Abstract
Arsenic trioxide, as a single agent, has proven efficacy in inducing molecular remission in patients with acute promyelocytic leukemia (APL). There is limited long-term outcome data with single-agent As2O3 in the management of newly diagnosed cases of APL. Between January 1998 to December 2004, 72 newly diagnosed cases of APL were treated with a regimen of single-agent As2O3 at our center. Complete hematologic remission was achieved in 86.1%. At a median follow-up of 25 months (range: 8-92 months), the 3-year Kaplan-Meier estimate of EFS, DFS, and OS was 74.87% ± 5.6%, 87.21% ± 4.93%, and 86.11% ± 4.08%, respectively. Patients presenting with a white blood cell (WBC) count lower than 5 × 109/L and a platelet count higher than 20 × 109/L at diagnosis (n = 22 [30.6%]) have an excellent prognosis with this regimen (EFS, OS, and DFS of 100%). The toxicity profile, in the majority, was mild and reversible. After remission induction, this regimen was administered on an outpatient basis. Single-agent As2O3, as used in this series, in the management of newly diagnosed cases of APL, is associated with responses comparable with conventional chemotherapy regimens. Additionally, this regimen has minimal toxicity and can be administered on an outpatient basis after remission induction.
Introduction
Acute promyelocytic leukemia (APL) is a subtype of acute myeloid leukemia (AML) characterized by unique clinical and laboratory features at presentation1 as well as a distinct morphology of the blasts2 and a specific cytogenetic abnormality.3 In the majority of cases, the cytogenetic abnormality is t(15;17). This results in a reciprocal translocation between the PML gene on chromosome 15 and the retinoic acid receptor α (RARα) gene on chromosome 17.4 Following the introduction of all-trans retinoic acid (ATRA) in the management of APL, there has been a significant reduction in early treatment-related mortality.5 The combination of ATRA and chemotherapy in induction has led to a dramatic improvement in event-free survival (EFS) and overall survival (OS).6 With currently used ATRA combined with chemotherapy regimens, 70% to 80% of patients are alive and free of disease at 5 years.7 However, as with most chemotherapy schedules, there is associated mortality in a minority and significant morbidity in the majority of patients on these regimens. It has been noted that patients with newly diagnosed APL can potentially be cured without chemotherapy or with minimal use of chemotherapy and thus avoid its complications.8,9 Arsenic trioxide (As2O3), in a dose-dependent manner, can induce differentiation and cause apoptosis of promyelocytes in APL.10 Arsenic trioxide, as a single agent, is effective in inducing remission in patients with relapsed APL.11,12 It has been shown to be equally effective in inducing remission in newly diagnosed cases of APL.13,14 At the doses used to induce remission in APL, As2O3 is not associated with toxicities commonly seen with chemotherapy. In published studies of both relapsed and newly diagnosed cases of APL treated with single-agent As2O3 for remission induction, the postremission therapy has varied. This makes it difficult to assess the impact of this drug on long-term outcome as well as to compare the outcome with established ATRA plus chemotherapy regimens.15
We report here our experience with a regimen of single-agent As2O3 used for remission induction, consolidation, and maintenance in the management of 72 newly diagnosed cases of promyelocytic leukemia/retinoic acid receptor α–positive (PML/RARα+) APL.
Patients, materials, and methods
A trial using As2O3 as a single agent in newly diagnosed cases of APL was initiated in January 1998 at our institution. This was an open, nonrandomized single-center study. The study was reviewed and approved by the institution's research and ethics committee. The first 14 patients were enrolled on this trial. Subsequently, from January 2001, this single-agent As2O3 regimen was offered as a standard alternative regimen to all patients who could not afford conventional ATRA-based chemotherapy regimens due to financial constraints. Patients were considered eligible to receive this regimen if they were diagnosed morphologically to have APL on FAB criteria.2 This was sufficient to initiate therapy with As2O3. To be included in the analysis, the diagnosis had to be subsequently confirmed by fluorescent in-situ hybridization (FISH) or by reverse-transcriptase–polymerase chain reaction (RT-PCR) assay for PML-RARα transcripts. At the onset, exclusion criteria included women who were pregnant, or younger than 10 years or older than 55 years. Following the favorable outcome in the occasional patient treated on a compassionate basis outside the stipulated age limit, due to absence of resources for conventional therapy, it was decided to remove age as an exclusion criterion from January 2001. A written informed consent was obtained from all patients in accordance with the Declaration of Helsinki.
Intravenous arsenic trioxide
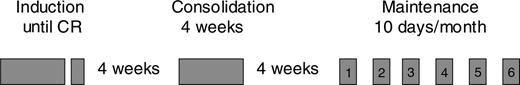
From the onset of the study until November 2003, As2O3 was prepared in the pharmacy department of the institution using the earlier published protocol.14 From December 2003, commercially available As2O3 was used (INTAS Pharmaceuticals, Matoda, Gujarat, India). Arsenic trioxide was administered by diluting 10 mg per 10-mL vial in 500 mL dextrose saline for adults and in 200 mL dextrose saline in the pediatric population and infusing it intravenously over 2 to 3 hours, once a day, without electrocardiographic monitoring. The schedule of single-agent As2O3 used in this study is summarized in Figure 1. Briefly, single-agent As2O3 was administered initially until complete hematologic remission (CR) or a maximum of 75 days (from January 2001, it was reduced to a maximum of 60 days). Following a 4-week interval, for those in CR, single-agent As2O3 was administered for another 4 weeks as a consolidation course. Subsequently after a second 4-week interval, for those continuing to remain in CR, single-agent As2O3 was administered 10 days a month for 6 months.
Supportive care
Complete blood counts (CBCs) were done daily for the first 2 weeks or until the patient was clinically stable, whichever occurred earlier. The CBCs were subsequently done on alternate days in induction, weekly in consolidation, and at each subsequent visit in maintenance and follow-up. Bone marrow analysis was done at the end of induction when 2 sequential CBCs were consistent with CR. If the bone marrow analysis showed evidence of persistent disease, then As2O3 was continued and the bone marrow analysis was repeated at weekly intervals until CR was documented or until the maximum duration of the induction period.
Coagulation parameters were monitored on alternate days for the first 2 weeks or until the patient was clinically stable and included a prothrombin time (PT), activated partial thromboplastin time (aPTT), and thrombin time (TT) performed by standard methods. Fibrinogen level was assayed if deranged coagulation parameters persisted in spite of attempted correction by fresh-frozen plasma (FFP). Once the patient was clinically stable, platelet count was higher than 50 × 109/L, and more than 3 serial readings of coagulation parameters were normal, the frequency of testing was reduced to once a week in induction. Unless clinically indicated, these tests were not monitored in consolidation or maintenance.
Liver function tests (LFTs) were done twice a week in induction, once a week in consolidation, and at each visit in maintenance and subsequent follow-up. Renal function tests and electrolytes including creatinine, sodium, potassium, calcium, phosphorous, and magnesium were monitored similarly in induction, consolidation, and maintenance.
Electrocardiogram (ECG) was done only if clinically indicated.
Platelet concentrates were transfused to maintain a platelet count higher than 20 × 109/L. Fresh-frozen plasma was infused (15 mL/kg) if the PT or aPTT was deranged, and cryoprecipitate was infused if the TT was prolonged or fibrinogen level was less than 1 g/L (100 mg/100 mL). Packed red cell transfusions were infused to maintain a hemoglobin level higher than 80 g/L (8 g%). Antibiotics and antifungal drugs were administered for fever as required.
Supplemental electrolytes were administered intravenously, if required, to maintain electrolyte levels within the normal range.
Regimen of single-agent arsenic trioxide. Arsenic trioxide was administered intravenously at a dose of 10 mg for adults and 0.15 mg/kg for pediatric patients until CR. Another 4-week course (consolidation) was administered after a 4-week interval for those achieving CR. Subsequently, after a second 4-week interval it was administered for 10 days/month for 6 months (maintenance).
Regimen of single-agent arsenic trioxide. Arsenic trioxide was administered intravenously at a dose of 10 mg for adults and 0.15 mg/kg for pediatric patients until CR. Another 4-week course (consolidation) was administered after a 4-week interval for those achieving CR. Subsequently, after a second 4-week interval it was administered for 10 days/month for 6 months (maintenance).
For patients who presented with high counts at diagnosis or had leukocytosis following initiation of therapy, hydroxyurea was administered as per the guidelines illustrated in Table 1. One or 2 doses of an anthracycline were administered at the clinician's discretion if patients developed a differentiation syndrome not resolving or continuing to worsen after administration of dexamethasone, or if there was leukocyte count higher than 50 × 109/L at presentation or rapidly progressive leukocytosis defined as a rise higher than 30 × 109/L in the first week or higher than 50 × 109/L in the second week in spite of administering hydroxyurea as per the guidelines.
Guidelines for administration of hydroxyurea during induction
WBC count, × 109/L . | Adult patients . | Pediatric patients . |
|---|---|---|
| 5 to 10 | 500 mg once daily | 15 mg/kg once daily |
| 10 to 15 | 500 mg twice daily | 15 mg/kg twice daily |
| 15 to 20 | 500 mg thrice daily | 15 mg/kg thrice daily |
| 20 to 50 | 500 mg 4 times a day | 15 mg/kg 4 times a day |
| More than 50 | 1.0 g 4 times a day | 30 mg/kg 4 times a day |
WBC count, × 109/L . | Adult patients . | Pediatric patients . |
|---|---|---|
| 5 to 10 | 500 mg once daily | 15 mg/kg once daily |
| 10 to 15 | 500 mg twice daily | 15 mg/kg twice daily |
| 15 to 20 | 500 mg thrice daily | 15 mg/kg thrice daily |
| 20 to 50 | 500 mg 4 times a day | 15 mg/kg 4 times a day |
| More than 50 | 1.0 g 4 times a day | 30 mg/kg 4 times a day |
For adult and pediatric patients with a WBC count less than 5 × 109/L, no hydroxyurea was administered.
RT-PCR
RT-PCR analysis for PML-RARα fusion transcripts with a sensitivity of 10–4 was done according to established protocols.4 RT-PCR was done at diagnosis, at the end of induction, and prior to initiating consolidation (first, third, and sixth maintenance course). At follow-up, RT-PCR was performed once in 6 months for 5 years.
Follow-up
After completion of the scheduled therapy, patients were followed up once in 3 months for the first 2 years and once in 6 months for the next 3 years.
Definition of outcomes
Achievement of CR required patients to have no clinical evidence of APL, an ANC higher than 1.5 × 109/L, an unsupported platelet count of more than 100 × 109/L, and a bone marrow analysis showing normocellularity to moderate hypocellularity with less than 5% blasts plus promyelocytes. Exception was made in patients who achieved unsupported platelet count higher than 100 × 109/L for more than 2 weeks with no evidence of residual disease as defined previously but had an ANC lower than 1.5 × 109/L.
Molecular relapse was defined as 2 consecutive positive RT-PCRs at an interval of 1 month apart after achieving molecular remission.
OS was defined as time from initiating treatment to last follow-up or death. Event-free survival was calculated from time of initiating therapy to last follow-up or an event (relapse or death). Disease-free survival (DFS) was calculated from time of achieving CR to last follow-up or an event (relapse).
Monitoring toxicity
Toxicities were documented using the National Cancer Institute–Common Toxicity Criteria version 2.0 (NCI-CTC v2.0; Bethesda, MD). Therapy with As2O3 was discontinued for any grade 3/4 toxicity and the patient rechallenged once the abnormality was corrected or if the grade reduced to less than 3. If grade 3/4 toxicity persisted after discontinuation of As2O3 or recurred on rechallenging the individual, the drug was discontinued. Criteria for diagnosis of a differentiation syndrome or retinoic acid syndrome were those defined in earlier studies.16,17
Statistical analysis
Analysis was done on an intention-to-treat basis. The χ2 or Fisher exact test was used to compare differences between groups for response to therapy. The probability of survival was estimated with the use of the product-limit method of Kaplan and Meier for overall survival, event-free survival, and disease-free survival and compared by the log-rank test. All survival estimates are reported ± 1 SE. The relationships of clinical features to outcome were analyzed by Cox proportional hazard model. All P values were 2-sided, with values of .05 or less indicating statistical significance. Statistical analysis was performed using SPSS 11.0 software (SPSS, Chicago, IL).
Results
Patient accrual and baseline characteristics
Between January 1998 and December 2004, 72 patients with PML/RARα+ APL were treated with this regimen. The baseline characteristics of the patients are summarized in Table 2. Seven additional patients, in this interval, who were considered eligible to receive this therapy were excluded: in 4 patients, the diagnosis could not be confirmed by RT-PCR; 2 patients were t(11;17); and 1 patient died shortly after admission before molecular confirmation of the diagnosis.
Baseline characteristics of patients
Characteristic . | Median, n . | Percent . | Impact on EFS, P . |
|---|---|---|---|
| Age, y (range) | 28 (3-75) | NA | NS |
| Younger than 10 | 5 | 6.9 | NS |
| 11 to 20 | 18 | 25 | NS |
| 21 to 55 | 44 | 61.1 | NS |
| Older than 55 | 5 | 6.9 | NS |
| Sex, M | 38 | 52.8 | NS |
| Duration of symptoms, d (range) | 21 (4-42) | NA | NS |
| Fever | 45 | 62.5 | NS |
| Hemorrhage | |||
| Mucosal | 31 | 43.5 | NS |
| CNS | 2 | 2.8 | NS |
| Organomegaly | 7 | 9.7 | NS |
| Hb level, less than 100 g/L, % | 53 | 73.6 | NS |
| WBC count, × 109/L (range) | |||
| Less than 1 | 7 | 9.7 | NS |
| Less than 2.5 | 34 | 47.2 | NS |
| Less than 5 | 45 | 62.5 | .032 |
| Less than 10 | 55 | 76.3 | NS |
| Platelet count, × 109/L | |||
| More than 10 | 53 | 73.6 | .028 |
| More than 20 | 29 | 40.2 | .020 |
| More than 40 | 12 | 16.6 | NS |
| PT, prolonged | 12 | 16.7 | .023 |
| APTT, prolonged | 3 | 4.2 | .051 |
| LDH (range) | 516 (226-2385) | NA | NS |
| RT-PCR | |||
| bcr 1 | 46 | 63.8 | NS |
| bcr 2 | 5 | 6.9 | NS |
| bcr 3 | 21 | 29.2 | NS |
Characteristic . | Median, n . | Percent . | Impact on EFS, P . |
|---|---|---|---|
| Age, y (range) | 28 (3-75) | NA | NS |
| Younger than 10 | 5 | 6.9 | NS |
| 11 to 20 | 18 | 25 | NS |
| 21 to 55 | 44 | 61.1 | NS |
| Older than 55 | 5 | 6.9 | NS |
| Sex, M | 38 | 52.8 | NS |
| Duration of symptoms, d (range) | 21 (4-42) | NA | NS |
| Fever | 45 | 62.5 | NS |
| Hemorrhage | |||
| Mucosal | 31 | 43.5 | NS |
| CNS | 2 | 2.8 | NS |
| Organomegaly | 7 | 9.7 | NS |
| Hb level, less than 100 g/L, % | 53 | 73.6 | NS |
| WBC count, × 109/L (range) | |||
| Less than 1 | 7 | 9.7 | NS |
| Less than 2.5 | 34 | 47.2 | NS |
| Less than 5 | 45 | 62.5 | .032 |
| Less than 10 | 55 | 76.3 | NS |
| Platelet count, × 109/L | |||
| More than 10 | 53 | 73.6 | .028 |
| More than 20 | 29 | 40.2 | .020 |
| More than 40 | 12 | 16.6 | NS |
| PT, prolonged | 12 | 16.7 | .023 |
| APTT, prolonged | 3 | 4.2 | .051 |
| LDH (range) | 516 (226-2385) | NA | NS |
| RT-PCR | |||
| bcr 1 | 46 | 63.8 | NS |
| bcr 2 | 5 | 6.9 | NS |
| bcr 3 | 21 | 29.2 | NS |
NS indicates not significant; NA, not applicable.
Induction therapy
Of the 72 eligible patients, 62 (86.11%) achieved hematologic complete remission (CR). Of the remaining 10, there were 7 early deaths (mean: 4.3 days, range: 2-7 days) secondary to intracranial (IC) bleeds. Three additional patients died prior to achieving a CR, on days 20, 23, and 49, secondary to uncontrolled sepsis, IC bleed, and a differentiation syndrome, respectively. Eight (11.1%) patients received an anthracycline in induction (7, mitoxantrone; 1, daunorubicin). Indications included a differentiation syndrome in 2 and high leukocyte count at presentation or a rapid leukocytic response in 6 cases. Hydroxyurea was administered to 53 (73.6%) patients for high leukocyte count at presentation or a leukocytic response following administration of As2O3. Hydroxyurea was administered for a median period of 11 days (range: 2-32 days) and a median cumulative dose of 12 g (range: 1-40.5 g). The median time to achieve CR was 42 days (range: 24-70 days). Results for molecular monitoring of PML/RARα by RT-PCR were available in 54 patients at the end of induction, of which 43 (79.6%) were positive and 11 (20.3%) were negative. RT-PCR performed again, prior to onset of consolidation, after a drug-free interval of 4 weeks showed that all 11 who had earlier attained molecular remission (MR) remained negative, while 30 of the 43 who were positive had become negative and 12 continued to remain positive, and RT-PCR was not done in 1 of these patients, at this time point. The median hospital stay in induction was 22 days (range: 0-65 days). During this period, the median time on antibiotics was 11.2 days (range: 0-56 days). Median red cell, platelet, and FFP support in induction were 2.5 units (range: 0-16 units), 15.5 units (range: 0-66 units), and 2 units (range: 0-16 units), respectively.
Consolidation and maintenance
Consolidation and maintenance courses were administered on an outpatient basis without cardiac monitoring in patients who continued to remain in CR. Of the 62 patients who achieved CR, in 2 patients therapy was discontinued, 1 due to persistent neutropenia and the other due to recurrent grade 3 transaminitis. Both patients were subsequently treated with a combination of ATRA and chemotherapy. The patient with persistent neutropenia relapsed on day 572. The patient with transaminitis also had persistent high-grade fever and was found on liver biopsy to have a noncaseating granulomatous hepatitis that resolved on antituberculous therapy; this patient continues to be in remission at 1 year. One patient had an isolated CNS relapse detected during the second maintenance course. Of the remaining 59 patients who completed the consolidation and maintenance course as scheduled, only 4 patients required hospital admission during this period. The admissions were for febrile neutropenia, acute onset diarrhea, nonneutropenic fever, and hepatitis, and the duration of admission was 8, 3, 5, and 4 days, respectively. Four of the 60 patients who received the consolidation course developed transient (< 1 week) grade 3/4 neutropenia; only 1 of these patients required admission. None of the remaining patients had grade 3/4 cytopenia or mucositis during either consolidation or maintenance. Excluding the period of hospital admission, for those who required it, the ECOG performance score was 0/1 for all patients through the duration of consolidation and maintenance. All patients who had achieved molecular remission prior to onset of consolidation remained in MR at the end of consolidation, while of the 12 who were positive 11 achieved MR at the end of consolidation and 1 patient achieved MR at the end of the first course of maintenance.
Toxicity profile
Apart from the 7 early deaths secondary to IC bleeds, there were 3 deaths in induction. One patient developed a differentiation syndrome that required intubation and ventilatory support; this patient subsequently died on day 49 from a probable fungal pneumonia prior to extubation. Two other patients died from uncontrolled sepsis on days 20 and 23. After remission induction, only 4 patients developed grade 3/4 neutropenia; all instances of neutropenia occurred during the consolidation course and were transient (< 1 week), and only 1 patient developed febrile neutropenia that required admission. In all these cases, after a brief period of discontinuation of the drug, it could be administered safely again without recurrence of cytopenia.
The nonhematologic toxicities in the majority of patients were mild, frequently reverted on continuing As2O3, and in the rest the toxicities were reversible on discontinuing the drug for an interval of 1 to 2 weeks.
Grade 3/4 hepatotoxicity was seen in 5 (6.9%) patients. Arsenic trioxide was discontinued for a mean period of 18.2 days (range: 7-28 days) for these patients. In this interval, the liver function tests reverted to normal levels in 4 patients and the abnormality did not recur on rechallenging with As2O3, nor was there evidence of hepatic compromise/decompensation in these patients on follow-up. In one patient with grade 3 toxicity, the hepatic dysfunction recurred on rechallenging with As2O3, and therapy with this drug was discontinued.
One patient, who developed grade 2 hepatotoxicity during maintenance, has persistent asymptomatic grade 1 transaminitis, 6 months after completion of therapy.
There were no sudden deaths attributable to a cardiac event in this series of patients, and on follow-up there were no documented second malignancies.
The toxicity profile of this regimen is summarized in Table 3.
Toxicity profile
Toxicity* . | N (%) . |
|---|---|
| Hepatotoxicity | |
| Grade 1 | 9 (12.5) |
| Grade 2 | 7 (9.7) |
| Grade 3 | 3 (4.1) |
| Grade 4 | 2 (2.7) |
| Neurotoxicity | |
| Grade 1 | 11 (15.2) |
| Grade 2 | 1 (1.3) |
| Grade 3 | 2 (2.7) |
| GIT: nausea, decreased appetite, dyspepsia; grade 1 | 7 (9.7) |
| Skin: hyperpigmentation, hypopigmentation, dryness; grade 1 | 18 (25) |
| Cardiac | |
| Nonspecific T-wave inversion, grade 1 | 1 (1.3) |
| SVT, grade 2 | 1 (1.3) |
| Weight gain | 4 (5.5) |
| Grade 1 | 1 (1.3) |
| Grade 3 | |
| Somnolence, grade 1 | 2 (2.7) |
| Definite differentiation syndrome | 5 (6.9) |
Toxicity* . | N (%) . |
|---|---|
| Hepatotoxicity | |
| Grade 1 | 9 (12.5) |
| Grade 2 | 7 (9.7) |
| Grade 3 | 3 (4.1) |
| Grade 4 | 2 (2.7) |
| Neurotoxicity | |
| Grade 1 | 11 (15.2) |
| Grade 2 | 1 (1.3) |
| Grade 3 | 2 (2.7) |
| GIT: nausea, decreased appetite, dyspepsia; grade 1 | 7 (9.7) |
| Skin: hyperpigmentation, hypopigmentation, dryness; grade 1 | 18 (25) |
| Cardiac | |
| Nonspecific T-wave inversion, grade 1 | 1 (1.3) |
| SVT, grade 2 | 1 (1.3) |
| Weight gain | 4 (5.5) |
| Grade 1 | 1 (1.3) |
| Grade 3 | |
| Somnolence, grade 1 | 2 (2.7) |
| Definite differentiation syndrome | 5 (6.9) |
Grades given are maximum grade according to NCI-CTC v2.0.
Differentiation syndrome
In this cohort of patients, there were 5 (6.9%) cases of definite differentiation syndrome or retinoic acid–like syndrome as evidenced by pulmonary infiltrates, tachypnea, fluid retention, and fever. The average time to onset following initiation of induction was 13.2 days (range: 6-21 days). The syndrome occurred in patients who had leukocytosis at diagnosis or a leukocytic response to As2O3. The mean leukocyte count at onset was 19.5 × 109/L (range: 4.8-45.8 × 109/L). Arsenic trioxide was discontinued temporarily and a course of dexamethasone given. In 2 cases, a dose of anthracycline was administered. One patient required intubation and ventilatory support and subsequently died of a probable fungal pneumonia, prior to extubation. The remaining patients were successfully rechallenged with As2O3 and completed the remainder of their induction regimen uneventfully. There were no cases of a differentiation syndrome documented either in consolidation or in maintenance.
Outcome
As of August 2005, at a median follow-up of 25 months (range: 8-92 months), of the 62 patients who completed induction there was one death in remission at 38.7 months of a suspected viral encephalitis and 6 patients relapsed. One relapse occurred during the second maintenance course and consisted of an isolated CNS relapse. The remaining relapses were all medullary and occurred at a median of 7.5 months from completion of therapy (range: 2-9 months). Sixty patients are alive, 55 in first CR. Serial RT-PCR monitoring revealed that 3 patients became transiently RT-PCR positive after achieving MR; in 2 cases it was prior to their third maintenance course and in 1 prior to the sixth maintenance course. In these 3 cases, repeat RT-PCR after a month was negative, and they have since continued to remain negative. At the time of analysis, one patient was RT-PCR positive, 5 months after completion of maintenance. This patient is scheduled to have a repeat RT-PCR after a month; a second positive reading would be required to define it as a molecular relapse. At the time of analysis, all 55 patients in first CR are in MR.
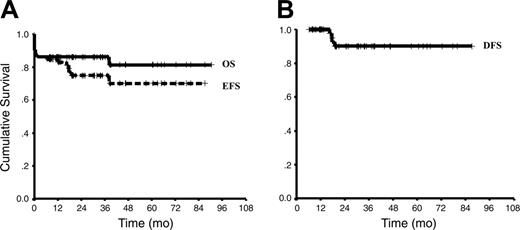
In this cohort, the 3-year Kaplan-Meier estimate of EFS, DFS, and OS was 74.87% ± 5.6%, 87.21% ± 4.93%, and 86.11% ± 4.08%, respectively (Figure 2A-B).
Of the 8 patients who received an anthracycline in induction for the indications listed earlier, 1 died on day 49 following onset of a differentiation syndrome. The remaining patients are in CR and MR at median follow-up of 19 months (range: 9.8-63.9 months).
Risk stratification
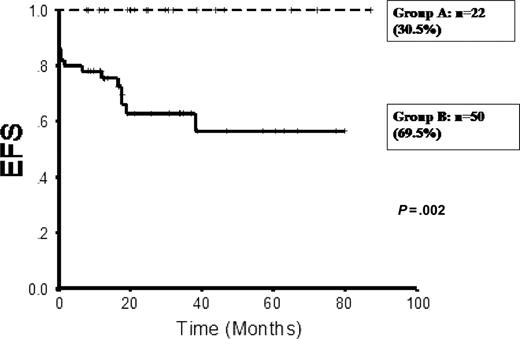
In a univariate analysis of factors (Table 2) at diagnosis that had an adverse impact on event-free survival, a statistically significant adverse effect was seen with a white blood cell (WBC) count higher than 5 × 109/L, a platelet count lower than 20 × 109/L (highest value at which a statistically significant discriminant value was noted), and a prolonged PT (P values: .032, .020, and .023, respectively). On a multivariate analysis, only a platelet count lower than 20 × 109/L retained a statistically significant adverse impact (RR = 5.23, P = .034), while WBC count higher than 5 × 109/L and prolonged PT showed an increased relative risk (RR = 1.4 and 2.8, respectively) with a trend to statistical significance. Prolonged PT, platelet count lower than 20 × 109/L, and WBC count higher than 5 × 109/L at diagnosis were seen in 12 (16.7%), 43 (59.7%), and 27 (37.5%) patients, respectively. The WBC count at diagnosis was retained in the subsequent risk stratification since it has been established to have a significant bearing on the treatment outcome of APL,18,19 and at the discriminate value of 5 × 109/L in this series, a substantial number of cases (37.5%) would fall into the adverse group for this parameter. Using the WBC and platelet count at diagnosis, 2 risk groups were identified: 1 with WBC count lower than 5 × 109/L and platelet count higher than 20 × 109/L (good risk, n = 22 [30.6%]) and the remaining patients (n = 50 [69.4%]). In the good-risk group, the 3-year Kaplan-Meier estimate of EFS, OS, and DFS was 100%, while in the rest the EFS, OS, and DFS were 62.78% ± 6.1%, 80% ± 5.6%, and 79.24% ± 7.69%, respectively (Figure 3). Statistical analysis of the survival curves by log-rank test between these 2 groups for EFS, OS, and DFS was significant (P values: .002, .021, and .045, respectively). Addition of the variable “prolonged PT” to the good-risk group did not alter the outcome in this group. There was no significant difference between the groups that had both WBC and platelet counts in the adverse range in comparison with a group that had either WBC or platelet count alone in the adverse range.
Kaplan-Meier product limit estimate of (A) overall survival (OS) and event-free survival (EFS) (n = 72). (B) Kaplan-Meier product limit estimate of disease-free survival (DFS) (n = 62).
Kaplan-Meier product limit estimate of (A) overall survival (OS) and event-free survival (EFS) (n = 72). (B) Kaplan-Meier product limit estimate of disease-free survival (DFS) (n = 62).
Comparison of Kaplan-Meier product limit estimate of event-free survival (EFS) between the good-risk group (group A: WBC count, < 5 × 109/L; platelet count, > 20 × 109/L) and the rest (group B).
Comparison of Kaplan-Meier product limit estimate of event-free survival (EFS) between the good-risk group (group A: WBC count, < 5 × 109/L; platelet count, > 20 × 109/L) and the rest (group B).
Discussion
This study shows that when single-agent As2O3 is used for induction, consolidation, and maintenance in the treatment of newly diagnosed cases of APL, it is associated with durable remissions, which are comparable with conventional ATRA plus chemotherapy regimens.20-22 However, longer follow-up is required to exclude the possibility of late relapses. When administered, as in the schedule published here, it is associated with minimal toxicity and is well tolerated. After remission induction, it can be administered on an outpatient basis; this, in combination with the absence of conventional toxicities of chemotherapy such as grade 3/4 neutropenia and mucositis, makes it significantly less expensive to administer. In our setting, administration of an ATRA plus chemotherapy regimen is associated with expenses of approximately $15 000 to $20 000, while this single-agent As2O3-based regimen is associated with expenses of approximately $3000 to $5000. The current market price of this drug in India is approximately $10/10-mg vial.
Unlike other myeloid malignancies, in APL, a maintenance schedule of therapy has a significant bearing on long-term outcome.20,23 Hence, at the onset of this study it was decided to administer a maintenance course of As2O3. In the absence of prior experience with such a regimen, an arbitrary duration of 6 months was used for this study. The optimal duration of such a maintenance regimen remains to be defined. The potential reduction in relapse risk on extending the duration of such a maintenance regimen has to be weighed against the potential for increasing the risk of cumulative toxicities including second malignancies.
A subset analysis of pediatric patients from this cohort, published earlier by our group, had documented the efficacy in this population.24 We and others have pointed out the potential advantage of this intravenous regimen, in this population, since there is no known intravenous formulation of ATRA for patients who cannot take it orally.24,25 In this series, there were 6 patients older than 50 years, with a median age of 56.5 years (range: 55-75 years). Two of these patients died prior to achieving a CR, one on day 4 secondary to an IC bleed and the other following the onset of a differentiation syndrome. The remaining patients are in continuous complete remission at a median follow-up of 16.5 months (range: 11.7-47 months). This elderly subset tolerated the regimen well, with none of the surviving patients experiencing any grade 3/4 toxicity.
Concerns have been raised in previous studies of the cardiac26-28 and hepatic29 toxicity with the use of As2O3. In this series, only one patient developed an arrhythmia (supraventricular tachycardia, without QTc prolongation), which occurred on day 4 of induction; this was associated with symptoms but reverted without treatment. Arsenic trioxide was discontinued for a day and subsequently administered as per the protocol without any further cardiac events. One other patient developed a retrosternal discomfort during induction and the ECG showed transient nonspecific T-wave inversions. In this patient, the regimen was continued without a break and completed uneventfully. The low incidence of cardiac-related toxic events in this series of newly diagnosed cases of APL could potentially be due to absence of exposure to anthracyclines or other cardiotoxic agents prior to this therapy and the attention to maintenance of electrolyte levels within the normal range. In the absence of cardiac monitoring, it is possible that transient QTc prolongations were missed. However, it has been noted that such a QTc interval prolongation on serial monitoring, in patients receiving As2O3, is an electrocardiographic finding rather than a clinical problem.15
In this series, hepatotoxicity was seen in 21 (29%) patients; in the majority (16/21), it was grade 1/2 and reverted to normal on continuing As2O3 as per the protocol. Of the 5 patients who developed grade 3/4 hepatotoxicity, in 4 patients, rechallenging with As2O3 once the hepatotoxicity had resolved did not lead to recurrence of the abnormality. There were no documented acute hepatic failures or cases with hepatic decompensation, though one patient had persistent grade 1 toxicity up to 6 months after completion of therapy. There was no effect of hepatotoxicity on EFS or OS. Patients who developed hepatotoxicity had better EFS than those who did not, though this did not reach statistical significance (data not shown). These observations are in contrast to an earlier publication that noted that 7 (63.63%) of 11 newly diagnosed patients developed hepatotoxicity and 2 of these failed to recover, with liver dysfunction contributing to their deaths.29 However, no other group has reported a similar hepatotoxicity profile. The hepatotoxicity profile in this series is similar to a more recently published study by Shen et al,30 where in the majority liver dysfunction was mild and returned to normal in 1 to 2 weeks.
A definite differentiation syndrome was seen in only 5 (6.9%) patients; this is lower than has been previously reported.31 It is possible that the use of hydroxyurea to control the leukocytic response contributed to this lower incidence. Excluding the patient who required ventilator support and subsequently died, in the rest it was easily controlled and did not recur on rechallenging with the drug. As with ATRA, it was seen only in induction.
Using the WBC and platelet counts at diagnosis, it was possible to identify a subset that had an excellent prognosis with this well-tolerated, predominantly outpatient-administered regimen. Even for this group, larger studies and further follow-up are required before it can be considered a standard alternative regimen. In the rest (group B), the outcome appears to be inferior to a similar subset treated with standard regimens, though such comparisons are difficult. A significant contributor to the lower EFS in this group was the early deaths secondary to IC bleeds, which could potentially be reduced by increasing the platelet and FFP/cryoprecipitate support in the first 2 weeks. There is also the potential that the addition of a synergistic agent such as ATRA,30 or an anthracycline in induction, could reduce the risk of relapse in this group, while retaining the low toxicity and outpatient basis of the rest of the regimen.
Prepublished online as Blood First Edition Paper, December 13, 2005; DOI 10.1182/blood-2005-08-3532.
An Inside Blood analysis of this article appears at the front of this issue.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 U.S.C. section 1734.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal