Comment on Mancuso et al, page 452
In this issue of Blood, Mancuso and colleagues present evidence that the number of apoptotic circulating endothelial cells is a promising predictor of outcome in patients undergoing metronomic chemotherapy for advanced breast cancer.
Breast cancer remains the leading cause of death in women aged 55 years or younger, and new approaches to treatment of advanced disease are urgently required. Neovascularization, or angiogenesis, is a rate-limiting step during tumorigenesis that promotes tumor cell survival and proliferation by ensuring a supply of oxygen and metabolites. In breast cancer, access to the vasculature also provides means for tissue invasion and metastasis to distant sites.
Antiangiogenic drugs and novel strategies that target the neovasculature are subjects of intense investigation and a popular focus of the drug development industry. One novel approach, termed “metronomic therapy,” uses long-term administration of low doses of chemotherapy, which effectively inhibits the tumor's drug-sensitive endothelial cell compartment.1 Preclinical models support the strong antiangiogenic effect of metronomic therapy1 ; however, classic methods for measuring regression of experimental tumors may not be appropriate for monitoring the efficacy of metronomic therapy in patients, and the development of reliable surrogate markers is required.
In this issue of Blood, Mancuso and colleagues quantified circulating endothelial cells (CECs) and circulating endothelial progenitors (CEPs) in the peripheral blood of patients with advanced breast cancer enrolled in a low-dose metronomic chemotherapy clinical trial.2 Whereas baseline CECs showed no relationship with clinical benefit, univariate and multivariate analyses revealed that higher numbers of CECs after 2 months of therapy were significantly associated with longer progression-free survival and overall survival.
A novel and key aspect of the current study, in contrast to previous preclinical and clinical studies in this area, is in the analysis of apoptotic (rather than viable or total) CECs and their correlation with clinical outcome. In those patients who gained a clinical benefit, the number of CECs increased significantly, with the increase derived from apoptotic CECs. In contrast, patients who experienced no clinical benefit exhibited a decline in CECs. These results suggest that apoptotic CECs may be a useful indicator of the efficacy of metronomic therapy. However, it remains unclear whether apoptosis induced in the CECs was via direct killing by metronomic therapy or was a consequence of deprivation of survival factors such as vascular endothelial growth factor (VEGF).FIG1
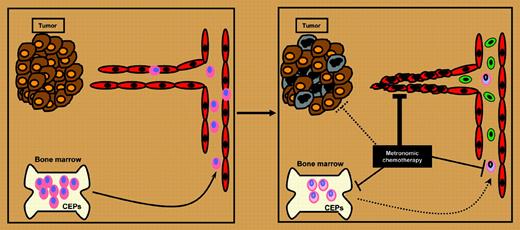
Revised model for the mechanism of metronomic chemotherapy. Metronomic chemotherapy may directly affect tumor cells (brown and gray ovals), may cause direct endothelial cell death or growth inhibition (red ovals), or may decrease the mobilization or viability of bone marrow–derived CEPs, which contribute to the tumor vasculature (pink ovals). The study by Mancuso and colleagues in this issue suggests that the primary mechanism of action is via induction of endothelial cell apoptosis (green ovals). Adapted from Shaked et al3 with the authors' permission.
Revised model for the mechanism of metronomic chemotherapy. Metronomic chemotherapy may directly affect tumor cells (brown and gray ovals), may cause direct endothelial cell death or growth inhibition (red ovals), or may decrease the mobilization or viability of bone marrow–derived CEPs, which contribute to the tumor vasculature (pink ovals). The study by Mancuso and colleagues in this issue suggests that the primary mechanism of action is via induction of endothelial cell apoptosis (green ovals). Adapted from Shaked et al3 with the authors' permission.
Using xenograft models, Mancuso and colleagues demonstrated that apoptotic CECs were not observed in cancer-free mice treated with chemotherapy, and concluded that apoptotic CECs in xenografted mice were derived from tumor-associated blood vessels (see figure). The possibility that apoptotic CECs arose from tumor vasculature is consistent with the “vessel normalization” model proposed by Jain.4 However, caution is necessary when extrapolating from preclinical models. Conclusive evidence of the origin of CECs in patients on metronomic therapy will depend on the development of methods that distinguish human CECs derived from tumor and bone marrow. Elucidation of the origin of the patients' apoptotic CECs will clarify the role of host-versus-tumor differences in CEC responses, which will have implications for the broader significance of this study to other types of cancers and treatments. More extensive translational clinical trials that follow a larger number of patients for a longer-term follow-up will determine whether a simple blood test can be used to identify and monitor cancer patients who will benefit from novel antiangiogenic therapies. ▪

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal