Abstract
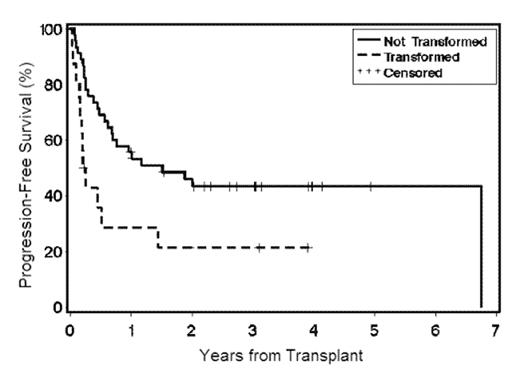
Sixty-two patients (pts) with chemotherapy-refractory indolent or transformed NHL were treated at 10 centers with allogeneic HCT from related (n=34) and unrelated (n=28) donors after 2 Gy total body irradiation with or without fludarabine. Diagnoses included follicular lymphoma (FL) (n=54, including 10 with grade 3 FL), small lymphocytic lymphoma (n=6), and marginal zone lymphoma (n=2). Median age was 54 years (range 33–66 years), and median time from diagnosis to HCT was 4.4 years (range 0.5–18.5 years). Sixteen pts had histologically documented transformation to diffuse aggressive lymphoma prior to HCT. Twenty-seven pts (44%) had failed autologous HCT. Disease status at the time of HCT was complete response (CR, n=16), partial response (PR, n=22), refractory (n=13), untested relapse (n=9), or unknown (n=2). Eleven of the 28 unrelated donor/recipient pairs (39%) had HLA mismatches: 2 at a single allele, 7 at a single antigen, and 2 at an antigen and an allele. One pt had non-fatal graft rejection from a 1-antigen-mismatched unrelated donor. Median follow-up of survivors after HCT was 36.6 months (range 2.3–60 months). Responses (CR [n=18] and PR [n=7]) were seen in 25 of 44 (57%) pts with evaluable disease prior to HCT, while 5 had stable disease, 9 progressed, and 5 were not evaluable due to early non-relapse mortality (NRM) on d27–d108. Two of 16 pts (13%) transplanted in CR relapsed; one was treated with donor lymphocyte infusion and achieved a persistent CR. The incidences of acute GVHD grades II–IV, III–IV, and chronic GVHD were 63%, 19%, and 53%, respectively. At 3 years, the risks of relapse/progression and NRM were 19% and 42%, respectively. There was a trend toward increased mortality with unrelated donors (HR 1.87 [0.9–3.7, p=0.08]). Progression-free and overall survival (PFS and OS) were significantly better in the non-transformed group (see tables 1 and 2).
Outcomes
| . | Non-transformed . | Transformed . |
|---|---|---|
| Relapse | 6/46 (13%) | 6/16 (38%) |
| NRM | 20/46 (43%) | 6/16 (38%) |
| 3-year OS | 24/46 (52%) | 4/16 (25%) |
| 3-year PFS | 20/46 (43%) | 4/16 (25%) |
| . | Non-transformed . | Transformed . |
|---|---|---|
| Relapse | 6/46 (13%) | 6/16 (38%) |
| NRM | 20/46 (43%) | 6/16 (38%) |
| 3-year OS | 24/46 (52%) | 4/16 (25%) |
| 3-year PFS | 20/46 (43%) | 4/16 (25%) |
Hazard Ratios (HR) for Transformed vs. Non-Transformed Pts
| . | HR (95% CI) . | p . |
|---|---|---|
| All-cause Mortality | 2.39 (1.2–4.9) | 0.02 |
| Relapse/progression | 4.75 (1.5–15) | 0.01 |
| Grade 3+ acute GVHD | 1.84 (0.5–6.3) | 0.35 |
| Extensive chronic GVHD | 1.96 (0.8–5.0) | 0.18 |
| . | HR (95% CI) . | p . |
|---|---|---|
| All-cause Mortality | 2.39 (1.2–4.9) | 0.02 |
| Relapse/progression | 4.75 (1.5–15) | 0.01 |
| Grade 3+ acute GVHD | 1.84 (0.5–6.3) | 0.35 |
| Extensive chronic GVHD | 1.96 (0.8–5.0) | 0.18 |
Figure
Allogeneic HCT after non-myeloablative conditioning can produce durable responses and prolonged survival in pts with refractory indolent or transformed NHL. Pts transplanted before histologic transformation had significantly better outcomes. Future efforts will focus on reducing NRM and identifying optimal timing of HCT.
Disclosure: No relevant conflicts of interest to declare.
Author notes
Corresponding author

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal