Abstract
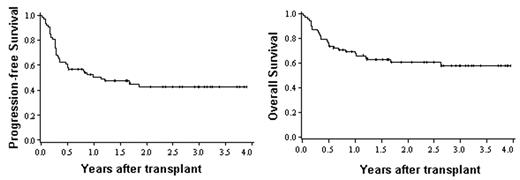
RIC regimens permit older and less fit patients to receive allogeneic stem cell transplantation (SCT). We designed a novel RIC regimen (cyclophosphamide, fludarabine, TBI [CY/FLU/TBI]) to achieve sufficient anti-neoplastic potency for cytoreduction and adequate immunosuppression for engraftment yet have limited treatment related mortality (TRM). We report the results of 72 patients (58% male) receiving sibling donor HLA-identical (n=66; 92%) or single antigen mismatched (n=6; 8%) G-CSF mobilized peripheral blood SCT from 2002–2005. Eligible patients were >55 years or had prior SCT, ongoing but controlled infections, ventricular ejection fraction 35–45% or corrected DLCO 30–50%. All patients had chemotherapy sensitive disease or remission. Most patients had lymphoma (n=29; 40%) or acute leukemia/MDS (n=23; 32%); others (28%) had multiple myeloma, CML, CLL, aplastic anemia, or renal cell carcinoma. All acute leukemia patients were in CR (CR1=14, ≥CR2=4). All lymphoma patients were chemosensitive; 4 were in CR. All patients received conditioning with FLU 40 mg/m2/day × 5 days, CY 50 mg/kg and 200 cGy TBI. Equine ATG 90 mg/kg plus methylprednisolone were given to those without recent combination chemotherapy (29%). GVHD prophylaxis included mycophenolate mofetil 1 gm BID and cyclosporine. The median age was 55 years (range, 11–65). The median graft cell dose infused was 5.4 × 106 CD34+ cells/kg (range, 0.6–15.5). Seventeen (24%) had previous SCT (14 autologous, 3 allogeneic). Neutrophil engraftment occurred at a median of 7 days (range, 0–13) and median time to platelet recovery >20K and >50K was 9 days (range, 0–51) and 14 days (range, 0–68), respectively. Median bone marrow chimerism by day 28 was 100% (range, 50–100); only 11 patients were <90%. The cumulative incidence (95% CI) of Grade 2–4 acute GVHD was 47% (35–59) and Grade 3–4 acute GVHD was 24% (14–33). Chronic GVHD at 2 years was 48% (34–62). Treatment related mortality at 100 days and 1 year was low [100 day (95% CI): 11% (4–18%); 1 year: 17% (8–25)]. Causes of death (n=29) included relapse (52%), GVHD (21%), organ toxicity (24%), and fungal infection (3%). The cumulative incidence (95% CI) of relapse/progression for all patients was 37% (25–49) at 2 years [acute leukemia/MDS, 47% (24–71); lymphoma, 37% (18–55)]. After a median 29 months (range, 6–48) follow-up of survivors, progression-free (PFS) and overall (OS) survival were encouraging: [PFS: 1 year, 51% (39–62); 3 years, 43% (31–55); OS: 1 year 68% (57–79); 3 years, 58% (45–70)]. Importantly, almost no events (relapse or death) have occurred beyond 2 years yielding a plateau in PFS and OS. This novel CY/FLU/TBI conditioning regimen is well tolerated, effective, and associated with promising PFS and OS. Further application and testing in multi-center studies is warranted.
Disclosure: No relevant conflicts of interest to declare.
Author notes
Corresponding author

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal