, we show that the decreased susceptibility to NK cells of K562 cells bearing PIGA mutations is attributable to the absence of ULBP1 and ULBP2 in vitro. Further, PNH clones may survive in vivo in the same manner, judging from the distinctive exposure of the ULBPs on GPI-expressing (GPI+) blood cells alone in a proportion of patients with PNH.
Patients, materials, and methods
Patients
Table 1 shows the clinical profiles and laboratory data of 14 patients with PNH: 7 female and 7 male patients ranging in age from 24 to 81 years. Eight and 6 patients were diagnosed as having de novo PNH and aplastic anemia-PNH syndrome, respectively. PNH was diagnosed on the basis of acquired intravascular hemolysis negative for Coombs test, the detection of complement-sensitive erythrocytes by Ham test, and detection by flow cytometry of blood cells negative for GPI-linked membrane proteins such as DAF and CD59.51,52 The controls consisted of 17 healthy volunteers.
Clinical profiles of patients with PNH
. | . | . | . | . | . | Granulocytes . | . | |
|---|---|---|---|---|---|---|---|---|
| Patient no. . | Sex/age, y . | Diagnosis . | Duration, y* . | Hemoglobin, g/L . | Platelets, × 109/L . | Cell no., × 109/L . | DAF–/CD59–, %† . | |
| 1 | M/24 | PNH | 2 | 88 | 75 | 1.7 | 79 | |
| 2 | M/29 | PNH | 12 | 62 | 232 | 1.3 | 94 | |
| 3 | M/35 | PNH | 15 | 59 | 270 | 0.2 | 90 | |
| 4 | F/56 | PNH | 12 | 92 | 193 | 2.2 | 84 | |
| 5 | M/66 | PNH | 9 | 133 | 191 | 3.6 | 44 | |
| 6‡ | F/71 | PNH | 24 | 101 | 67 | 1.4 | 100 | |
| 7 | M/79 | PNH | 7 | 102 | 124 | 1.9 | 35 | |
| 8 | F/79 | PNH | 7 | 90 | 194 | 1.8 | 72 | |
| 9 | F/24 | AA-PNH | 8 | 69 | 216 | 2.0 | 90 | |
| 10 | F/27 | AA-PNH | 8 | 127 | 76 | 1.5 | 15 | |
| 11 | F/39 | AA-PNH | 1 | 103 | 96 | 1.4 | 1 | |
| 12 | M/64 | AA-PNH | 9 | 116 | 121 | 1.5 | 1 | |
| 13 | F/73 | AA-PNH | 8 | 87 | 37 | 2.1 | 95 | |
| 14 | M/81 | AA-PNH | 10 | 117 | 69 | 2.6 | 1 | |
. | . | . | . | . | . | Granulocytes . | . | |
|---|---|---|---|---|---|---|---|---|
| Patient no. . | Sex/age, y . | Diagnosis . | Duration, y* . | Hemoglobin, g/L . | Platelets, × 109/L . | Cell no., × 109/L . | DAF–/CD59–, %† . | |
| 1 | M/24 | PNH | 2 | 88 | 75 | 1.7 | 79 | |
| 2 | M/29 | PNH | 12 | 62 | 232 | 1.3 | 94 | |
| 3 | M/35 | PNH | 15 | 59 | 270 | 0.2 | 90 | |
| 4 | F/56 | PNH | 12 | 92 | 193 | 2.2 | 84 | |
| 5 | M/66 | PNH | 9 | 133 | 191 | 3.6 | 44 | |
| 6‡ | F/71 | PNH | 24 | 101 | 67 | 1.4 | 100 | |
| 7 | M/79 | PNH | 7 | 102 | 124 | 1.9 | 35 | |
| 8 | F/79 | PNH | 7 | 90 | 194 | 1.8 | 72 | |
| 9 | F/24 | AA-PNH | 8 | 69 | 216 | 2.0 | 90 | |
| 10 | F/27 | AA-PNH | 8 | 127 | 76 | 1.5 | 15 | |
| 11 | F/39 | AA-PNH | 1 | 103 | 96 | 1.4 | 1 | |
| 12 | M/64 | AA-PNH | 9 | 116 | 121 | 1.5 | 1 | |
| 13 | F/73 | AA-PNH | 8 | 87 | 37 | 2.1 | 95 | |
| 14 | M/81 | AA-PNH | 10 | 117 | 69 | 2.6 | 1 | |
AA-PNH indicates aplastic anemia–PNH syndrome.
Years after diagnosis
DAF–/CD59– indicates granulocytes negative for both DAF and CD59
Patient no. 6 was a PNH patient with coexisting congenital deficiency of complement C950
Cell culture
Human leukemic K562 cells bearing a PIGA mutation were transfected with either PIGA cDNA or a mock vector alone without PIGA cDNA, as described previously.38 The former K562 cells recovered the expression of GPI-linked membrane proteins such as DAF and CD59 (GPI+ cells), while the latter still failed to express the membrane proteins (GPI- cells; data not shown). In contrast to wild-type K562 cells that are known to lack MHC class I, both GPI+ and GPI- K562 cells weakly but equally expressed MHC class I.38 The differences between GPI+ and GPI- cells were merely in the PIGA mutation and expression of GPI-linked membrane proteins. The K562 cells were cultured in RPMI 1640 medium as described previously.38 Next, an interleukin (IL)-2-dependent human NK cell line bearing a p53 mutation (KHYG-1; Human Science Research Resources Bank, Osaka, Japan)53 was maintained in the medium with 100 U/mL recombinant IL-2 (Shionogi, Osaka, Japan) and used as cytotoxic effector cells after incubation in the IL-2-depleted medium for 24 hours prior to cytotoxicity assay, as described previously.38
Preparation of blood cells
Granulocytes and peripheral blood mononuclear cells (PBMCs) were prepared with dextran sulfate (Nacalai Tesque, Kyoto, Japan) and Ficoll-Hypaque (Amersham, Piscataway, NJ) by the methods described elsewhere.54 The purity of a granulocyte fraction exceeded 98% when determined by May-Giemsa staining. BM mononuclear cells were obtained from 3 patients with PNH and 3 healthy controls by Ficoll-Hypaque gradient centrifugation.54 All samples from patients with PNH and healthy donors were obtained after informed consent was provided according to the Declaration of Helsinki. These studies were approved by the Institutional Review Board of Kumamoto University.
Antibodies
Mouse monoclonal antibodies (mAbs) to ULBP1 (170818, IgG2a), ULBP2 (165903, IgG2a), ULBP3 (166510, IgG2a), and NKG2D (149810, IgG1) were purchased from Genezyme Techne (Minneapolis, MN). mAbs to CD48 (Tu145, IgM) and CD16 (3G8, IgG1) and phycoerythrin (PE)-conjugated mAb to CD56 (B159, IgG1) were from Pharmingen (San Jose, CA). mAb to MICA (AMO1, IgG1) was from Immatics Biotechnologies (Firenze, Italy). PE-conjugated mAbs to CD34 (IOM34, IgG1), DAF (67, IgG1), and CD8 (T8, IgG1) were from Immunotech (Marseille, France), Caltag Laboratories (Burlingame, CA), and Beckman Coulter (Miami, FL), respectively. mAbs to MHC class I (W6/32, IgG2a) and fluorescein isothiocyanate (FITC)-conjugated mAb to CD59 (5H8, IgG1)9 were a gift from M. Takiguchi (Kumamoto University) and M. Tomita (Showa University), respectively. FITC-conjugated mAb to CD3 (UCHT1, IgG1) was from Beckman Coulter. Goat polyclonal antibodies (pAbs) to ULBP1, ULBP3, MICA/B, and NKG2D were purchased from Santa Cruz Biotechnology (Santa Cruz, CA) and pAb to ULBP2 was from Genezyme Techne. FITC-conjugated goat antibodies to mouse Ig (IgG or IgM), PE-conjugated goat antibodies to mouse IgG, and PE-conjugated rabbit antibodies to goat IgG were purchased from Zymed Laboratories (San Francisco, CA), Chemicon (Temecula, CA), and Sigma-Aldrich (St. Louis, MO), respectively. Mouse IgG1, IgG2a, IgM (Beckman Coulter), and goat IgG (Chemicon) were used as isotype-matched control immunoglobulins.
Flow cytometry
Cell surface was analyzed by flow cytometry as described previously.10,35 In brief, GPI+ and GPI- K562 cells were incubated with antibodies to ligands for NK cells (ULBPs 1-3, MICA, MICA/B, MHC class I, and CD48) and labeled with PE- or FITC-conjugated second antibodies. Cultured NK cells (KHYG-1) were incubated with mAbs to either NKG2D or CD16, and labeled with FITC-conjugated second antibodies. Cells were then analyzed with a flow cytometer (EPICS; Beckman Coulter, Fullerton, CA). Two-color flow cytometry was used to determine the expression of both ULBPs and MICA on granulocytes positive or negative for CD59. Granulocytes were incubated with mAbs to either ULBPs 1-3, MICA, or isotype-matched control Ig, labeled with PE-conjugated goat anti-mouse IgG, and then with FITC-conjugated mAb to CD59. BM cells were also analyzed by 2-color flow cytometry after labeling with mAbs to ULBPs 1-3, FITC-conjugated goat anti-mouse IgG, and then PE-conjugated mAb to CD34. Surface expression of NKG2D on lymphocytes was analyzed by 2-color flow cytometry after labeling with mAb to NKG2D, FITC-conjugated goat anti-mouse IgG, and then PE-conjugated mAb to CD56 or CD8. The number of NK (CD3-/CD56+) cells in PBMCs was determined by 2-color flow cytometry using both FITC-conjugated mAb to CD3 and PE-conjugated mAb to CD56.
Cytotoxicity assay
NK cell activity was determined by 51Cr-release assay as described previously.38 In brief, target cells (5 × 105 /mL K562 cells, or 1 × 106 /mL granulocytes) were preincubated with 3.7 MBq (0.1 mCi) Na251CrO4 (Perkin Elmer, Boston, MA) for 3 hours at 37°C. After dilution, cells (5 × 103/100 μL of K562 cells per well, or 1 × 104/100 μL of granulocytes per well) were mixed with NK cells at various ratios of effector and target cells (E/T ratio) in a 96-well round-bottom microtiter plate (Corning, New York, NY) in triplicate. After the plate was centrifuged at 50g for 2 minutes, K562 cells and granulocytes were incubated, respectively, for 2 and 4 hours at 37°C, 5% CO2 in the culture medium containing 10 mM N-2-hydroxyethylpiperazine-N′-2-ethanesulfonic acid (HEPES; Sigma-Aldrich) at pH 7.2. Radioactivity of 51Cr released to the medium from target cells was determined with an automated γ-counter (Minaxi 5530; Packard Instrument, Downers Grove, IL). Percentage cytotoxicity was calculated using the following formula: % specific cytotoxicity = (experimental release - spontaneous release)/(maximum release - spontaneous release) × 100. Spontaneous release was less than 10% of maximum release.
Inhibition assays with antibodies
Cultured NK cells (KHYG-1 cell line) lack CD16 (receptor for Fcγ)53 and do not exert antibody-dependent cellular cytotoxicity (ADCC). Cytotoxicity by KHYG-1 cells was assessed after target K562 cells were preincubated with or without various concentrations of antibodies to NKG2D ligands (ULBPs 1-3, MICA, and MICB) for 1 hour at 37°C. E/T ratio was 16:1. In another experiment, KHYG-1 cells were pretreated with 100 μg/mL of pAb to NKG2D receptor and used for cytotoxicity assay under the same conditions as described.
Reverse transcription-polymerase chain reaction (RT-PCR) analysis
Total RNA was isolated from cells with TRIzol Reagent (Invitrogen, Carlsbad, CA) and converted to cDNA with oligo dT primer using a kit (ReverTra; Toyobo, Osaka, Japan) according to the manufacturer's instructions.55 A fragment of 322-328 bp encompassing a part of α2 domain and GPI anchor signal sequence of ULBPs 1-3 transcripts42 was amplified by PCR with 0.5 U recombinant Taq DNA polymerase (ExTaq; Takara, Shiga, Japan), 200 μM dNTPs in a buffer (25 μL; 10 mM Tris-HCl, pH 8.3, 50 mM KCl, 1.5 mM MgCl2, 0.001% gelatin), and 10 pmol of primers (forward, 5′-CTGCAGGYMAGGATGTCTTGTGAG-3′; reverse, 5′-TGAGGGTGGTGGCYRTGGC-3′).42 After initial denaturation at 95°C for 1 minute, DNA amplification was performed with a PCR thermocycler (Astec, Fukuoka, Japan) for 35 cycles; each cycle consisted of denaturation at 95°C for 30 seconds, annealing at 65°C for 30 seconds, and extension at 72°C for 45 seconds with a final extension at 72°C for 3 minutes. A housekeeping gene, glyceraldehyde 3-phosphate dehydrogenase (G3PDH), was used as a control to determine equal loading of RNA. Each transcript of ULBPs 1-3 was identified by its sensitivity to restriction enzymes.42 Briefly, RT-PCR products were digested with BamHI and BglII (Toyobo), restriction enzymes specific for ULBP1 and ULBP2 transcripts, respectively, and then were analyzed by 2% agarose gel electrophoresis and ethidium bromide staining. In further experiments, a full-length cDNA (741 bp) of ULBP2, as representative of 3 ULBPs of granulocytes, was analyzed by semiquantitative RT-PCR using specific primers (forward, 5′-CGGAATTCATGGCAGCAGCCGCCGCTACCAA-3′; reverse, 5′-CGCTCGAGTCAGATGCCAGGGAGGATGAAGCAGG-3′).
Statistical analysis
Student unpaired t test or analysis of variance (ANOVA) followed by Fisher protected least significant difference test was used to determine significance levels when comparing 2 groups or more than 2 groups, respectively. For multiple comparisons of data from patients' samples, Kruskal-Wallis nonparametric test was used. P values less than .05 were considered significant.
Results
Limited expression of ULBP on the membrane of GPI+ K562 cells
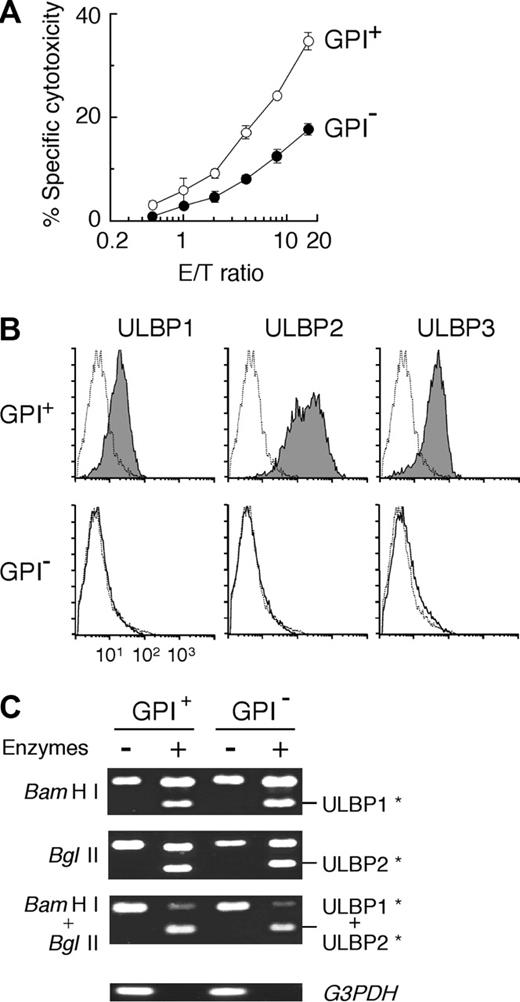
Our previous findings that leukemic cells bearing PIGA mutations were less susceptible to NK cells than control cells without the mutations are reproducible as shown in Figure 1A.38
We have proposed that the decreased NK susceptibility of GPI- cells is attributable to the absence of some GPI-linked membrane protein(s) that activate NK cells. In our search, ULBP and CD48 were the candidates for the GPI proteins.42,43 Flow cytometry showed that none of our K562 cells expressed CD48 (data not shown). In contrast, ULBPs 1-3 were differentially expressed on GPI+ cells but on none of GPI- cells (Figure 1B). ULBP2 expression was the most obvious (Figure 1B). RT-PCR products of ULBP transcripts with expected size of 322 to 328 bp were almost equally generated from both GPI+ and GPI- cells (Figure 1C, top and middle panels). ULBP1 and ULBP2 transcripts were separated by the digestion of their RT-PCR products with BamHI and BglII restriction enzymes, respectively. The ULBP3 transcript was confirmed by its resistance to the enzymes (Figure 1C, bottom panel). As a result, only the membrane expression of ULBPs distinguishes GPI+ from GPI- K562 cells.
Selective expression of ULBP on the membrane of GPI+ K562 cells. (A) GPI- K562 cells (•) were less susceptible to NK cells than GPI+ K562 cells (○). Each value represents the mean (± SD) of triplicate assays. (B) Flow cytometry showed the membrane expression of ULBPs 1-3 in GPI+ cells alone (shaded histograms). Dotted lines show nonspecific background staining with isotype-matched control Ig. (C) RT-PCR products showed similar expression of ULBPs 1-3 in GPI+ and GPI- cells. RT-PCR products of ULBP1 and ULBP2 were digested with BamHI and BglII restriction enzymes, respectively. RT-PCR products of ULBP3-transcript were resistant to both enzymes. G3PDH indicates glyceraldehyde 3-phosphate dehydrogenase. *Digested fragments of RT-PCR products of each ULBP.
Selective expression of ULBP on the membrane of GPI+ K562 cells. (A) GPI- K562 cells (•) were less susceptible to NK cells than GPI+ K562 cells (○). Each value represents the mean (± SD) of triplicate assays. (B) Flow cytometry showed the membrane expression of ULBPs 1-3 in GPI+ cells alone (shaded histograms). Dotted lines show nonspecific background staining with isotype-matched control Ig. (C) RT-PCR products showed similar expression of ULBPs 1-3 in GPI+ and GPI- cells. RT-PCR products of ULBP1 and ULBP2 were digested with BamHI and BglII restriction enzymes, respectively. RT-PCR products of ULBP3-transcript were resistant to both enzymes. G3PDH indicates glyceraldehyde 3-phosphate dehydrogenase. *Digested fragments of RT-PCR products of each ULBP.
Decreased NK cell sensitivity of GPI- K562 cells ascribable to lack of ULBPs 1 and 2
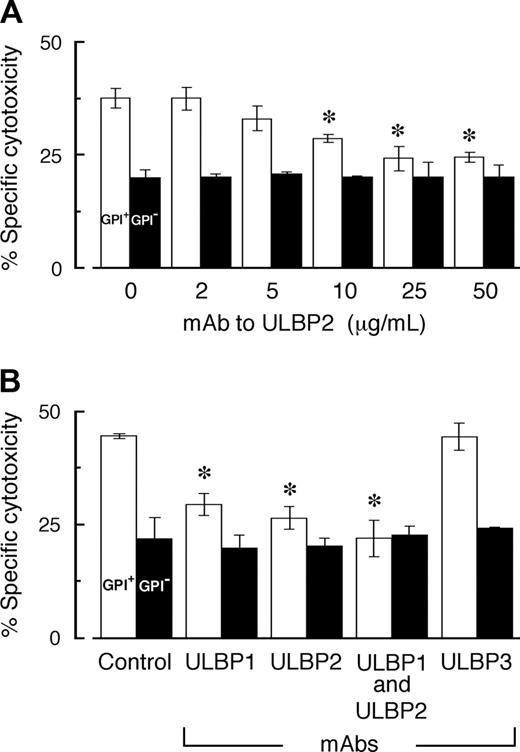
We assessed the role of ULBP molecules on the membrane of GPI+ K562 cells in the cytotoxicity exerted by NK cells, using mAbs to ULBPs. Antibodies to ULBP1 or ULBP2 dose-dependently inhibited NK cell-mediated killing of GPI+ K562 cells, while none of the mAbs exerted any effects on the killing of GPI- cells (data partly shown in Figure 2A-B).
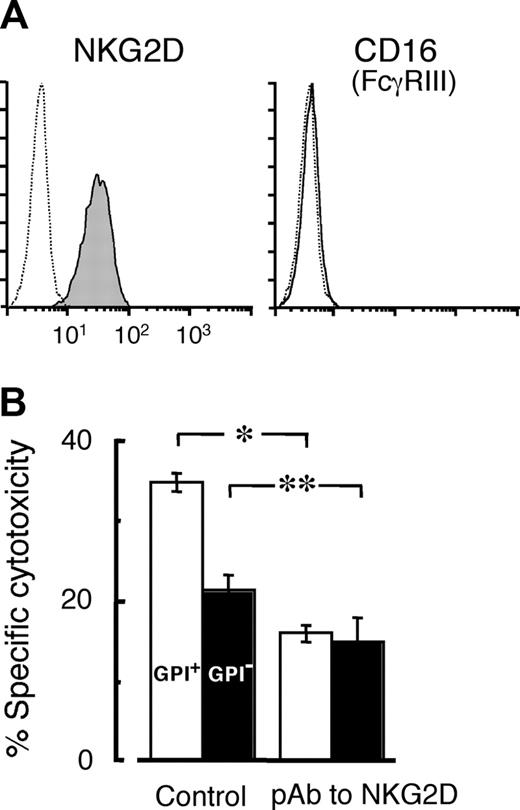
Maximum inhibition was achieved with 25 μg/mL of each mAb. Of note, mAbs to both ULBP1 and ULBP2, in combination but not separately, virtually abolished the difference in the NK cell sensitivity between GPI+ and GPI- cells (Figure 2B). None of the antibodies to ULBP3 exerted any effect in the cytotoxicity assay (Figure 2B). ULBP3 is then functionally distinctive. Polyclonal antibodies to the ULBPs showed consistent results with those using the mAbs (data not shown). These findings suggest that ULBP1 and ULBP2 are molecules responsible for the decreased sensitivity to NK cells of GPI- K562 cells. To support this conclusion, we next attempted to inhibit the NK activation signal from NKG2D-ULBP engagement, using antibodies to NKG2D on NK cells instead of antibodies to ULBPs on target cells. Cultured NK cells, KHYG-1, expressed NKG2D but were negative for CD16 (Figure 3A), indicating that CD16-mediated ADCC could be excluded in the assays with antibodies.
Inhibition of NK cell-mediated killing with mAbs to ULBP on K562 cells. (A) Monoclonal antibody to ULBP2 dose-dependently inhibited the killing of GPI+ K562 cells alone. (B) Killing of GPI+ cells was inhibited with 25 μg/mL mAbs to ULBPs 1 and 2 but none of mAb to ULBP3. The mixture of mAbs to ULBPs 1 and 2 completely abolished the difference in the killing between GPI+ and GPI- cells. Each value represents the mean (± SD) of triplicate assays (E/T ratio, 16:1). □ indicates GPI+ K562 cells; ▪, GPI- K562 cells; and Control, isotype-matched control Ig. *P < .01 compared with antibody-free group.
Inhibition of NK cell-mediated killing with mAbs to ULBP on K562 cells. (A) Monoclonal antibody to ULBP2 dose-dependently inhibited the killing of GPI+ K562 cells alone. (B) Killing of GPI+ cells was inhibited with 25 μg/mL mAbs to ULBPs 1 and 2 but none of mAb to ULBP3. The mixture of mAbs to ULBPs 1 and 2 completely abolished the difference in the killing between GPI+ and GPI- cells. Each value represents the mean (± SD) of triplicate assays (E/T ratio, 16:1). □ indicates GPI+ K562 cells; ▪, GPI- K562 cells; and Control, isotype-matched control Ig. *P < .01 compared with antibody-free group.
Inhibition of NK cell-mediated killing with pAb to NKG2D on NK cells. (A) A NK cell line (KHYG-1) expressed NKG2D, a receptor for ULBPs (shaded histogram). The cells were negative for CD16, which is needed for ADCC. Dotted lines show nonspecific background staining with isotype-matched control Ig. (B) Antibodies to NKG2D (100 μg/mL) inhibited the killing and virtually abolished the difference in the killing of GPI+ (□) and GPI- (▪) K562 cells. Each value represents the mean (± SD) of triplicate assays (E/T ratio, 16:1). Control indicates isotype-matched control Ig. *P < .01; **P < .05.
Inhibition of NK cell-mediated killing with pAb to NKG2D on NK cells. (A) A NK cell line (KHYG-1) expressed NKG2D, a receptor for ULBPs (shaded histogram). The cells were negative for CD16, which is needed for ADCC. Dotted lines show nonspecific background staining with isotype-matched control Ig. (B) Antibodies to NKG2D (100 μg/mL) inhibited the killing and virtually abolished the difference in the killing of GPI+ (□) and GPI- (▪) K562 cells. Each value represents the mean (± SD) of triplicate assays (E/T ratio, 16:1). Control indicates isotype-matched control Ig. *P < .01; **P < .05.
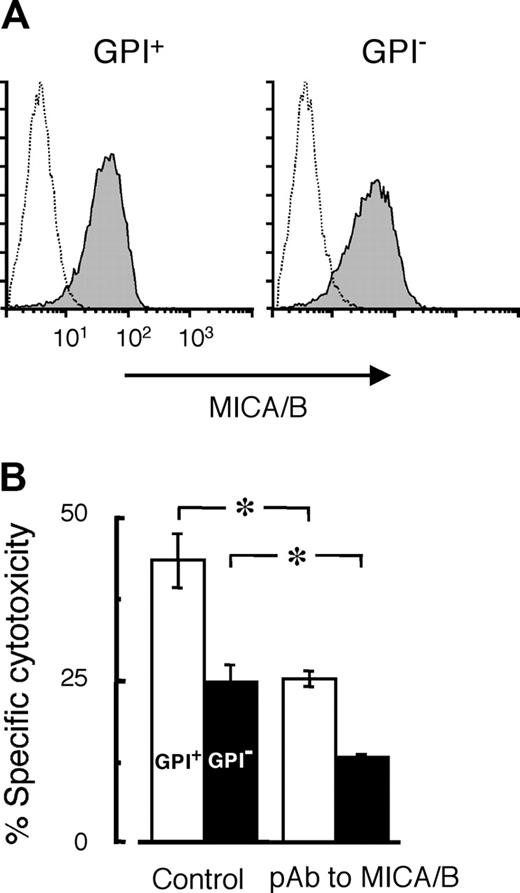
Pretreatment with pAb to NKG2D of KHYG-1 (NK) cells diminished the cytotoxicity and virtually abolished the difference in the killing of GPI+ and GPI- K562 cells (Figure 3B). Furthermore, we used pAbs to MICA and MICB that share a NKG2D receptor with ULBPs in order to clarify the involvement of NKG2D-MICA/B engagement in the cytotoxicity. Both GPI+ and GPI- cells similarly expressed MICA and MICB that are not GPI-linked proteins (Figure 4A).
As expected, the antibodies significantly inhibited the cytotoxicity but did not alter the difference in the killing between GPI+ and GPI- cells (Figure 4B). The decreased sensitivity to NK cells of GPI- K562 cells is thus attributable to the absence of both ULBP1 and ULBP2 in vitro.
Display of ULBP on the membrane of blood cells of patients with PNH
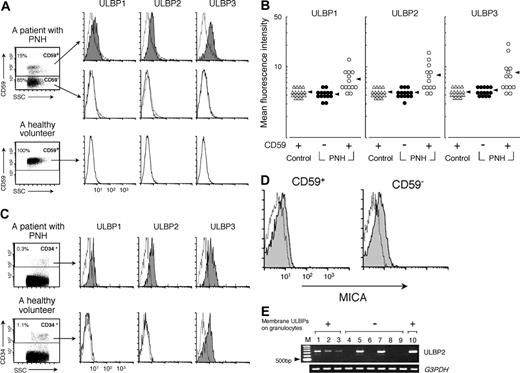
Our next concern is whether the immune escape scenario for GPI- K562 cells is applicable for PNH clones to selectively expand in patients with PNH. To collect evidence to support this scenario, we analyzed cell-surface expression of ULBPs in blood cells of patients with PNH. ULBPs appeared in the circulating GPI+ granulocytes of 7 of 14 patients with PNH (Figure 5A-B), although their expression was less than that of GPI+ K562 cells (Figure 1B).
The weak expression of ULBPs in freshly isolated human cells is often noted.56 ULBPs were variably expressed: ULBPs 1-3 in patient nos. 1, 2, 3, 4, and 13; and ULBPs 2 and 3 in patient nos. 9 and 14, listed in Table 1. In patient no. 6, GPI+ granulocytes were not detectable. In patient nos. 5, 7, 8, 10, 11, and 12, none of the GPI+ granulocytes expressed ULBPs. As expected, neither the GPI- granulocytes of patients nor the control granulocytes of 17 healthy volunteers expressed ULBPs (Figure 5A-B). On the other hand, a sufficient number of CD34+ cells for the analysis were collected from 2 (patient nos. 10 and 13 in Table 1) of 3 patients with PNH who donated their BM cells. More than 11% of CD34+ BM cells were positive for CD59 in these patients. On the CD34+ cells, ULBPs 1-3 were detected visibly (Figure 5C), indicating the expression of ULBPs on hematopoietic stem cells. CD34+ cells of healthy donors were all positive for CD59 but negative for ULBPs 1 and 2 (Figure 5C). To our surprise, ULBP3 was evidently detected on CD34+ cells of the healthy donors (Figure 5C), although there is a report of ULBP3 transcripts in normal CD34+ BM cells.57 To confirm the presence of stress to induce membrane ULBPs, we attempted to detect another stress-inducible protein, MICA, which is not GPI linked. MICA appeared equally on both CD59+ and CD59- granulocytes of PNH patients who had cells expressing membrane ULBPs (Figure 5D), indicating that the patients were exposed to some stress to induce ULBPs and MICA. In terms of MICA expression, CD59- cells perceived and responded to the stress as well as CD59+ cells.
Inhibition of NK cell-mediated killing with pAb to MICA/B on K562 cells. (A) MICA/B, peptide-anchored membrane proteins, were expressed in both GPI+ and GPI- K562 cells (shaded histograms). Dotted lines show nonspecific background staining with isotype-matched control Ig. (B) Polyclonal antibodies to MICA/B (100 μg/mL) inhibited the killing of both GPI+ (□) and GPI- (▪) cells but did not abolish the difference in their killing. Each value represents the mean (± SD) of triplicate assays (E/T ratio, 16:1). Control indicates isotype-matched control Ig. *P < .01.
Inhibition of NK cell-mediated killing with pAb to MICA/B on K562 cells. (A) MICA/B, peptide-anchored membrane proteins, were expressed in both GPI+ and GPI- K562 cells (shaded histograms). Dotted lines show nonspecific background staining with isotype-matched control Ig. (B) Polyclonal antibodies to MICA/B (100 μg/mL) inhibited the killing of both GPI+ (□) and GPI- (▪) cells but did not abolish the difference in their killing. Each value represents the mean (± SD) of triplicate assays (E/T ratio, 16:1). Control indicates isotype-matched control Ig. *P < .01.
Increased gene expression of ULBP in granulocytes of patients with PNH
To support the appearance of ULBPs on membrane of blood cells of patients with PNH, we analyzed mRNA expression of ULBP2, as representative of 3 ULBPs, in granulocytes of patients with PNH by semiquantitative RT-PCR (Figure 5E). ULBP2 mRNA was up-regulated in patients with PNH who had granulocytes expressing membrane ULBPs (lanes 1-3) but in none of healthy donors (lanes 8 and 9). In patients with PNH whose granulocytes lacked membrane ULBPs (lanes 4-7), ULBP2 was up-regulated in 2 (lanes 5 and 7) but not detectable in other patients (lanes 4 and 6). Proportions of PNH granulocytes in lanes 4 to 7 were 35%, 15%, 1%, and 100%, respectively. Both lack of membrane ULBPs and up-regulation of ULBP2 mRNA in lanes 5 and 7 may be explained by inhibition of their display on the membrane (so-called masking)58 and the absence of GPI+ granulocytes (patient no. 6 in Table 1), respectively. Further, up-regulation of mRNA of stress-inducible ULBP2 in patient no. 6 who had granulocytes with PNH phenotype alone (lane 7) suggests that PNH cells responded to stress to induce, at least, ULBP2. The stress response of PNH cells is also supported by the MICA expression (Figure 5D). Patients in lanes 4 and 6 expressed neither membrane ULBPs nor ULBP2 mRNA. In these patients, it is conceivable that ULBP-inducible stress has disappeared. Induction of both ULBPs and MICA shown by either flow cytometry (Figure 5A-D) or RT-PCR analysis (Figure 5E) suggests that the patients were exposed to some pressure to induce the expression of the stress proteins.
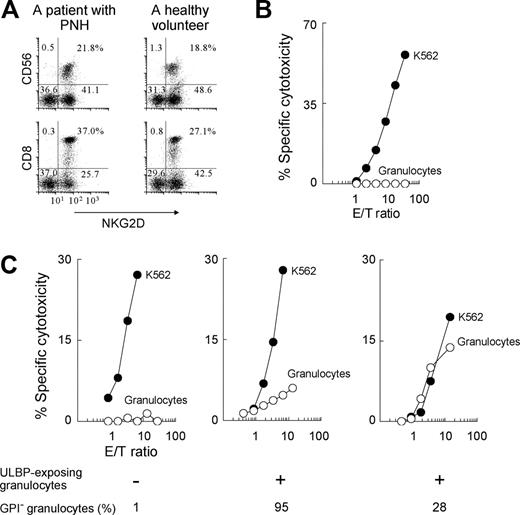
Killing of granulocytes by autologous cytotoxic cells of patients with PNH having cells displaying membrane ULBP
To evaluate the pathophysiologic roles of the membrane expression of ULBPs in blood cells of patients with PNH, we attempted to kill ULBP-expressing granulocytes with autologous cytotoxic cells, including NK and T cells, that express NKG2D (Figure 6). Assay with autologous NK cells has been described.59,60 Although maximum E/T ratio was at most 27 because of a limited amount of cytotoxic effector cells isolated from patients with PNH, granulocytes of patients with PNH who had cells expressing membrane ULBPs were partly killed (middle and right panels in Figure 6C). Only the patients having ULBP+ granulocytes (middle and right panels in Figure 6C) also had MICA+ granulocytes.
Expression of ULBP on the blood cells of patients with PNH. (A) Flow cytometry revealed the expression of ULBPs 1-3 on GPI+ granulocytes (shaded histograms) of a patient with PNH (patient no. 1 in Table 1) but on neither his GPI- granulocytes nor control granulocytes of a healthy volunteer. (B) Expression profiles of ULBPs were summarized in 14 PNH patients (PNH: ○, CD59+; •, CD59-) and 17 healthy volunteers (Control, ▵). Arrows indicate the average of mean fluorescence intensities in each population. (C) ULBPs 1-3 were expressed on CD34+ BM cells (shaded histograms) of a patient with PNH (patient no. 10 in Table 1). 87% of the cells were positive for CD59. Only ULBP3 was detected on the BM cells of a healthy volunteer. Dotted lines show nonspecific background staining with isotype-matched control Ig. (D) Expression of MICA on CD59+ and CD59- granulocytes (shaded histograms) of a patient with PNH (patient no. 9 in Table 1) who had granulocytes expressing membrane ULBPs. (E) Expression of ULBP2 mRNA in granulocytes of 7 patients with PNH (lanes 1-7) and 2 healthy donors (lanes 8 and 9). Lanes 1-3 show patients with PNH having granulocytes expressing membrane ULBPs; lanes 4-7, PNH patients having granulocytes lacking membrane ULBPs. M indicates 100-bp DNA ladder; lanes 1-7, patient nos. 2, 3, 4, 7, 10, 12, or 6 in Table 1; lane 10, K562 cells; and G3PDH, glyceraldehyde 3-phosphate dehydrogenase. Dotted lines in panels A, C, and D indicate nonspecific background staining with isotype-matched control Ig.
Expression of ULBP on the blood cells of patients with PNH. (A) Flow cytometry revealed the expression of ULBPs 1-3 on GPI+ granulocytes (shaded histograms) of a patient with PNH (patient no. 1 in Table 1) but on neither his GPI- granulocytes nor control granulocytes of a healthy volunteer. (B) Expression profiles of ULBPs were summarized in 14 PNH patients (PNH: ○, CD59+; •, CD59-) and 17 healthy volunteers (Control, ▵). Arrows indicate the average of mean fluorescence intensities in each population. (C) ULBPs 1-3 were expressed on CD34+ BM cells (shaded histograms) of a patient with PNH (patient no. 10 in Table 1). 87% of the cells were positive for CD59. Only ULBP3 was detected on the BM cells of a healthy volunteer. Dotted lines show nonspecific background staining with isotype-matched control Ig. (D) Expression of MICA on CD59+ and CD59- granulocytes (shaded histograms) of a patient with PNH (patient no. 9 in Table 1) who had granulocytes expressing membrane ULBPs. (E) Expression of ULBP2 mRNA in granulocytes of 7 patients with PNH (lanes 1-7) and 2 healthy donors (lanes 8 and 9). Lanes 1-3 show patients with PNH having granulocytes expressing membrane ULBPs; lanes 4-7, PNH patients having granulocytes lacking membrane ULBPs. M indicates 100-bp DNA ladder; lanes 1-7, patient nos. 2, 3, 4, 7, 10, 12, or 6 in Table 1; lane 10, K562 cells; and G3PDH, glyceraldehyde 3-phosphate dehydrogenase. Dotted lines in panels A, C, and D indicate nonspecific background staining with isotype-matched control Ig.
The granulocytes showed ordinary expression of MHC class I (data not shown), indicating that the killing overrode the inhibition by MHC class I.42,45 In contrast, granulocytes lacking the stress-inducible membrane proteins of either PNH patients (left panel in Figure 6C) or healthy donors (Figure 6B) were not killed. Thus, the findings suggest that the membrane ULBPs and MICA, despite their low level of expression, are functionally active, consistent with previous reports.56
Among the granulocytes shown in Figure 6C, there were differences in both their killing and population of GPI- cells. Considering that MICA is not GPI linked, the difference in the killing may be partly explained by the expression of ULBPs which are GPI linked. It is possible that ULBPs play a role in the killing.
Discussion
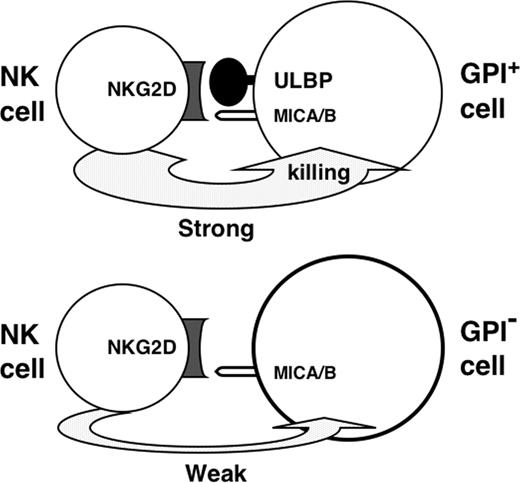
We previously reported that human leukemic K562 cells were less sensitive to NK cell-mediated cytotoxicity in vitro when the leukemic cells acquired PIGA mutations.38 In the present study, we found that the decreased sensitivity to NK cells of the mutant K562 cells was attributable to a deficiency of both ULBPs 1 and 2, which are known to be GPI-linked molecules, to bind to NKG2D on such cytotoxic cells as NK and T cells, and to activate these cells.42 In other words, the absence of the ULBPs resulted in an impaired NK activation (Figure 7).
The PNH clone is representative of PIGA mutant cells deficient in a series of GPI-linked membrane proteins. Therefore, it is conceivable that PNH clones are also capable of preferentially surviving in ULBP-associated injury exerted by cytotoxic cells expressing NKG2D when PNH clones lack ULBPs. As expected, flow cytometry detected ULBPs on none of the CD59- granulocytes of all 14 patients with PNH, indicating that PNH clones lack membrane ULBPs. None of the normal granulocytes of 17 healthy volunteers expressed any ULBPs on their membranes. Interestingly, some molecules of ULBPs 1-3 were expressed on the membrane of both CD59+ granulocytes of 7 of 14 patients and CD34+ BM cells of 2 patients with PNH. These findings indicate that there was pressure to induce ULBPs on the blood cells of these patients. In support, ULBP2 mRNA was up-regulated in patients with PNH who had granulocytes expressing membrane ULBPs (ULBP+). Further, MICA of another stress-inducible protein, which binds to NKG2D and activates NK cells,45 was also detected in the patients. Of note, granulocytes of patients with PNH carrying ULBP+ cells were susceptible to killing by autologous cytotoxic cells, including NK and T cells that expressed NKG2D. Our results prompt us to speculate that the ULBP-NKG2D engagement is implicated in the pathogenesis of BM failure at least in a proportion of patients with PNH. In this setting, lack of membrane ULBPs confers PNH clones a relative survival advantage, allowing their selective expansion.
Killing of granulocytes by autologous cytotoxic cells of patients with PNH. (A) 2-color flow cytometry showed that both CD56+ and CD8+ cells expressed NKG2D in a representative patient with PNH (patient no. 1 in Table 1) and a healthy volunteer. Dotted lines show nonspecific background staining with isotype-matched control Ig. The percentages of cells in each quadrant are indicated. (B-C) Killing of granulocytes (○) and K562 cells (•) was assessed by 4-hour cytotoxicity assay with autologous PBMCs. (B) Representative of 4 healthy donors. (C) Left panel, representative of 3 PNH patients not having granulocytes with membrane ULBPs; middle and right panels, representatives of 5 patients with PNH having granulocytes with membrane ULBPs. Only the patients with ULBP+ cells also had MICA+ cells, whereas the patients without ULBP+ cells did not. E/T ratio indicates NK cells in PBMCs-target cells (K562 cells or isolated granulocytes).
Killing of granulocytes by autologous cytotoxic cells of patients with PNH. (A) 2-color flow cytometry showed that both CD56+ and CD8+ cells expressed NKG2D in a representative patient with PNH (patient no. 1 in Table 1) and a healthy volunteer. Dotted lines show nonspecific background staining with isotype-matched control Ig. The percentages of cells in each quadrant are indicated. (B-C) Killing of granulocytes (○) and K562 cells (•) was assessed by 4-hour cytotoxicity assay with autologous PBMCs. (B) Representative of 4 healthy donors. (C) Left panel, representative of 3 PNH patients not having granulocytes with membrane ULBPs; middle and right panels, representatives of 5 patients with PNH having granulocytes with membrane ULBPs. Only the patients with ULBP+ cells also had MICA+ cells, whereas the patients without ULBP+ cells did not. E/T ratio indicates NK cells in PBMCs-target cells (K562 cells or isolated granulocytes).
For the 6 PNH patients whose CD59+ granulocytes did not express any membrane ULBPs, we raise several possibilities: the pressure to induce ULBPs disappeared; cells expressing ULBPs were preferentially excluded by cytotoxic cells; and membrane exposure of ULBPs was inhibited by binding with some molecules such as CMV-UL16 glycoprotein.58 To draw a conclusion, a large scale and time-course analysis of blood cells of patients with PNH is needed. With regard to the discrete features of ULBP3,61 our inhibition assays with antibodies indicate that ULBP3 was not engaged in the killing of K562 cells in contrast with ULBPs 1 and 2. The findings appear inconsistent with the report that ULBP3 binds to NKG2D and activates NK cells as well as other ULBPs.42,47 As another feature, only ULBP3 was exclusively expressed on the membrane of CD34+ BM cells of healthy donors. In addition, ULBP3 has been reported to not bind to CMV-UL16 in contrast to other ULBPs.42 To depict the role of outstanding behaviors of ULBP3, the mechanism to control the expression of ULBP3 remains to be clarified. In general, the appearance of ULBPs on the membrane of cells under stress triggers a signal of cytotoxicity by NKG2D-expressing cells. Therefore, analyses of both the stress and ULBP expression would be of great help to understand the etiology and pathophysiology of lymphocyte-associated cytotoxicity in aplastic anemia,12,62 rheumatic diseases,63 viral hepatitis,64 and cancers.65,66 Indeed, our preliminary study showed appearance of ULBPs on granulocytes of patients with aplastic anemia and myelodysplastic syndromes (data not shown). Provided that an impaired ULBP-NKG2D engagement allows PNH clones to survive, leading to overt PNH as a human disease, it is feasible to develop a potent remedy by controlling of ULBP-NKG2D interaction for the lymphocyte-associated cytotoxicity.
Lack of ULBP leading to an impaired NK activation under pressure to express stress-inducible membrane proteins.
Lack of ULBP leading to an impaired NK activation under pressure to express stress-inducible membrane proteins.
Prepublished online as Blood First Edition Paper, September 29, 2005; DOI 10.1182/blood-2005-03-1337.
Supported partly by grants from the Wakayama Foundation for the Promotion of Medicine and the Ministry of Education, Culture, Sports, Science, and Technology of Japan.
N.H. and T.K. contributed equally to this work.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 U.S.C. section 1734.
We thank Dr S. Ishihara of Kumamoto University for advice and help.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal