Around 20% to 30% of patients with Hodgkin lymphoma (HL) do not benefit from standard therapies and finally succumb to their disease. The factors that influence the outcome of HL have not been elucidated, underscoring the demand for the identification of biologic risk factors and new therapeutic targets. We analyzed the gene expression profiles of samples from 29 patients with advanced classic HL treated with standard therapy and compared the expression profiles of patients with favorable and unfavorable clinical outcome. Using supervised methods, we identified 145 genes associated with outcome, which were grouped into 4 signatures representing genes expressed by either the tumoral cells (genes involved in the regulation of mitosis and cell growth/apoptosis) or the tumor microenvironment. The relationship between the expression of 8 representative genes and survival was successfully validated in an independent series of 235 patients by quantification of protein expression levels on tissue microarrays. Analysis of centrosomes and mitotic checkpoint confirmed the existence of an abnormal transition through mitosis in HL cells. Therefore, genes related to tumor microenvironment, cell growth/apoptosis, and regulation of mitosis are associated with treatment response and outcome of patients with HL.
Introduction
Hodgkin and Reed-Sternberg (H/RS) cells represent a clonal expansion of germinal center (GC) B cells harboring rearranged and somatically mutated immunoglobulin genes1,2 and are characterized by a defective B-cell expression program.3 Several antiapoptotic and proproliferative mechanisms have been described in H/RS cells, such as constitutive activation of NF-κB 4,5 and STAT pathways6,7 and defects in the machinery of apoptosis and cell-cycle regulation.8,9 However, although many advances have been made in the understanding of biologic and pathogenic mechanisms, little of our knowledge has proved to be of any practical value in the clinical management of patients with Hodgkin lymphoma (HL).
Current therapeutic approaches using the ABVD (adriamycin, bleomycin, vinblastine, dacarbazine) regimen10 and more recent protocols such as bleomycin, etoposide, doxorubicin, cyclophosphamide, vincristine, procarbazine, and prednisone (BEACOPP)11 and Stanford V (mechlorethamine, doxorubicin, vinblastine, vincristine, bleomycin, etoposide, prednisone, granulocyte colony–stimulating factor)12 in combination with radiotherapy tailored to the stage of the disease are, in general, very effective for the treatment of HL, but about 20% to 30% of patients will nevertheless eventually die of the disease.13,14 In the long-term, progressive disease remains the main cause of death regardless of the modality of treatment used and the prognostic factors present at diagnosis. The ultimate reasons for this unsuccessful outcome have not yet been elucidated. Moreover, these therapies have additional consequences, because treatment-associated late toxicities (especially secondary malignancies and cardiovascular disease) may eventually develop. These may further reduce the number of long-term survivors.14
This situation has stimulated increasing interest in identifying factors that allow the identification of different groups of patients who will require more or less intensive therapy.15,16 For the time being, the best prognostic system available in clinical practice is the International Prognostic Score (IPS).17 However, this index is far from perfect because it fails to identify patients with very bad prognosis, and its applicability to earlier stages of the disease is also unclear.18
In this context, 2 important goals in HL research are the identification of reliable biologic factors that allow risk stratification of patients with HL and the discovery of new therapeutic targets.15 So far, gene expression signatures have been identified for the most common types of non-Hodgkin lymphomas using DNA microarrays,19-22 and the relationship between clinical outcomes and expression profiles of different lymphoma types has been investigated.22-25 These studies have also proved the ability of these technologies to identify new molecular targets and biologic processes involved in the pathogenesis of the diseases.
In the study reported here, we used gene expression analysis for the identification of specific gene signatures associated with favorable or unfavorable clinical outcome in patients with classic HL with advanced stages. We found 145 genes whose expression was associated with treatment response. These genes were grouped into 4 signatures composed of genes related to tumor microenvironment, genes implicated in the regulation of the mitotic checkpoint, and cell growth/apoptosis. These findings were validated in an independent series of 235 patients with HL by quantification of protein levels using tissue microarrays (TMAs).
Patients, materials, and methods
Patient samples
Pretreatment samples from 29 patients with advanced classic HL (training set) were selected according to homogeneous criteria: negative HIV status; advanced disease (stages III/IV, or stage II with B symptoms and/or bulky masses); availability of representative frozen lymph node samples; and uniform, standard modalities of first-line treatment for advanced clinical stages (ABVD or similar regimens).
To evaluate treatment response we used the most consistent surrogate of the final outcome of the disease: patients who achieved complete remission and maintained it for more than 12 months were classified in the favorable outcome group; conversely, patients who failed to achieve complete remission, had progressive disease, or had a short period before relapse were classified in the unfavorable outcome group.26,27 The training set was intentionally biased to include 2 balanced groups containing representative samples of treatment responders and nonresponders, respectively. Thus, we selected 14 patients with a favorable outcome and 15 with an unfavorable outcome (Table 1). Biopsy specimens and clinical data were retrospectively obtained from the files of the participant institutions of the Spanish Hodgkin Lymphoma Study Group,9,28 and the histologic confirmation of classic HL was achieved in all the cases by central review.
Clinical characteristics of the patients in the training set
No. . | Age, y . | Sex . | HL subtype . | Ann Arbor stage . | B symptoms . | Bulky masses . | Outcome* . |
|---|---|---|---|---|---|---|---|
| 1 | 34 | M | MC | III | No | No | FR |
| 2 | 82 | F | NS | IV | Yes | No | FR |
| 3 | 36 | F | NS | III | Yes | Yes | FR |
| 4 | 55 | M | NS | II | No | Yes | FR |
| 5 | 22 | M | NS | III | Yes | No | FR |
| 6 | 31 | M | NS | II | Yes | Yes | FR |
| 7 | 80 | F | MC | III | Yes | No | FR |
| 8 | 22 | M | NS | II | Yes | Yes | FR |
| 9 | 41 | M | NS | IV | Yes | No | FR |
| 10 | 23 | M | NS | II | No | Yes | FR |
| 11 | 28 | M | MC | II | No | Yes | FR |
| 12 | 61 | F | NS | II | Yes | Yes | FR |
| 13 | 38 | M | NS | II | Yes | Yes | FR |
| 14 | 16 | M | NS | II | Yes | Yes | FR |
| 15 | 70 | M | NS | IV | Yes | No | UR |
| 16 | 57 | F | MC | IV | Yes | No | UR |
| 17 | 61 | F | NS | IV | Yes | No | UR |
| 18 | 22 | F | NS | IV | Yes | No | UR |
| 19 | 28 | F | NS | II | Yes | Yes | UR |
| 20 | 19 | M | NS | II | No | Yes | UR |
| 21 | 37 | F | MC | III | Yes | No | UR |
| 22 | 17 | F | NS | II | Yes | No | UR |
| 23 | 48 | M | MC | III | No | No | UR |
| 24 | 35 | M | NS | II | Yes | Yes | UR |
| 25 | 56 | M | NS | II | No | Yes | UR |
| 26 | 24 | F | NS | IV | Yes | No | UR |
| 27 | 24 | M | NS | III | Yes | Yes | UR |
| 28 | 26 | M | NS | IV | Yes | Yes | UR |
| 29 | 47 | M | NS | IV | Yes | No | UR |
No. . | Age, y . | Sex . | HL subtype . | Ann Arbor stage . | B symptoms . | Bulky masses . | Outcome* . |
|---|---|---|---|---|---|---|---|
| 1 | 34 | M | MC | III | No | No | FR |
| 2 | 82 | F | NS | IV | Yes | No | FR |
| 3 | 36 | F | NS | III | Yes | Yes | FR |
| 4 | 55 | M | NS | II | No | Yes | FR |
| 5 | 22 | M | NS | III | Yes | No | FR |
| 6 | 31 | M | NS | II | Yes | Yes | FR |
| 7 | 80 | F | MC | III | Yes | No | FR |
| 8 | 22 | M | NS | II | Yes | Yes | FR |
| 9 | 41 | M | NS | IV | Yes | No | FR |
| 10 | 23 | M | NS | II | No | Yes | FR |
| 11 | 28 | M | MC | II | No | Yes | FR |
| 12 | 61 | F | NS | II | Yes | Yes | FR |
| 13 | 38 | M | NS | II | Yes | Yes | FR |
| 14 | 16 | M | NS | II | Yes | Yes | FR |
| 15 | 70 | M | NS | IV | Yes | No | UR |
| 16 | 57 | F | MC | IV | Yes | No | UR |
| 17 | 61 | F | NS | IV | Yes | No | UR |
| 18 | 22 | F | NS | IV | Yes | No | UR |
| 19 | 28 | F | NS | II | Yes | Yes | UR |
| 20 | 19 | M | NS | II | No | Yes | UR |
| 21 | 37 | F | MC | III | Yes | No | UR |
| 22 | 17 | F | NS | II | Yes | No | UR |
| 23 | 48 | M | MC | III | No | No | UR |
| 24 | 35 | M | NS | II | Yes | Yes | UR |
| 25 | 56 | M | NS | II | No | Yes | UR |
| 26 | 24 | F | NS | IV | Yes | No | UR |
| 27 | 24 | M | NS | III | Yes | Yes | UR |
| 28 | 26 | M | NS | IV | Yes | Yes | UR |
| 29 | 47 | M | NS | IV | Yes | No | UR |
There were no significant statistical differences between the 2 groups (FR and UR) of patients in any of the variables.
MC indicates mixed-cellularity HL; NS, nodular-sclerosis HL.
Response to first-line treatment: favorable treatment response (FR): sustained complete remission; unfavorable treatment response (UR): progressive disease, failure to achieve complete remission, or relapse within 12 months. See “Patient samples.”
The validation set consisted of biopsy samples from 235 patients with classic HL including both early and advanced stages regardless of their clinical outcome (Table 2). All the samples for the training and validation sets were collected with the collaboration of the Spanish National Tumor Bank Network, coordinated by the Spanish National Cancer Centre (CNIO), following the technical and ethical procedures of the network, including anonymization processes. Approval was obtained from the CNIO institutional review board. Informed consent was obtained in all cases.
Clinical characteristics of the patients in the validation set*
Characteristic . | Value . |
|---|---|
| Mean age, y (range) | 38.7 (10-86) |
| Sex, no. (%) | |
| Male | 117 (49.8) |
| Female | 118 (50.2) |
| Diagnosis, no. (%) | |
| Nodular sclerosis HL | 138 (58.7) |
| Mixed cellularity HL | 79 (33.6) |
| Lymphocyte-rich classic HL | 12 (5.1) |
| Lymphocyte-depleted HL | 6 (2.5) |
| Stage, no. (%) | |
| I | 31 (13.2) |
| II | 115 (48.9) |
| III | 55 (23.4) |
| IV | 34 (14.5) |
| IPS, no. (%) | |
| 0-2 | 172 (74.5) |
| 3 or more | 59 (25.5) |
| Outcome, no. (%) | |
| FR | 197 (86) |
| UR | 32 (14) |
| Follow-up, no. (%) | |
| ACR | 185 (78.4) |
| AWD | 17 (7.2) |
| DOD | 31 (14.0) |
Characteristic . | Value . |
|---|---|
| Mean age, y (range) | 38.7 (10-86) |
| Sex, no. (%) | |
| Male | 117 (49.8) |
| Female | 118 (50.2) |
| Diagnosis, no. (%) | |
| Nodular sclerosis HL | 138 (58.7) |
| Mixed cellularity HL | 79 (33.6) |
| Lymphocyte-rich classic HL | 12 (5.1) |
| Lymphocyte-depleted HL | 6 (2.5) |
| Stage, no. (%) | |
| I | 31 (13.2) |
| II | 115 (48.9) |
| III | 55 (23.4) |
| IV | 34 (14.5) |
| IPS, no. (%) | |
| 0-2 | 172 (74.5) |
| 3 or more | 59 (25.5) |
| Outcome, no. (%) | |
| FR | 197 (86) |
| UR | 32 (14) |
| Follow-up, no. (%) | |
| ACR | 185 (78.4) |
| AWD | 17 (7.2) |
| DOD | 31 (14.0) |
IPS indicates International Prognostic Score; FR, favorable treatment response; UR, unfavorable treatment response (see “Patient samples”); ACR, alive in complete remission; AWD, alive with disease; DOD, dead of disease.
The validation set of patients was selected from a previous series28 on the basis of the availability of tumor biopsy specimens. All patients were HIV negative.
To generate the gene expression signatures, a group of control samples was included in the study: 5 reactive lymph node samples, a pool of normal GC B cells (centroblasts) from healthy donors (isolated from 3 tonsillectomy specimens using anti-CD77 magnetic beads, as described elsewhere29 ), and 5 HL-derived cell lines (L-540, L-428, KM-H2, HDLM-2, L-1236) obtained from the German Collection of Microorganisms and Cell Cultures. RNA was obtained from 2 independent cultures of each of the cell lines at a homogeneous passage number.
Gene expression analysis
Gene expression profiles were analyzed using OncoChip.v2 cDNA microarrays20 produced at the CNIO. This platform contains 11 675 human clones representing 9348 genes selected on the basis of their proven or putative involvement in cancer. Total RNA was extracted with Trizol (Invitrogen, Carlsbad, CA), precipitated with isopropanol, and purified using the RNeasy kit (Qiagen, Hilden, Germany). RNA was amplified by double-stranded cDNA synthesis followed by T7-based in vitro transcription. Equal amounts of Cy3-labeled amplified RNA and Cy5-labeled Universal Reference RNA (Stratagene, La Jolla, CA) were hybridized onto OncoChip slides as described.20 The images were scanned with a G2565BA Microarray Scanner System (Agilent Technologies, Palo Alto, CA). The Cy3/Cy5 intensity ratios were quantified using GenePix Pro 5.1 software (Molecular Devices, Sunnyvale, CA) and normalized to the mean ratio value of all spots in the array.
Immunohistochemistry and protein quantification on TMAs
We assessed the expression of a selected number of markers in the validation set of samples using immunohistochemical techniques on TMAs, as previously described.9,30 Primary antibodies were as follows: anti-ALDH1A1, anti-STAT1, anti-RRM2, anti-SH2D1A (Santa Cruz Biotechnology, Santa Cruz, CA); anti-CDC2 (BD Biosciences, San Jose, CA); anti-MAD2L1 (BD Biosciences); anti-TOP2A (DAKO, Glostrup, Denmark); and anti-PCNA (EMD Biosciences, San Diego, CA). These markers were chosen as representative of the different signatures and were based on the availability of reliable antibodies.
The TMAs were scanned using a computerized microscope (BLISS system; Bacus Laboratories, Lombard, IL) and stored as digital images, as reported elsewhere.30 Protein levels were subsequently quantified by adjusting the appropriate thresholds for each marker using the TMAscore software package (Bacus Laboratories) following the manufacturer's recommendations.
Statistical analysis
The analysis of gene expression data was performed using public software created by the CNIO Bioinformatics Unit. Profiles with more than 20% of missing values and “flat patterns” (profiles with standard deviation across HL samples below 0.75) were excluded from the analyses. To identify differentially expressed genes, we used a supervised method based on a Student t test.31 Unadjusted P values were obtained from 100 000 permutations of the dataset, and false discovery rate (FDR) values were calculated by the method of Benjamini and Hochberg.32 Unsupervised clustering was performed using the Self-Organising Tree Algorithm (SOTA).33
For the survival analysis, patients in the validation set (n = 235) were grouped into quartiles according to the protein expression levels of each marker, considered as continuous variables. The end point was disease-specific survival (DSS), defined as the interval from the beginning of treatment to death from any cause directly related to the disease. Patients known to have died from causes unrelated to HL were censored. The association between the different markers and DSS was estimated by the Kaplan-Meier method and the log-rank test using the SPSS statistical program (SPSS, Chicago, IL).
Centrosome analysis
Centrosomes were visualized by indirect immunofluorescence on paraffin-embedded HL samples using an antibody against pericentrin-2 (kendrin).34 Simultaneous CD30 staining allowed the identification of H/RS cells. Centrosomes were considered abnormal if their diameter was at least twice that of centrosomes in normal cells or if they displayed numeric abnormalities, as described.35
Analysis of the mitotic checkpoint
Three HL-derived cell lines (L-1236, HDLM-2, and L-428) and lymphoblastoid (EBV-immortalized) B cells as controls were treated with 200 nM nocodazole (Sigma, St Louis, MO) and harvested at the indicated time points. To determine cell-cycle kinetics, cells were stained with propidium iodide and analyzed by flow cytometry (FACSCalibur; BD Biosciences). Mitotic index was assessed by direct visualization of DAPI (4′,6-diamidino-2-phenylindole)–stained cells under a fluorescence microscope. Between 200 and 500 cells were counted, and the mitotic index was calculated as the percentage of mitotic cells with respect to the total number of viable cells.
Results
Gene expression analysis
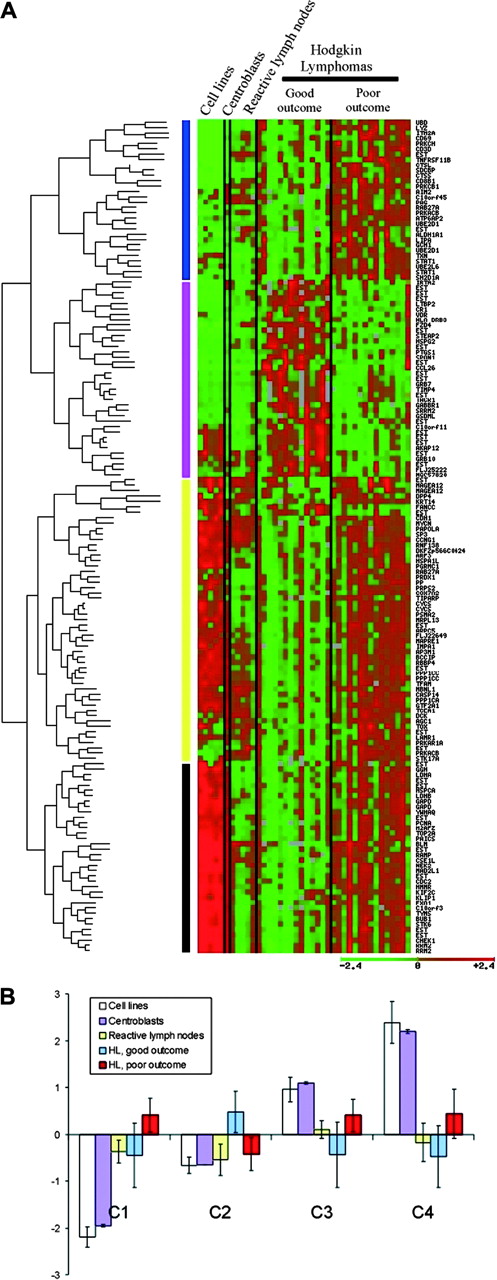
We analyzed the expression profiles of 9348 genes in samples from 29 patients with HL and in control samples (including normal lymph nodes, HL-derived cell lines, and normal GC B cells). Unsupervised hierarchic clustering of the complete dataset did not classify patients according to their treatment responses (Figure S1, available on the Blood website; see the Supplemental Materials link at the top of the online article). Therefore, we performed a supervised analysis with the purpose of identifying genes differentially expressed in the 2 groups of patients. We applied Student t test with a correction for multiple testing and ranked the genes by their FDR value. Thus, 145 genes had FDR values below 0.15 (corresponding to unadjusted P values less than .025) and were considered to be differentially expressed. Hierarchic clustering of the expression profiles of the selected genes across the series of HL samples and control samples allowed the identification of 4 clear gene clusters or signatures (Figure 1; Tables S1-S2).
The first 2 clusters consist of genes related to host immune response and tumor microenvironment. The first signature is overexpressed by the unfavorable outcome group of patients and mainly includes genes expressed by specific subpopulations of T cells (eg, CD8B1, CD3D, CD26, SH2D1A), macrophages (eg, ALDH1A1, LYZ, STAT1), and plasmacytoid dendritic cells (eg, ITM2A). The second signature, which is overexpressed by the favorable outcome group, consists of a heterogeneous set of genes involved in adhesion and remodeling of the extracellular matrix (eg, TIMP4, SPON1, LAMB1), genes implicated in fibroblast function and chemotaxis (eg, TACR1, CCL26), and molecules expressed by antigen-presenting cells (eg, CR1, HLA-DRB3) and specific populations of B cells (eg, IRTA2, VDR). Consistently, most of these genes are not expressed by HL cell lines or GC B cells. Their expression is also weak in normal lymph nodes.
Clusters 3 and 4 consist of genes overexpressed by the unfavorable outcome group of patients, most of which are highly expressed by HL-derived cell lines and normal GC B cells and display variable expression in reactive lymph nodes. Cluster 3 is a heterogeneous group of genes involved in apoptosis regulation (eg, CYCS, CASP14, HSPA1L), signal transduction (eg, PDCD10, PRKACB), and metabolism and cell growth (eg, COX7A2, MYCN, DCK). Finally, cluster 4 mainly includes genes coding for cell-cycle–regulatory proteins. Interestingly, most of these genes are involved in the regulation of the mitotic checkpoint (eg, MAD2L1, BUB1, STK6, CDC2, CHEK1). It is also noteworthy that many of these genes encode enzymes previously described as factors implicated in drug resistance in other tumor types (eg, RRM2, TYMS). Additional support for our interpretations is the fact that the gene encoding for topoisomerase 2 alpha (TOP2A), one of the cellular targets of adriamycin, is also found in this signature.
Immunohistochemical analysis in the validation set of patients
To validate the results of the gene expression profiling analysis, we explored the relationship between gene expression and clinical outcome in an independent series of 235 patients using a completely different technical approach: quantification of protein expression levels of 8 selected markers using TMAs and an automated quantification technique. These markers were chosen as representative of the immune response signatures (genes that are theoretically expressed by reactive cells: macrophages [ALDH1A1, STAT1] and T cells [SH2D1A]) and the cell-cycle signatures (genes that are theoretically expressed mainly by the neoplastic H/RS cells: TOP2A, RRM2, PCNA, MAD2L1, and CDC2) (Figure 2; Figure S2). In agreement with the gene expression data, there were clear differences in survival among quartiles for most of the markers, and the quartile with the highest level of expression displayed significantly shorter survival.
Gene expression signatures associated with clinical outcome of patients with HL. (A) The genes identified in a supervised analysis (t test) as differentially expressed (FDR below 0.15) between the 2 groups of patients (favorable versus unfavorable treatment response) were subjected to hierarchic clustering using the SOTA algorithm. Four main clusters or signatures were obtained (see “Gene expression analysis”). For the cell lines and the centroblasts, the average of 2 hybridizations is shown. (B) Histogram representing the average expression value of each signature in the different groups of samples (cell lines, centroblasts, normal lymph nodes, favorable outcome HL, and unfavorable outcome HL). Error bars represent standard deviations. C1 to C4 represents clusters 1 through 4.
Gene expression signatures associated with clinical outcome of patients with HL. (A) The genes identified in a supervised analysis (t test) as differentially expressed (FDR below 0.15) between the 2 groups of patients (favorable versus unfavorable treatment response) were subjected to hierarchic clustering using the SOTA algorithm. Four main clusters or signatures were obtained (see “Gene expression analysis”). For the cell lines and the centroblasts, the average of 2 hybridizations is shown. (B) Histogram representing the average expression value of each signature in the different groups of samples (cell lines, centroblasts, normal lymph nodes, favorable outcome HL, and unfavorable outcome HL). Error bars represent standard deviations. C1 to C4 represents clusters 1 through 4.
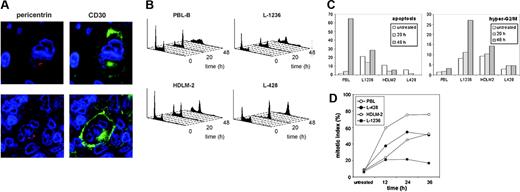
Analysis of the mitotic checkpoint and centrosome alterations in H/RS cells
The functions of the genes contained in cluster 4 clearly suggest that alterations in the regulation of the mitotic checkpoint may be an important biologic event influencing treatment resistance in HL. Thus, we decided to explore further the functional integrity of this checkpoint in H/RS cells. To this end, HL cell lines and lymphoblastoid B cells were treated with nocodazole, a microtubule-disrupting agent that inhibits spindle formation and activates the mitotic checkpoint, causing arrest in early mitosis. As depicted in Figure 3, lymphoblastoid B cells displayed a normal response to nocodazole, characterized by nearly complete mitotic arrest preceding massive apoptosis. In contrast, the checkpoint response in HL cell lines was impaired to a variable extent: mitotic arrest was incomplete, induction of apoptosis was weaker, and there was an increase in the hyper-G2/M population at late time points in L-1236 and, to a lesser extent, in HDLM-2 cells. These results clearly indicate the existence of a common disruption of the mitotic spindle checkpoint in H/RS cells compared with nontransformed B lymphocytes.
These findings are also strengthened by the existence of well-known alterations in chromosomal segregation, ploidy, and chromosomal instability in H/RS cells as common features of HL tumors. Because defects in centrosome replication may contribute to the acquisition of chromosomal aberrations and aneuploidy, we analyzed centrosome number and morphology in tissue sections from 31 HL tumors by immunofluorescence using pericentrin-2 as a centrosomal marker (Figure 3). Although a characteristic single or paired centrosome pattern was detectable in nonmalignant cells, we found structural and/or numeric aberrations in H/RS cells in 28 of 31 (90%) of samples, consistent with previous observations.34
Discussion
Classically, the clinical and histologic heterogeneity and the scarcity of tumoral cells have prevented molecular studies in HL. However, here we have demonstrated the feasibility of gene expression analysis in HL tumors following a stringent selection of samples with clearly defined clinical and pathologic criteria and using appropriate supervised methods based on class comparison. As a result, we identified clusters of functionally related genes that are associated with clinical outcome and are expressed by either the reactive cell component or the neoplastic H/RS cells. HL is the prototype of lymphoma in which survival and progression have been traditionally associated with the immune response,36,37 and many recent studies also suggest the importance of the microenvironment in outcome prediction in other tumors,24,38 underscoring the necessity of gene expression analysis using RNA extracted from whole-tissue samples.
To overcome the obstacles associated with gene expression studies, we used a homogeneous series, including only patients with advanced disease treated with uniform chemotherapeutic protocols, thus aiming at identifying gene signatures associated with specific and clearly opposed outcomes. Finally, we validated the potential prognostic value of a set of these new markers in an independent set of patients with an entirely different technical approach based on immunohistochemistry performed on TMAs. Although it was not the purpose of this study to construct a predictive model of treatment response in HL, the biologic variables identified here could potentially be included, after further validation, in a predictive system combining features of the H/RS cells and their cellular microenvironment.
Analysis of the relationship between gene expression and outcome in the validation set of patients. Immunohistochemical analysis of the expression of 8 selected genes in the validation series of patients using TMAs. The patients were grouped into quartiles according to the protein expression level of each marker, and the DSS of the fourth quartile (the one with the highest expression) was compared with that of the rest of the series (quartiles 1 to 3). For each marker, a representative field of a stained tissue section and the Kaplan-Meier curves are shown. Note ALDH1A1 and STAT1 immunostaining, restricted mainly to macrophages; SH2D1A immunostaining mainly in T cells; and TOP2A, RRM2, PCNA, MAD2L1, and CDC2 overexpression in the neoplastic H/RS cells. Micrographic images were obtained with a BLISS Slide Scanner (Bacus Laboratories) equipped with a Zeiss Axioplan 2 microscope (Zeiss, Oberkochen, Germany). A 40 ×/0.75 objective lens was used to visualize images, which were acquired through software provided with the BLISS scanner.
Analysis of the relationship between gene expression and outcome in the validation set of patients. Immunohistochemical analysis of the expression of 8 selected genes in the validation series of patients using TMAs. The patients were grouped into quartiles according to the protein expression level of each marker, and the DSS of the fourth quartile (the one with the highest expression) was compared with that of the rest of the series (quartiles 1 to 3). For each marker, a representative field of a stained tissue section and the Kaplan-Meier curves are shown. Note ALDH1A1 and STAT1 immunostaining, restricted mainly to macrophages; SH2D1A immunostaining mainly in T cells; and TOP2A, RRM2, PCNA, MAD2L1, and CDC2 overexpression in the neoplastic H/RS cells. Micrographic images were obtained with a BLISS Slide Scanner (Bacus Laboratories) equipped with a Zeiss Axioplan 2 microscope (Zeiss, Oberkochen, Germany). A 40 ×/0.75 objective lens was used to visualize images, which were acquired through software provided with the BLISS scanner.
The genes identified as differentially expressed between patients with favorable and unfavorable response are functionally clustered in 4 signatures remarkably consistent with the biologic features of HL tumors (Table S2). Thus, the first half of the genes reflect specific cell populations that participate in particular immune responses, some of which had been previously reported as modifiers of the clinical outcome (eg, cytotoxic T-cell response37,39 ). Additionally, we have identified new cell populations that can reflect certain immune or metabolic states (genes expressed either by monocyte/macrophage cells such as ALDH1A1, STAT1, or LYZ; antigen-presenting cells such as CR1, HLA-DRB3; or plasmacytoid dendritic cells such as ITM2A). The presence of STAT1-expressing reactive cells linked to unfavorable outcome, together with the expression of macrophage markers such as LYZ and ALDH1A1, is suggestive of an important role of tumor-associated macrophages. Macrophages infiltrated into a tumor have a complex, ambivalent relationship with cancer cells and can suppress local T-cell–mediated immune response through a STAT1-dependent mechanism, resulting in the inhibition of antitumor immunity and the promotion of tumor progression.40,41 Therefore, our data confirm and expand previous observations concerning the role of the cellular microenvironment in the pathogenesis of HL.
Alterations in the mitotic spindle checkpoint in H/RS cells. (A) Analysis of centrosomes in tissue sections from HL tumors. Immunofluorescence staining for pericentrin-2 (red) and CD30 (green) revealed structural and numeric aberrations in H/RS cells. Images were obtained with a TCS-SP2-AOBS-UV confocal microscope equipped with a PL-APO 100 ×/1.40-0.70 oil-immersion objective lens and LCS software (Leica Microsystems, Bannockburn, IL). (B) Cell-cycle profiles of HL-derived cell lines and lymphoblastoid B cells (PBL-B) treated with nocodazole. (C) Quantification of the percentage of apoptotic and hyper-G2/M cells in panel B. Lymphoblastoid cells displayed a normal response to nocodazole (mitotic arrest preceding massive apoptosis), whereas HL-derived cell lines had a lower apoptotic index and higher hyper-G2/M fraction at late time points. (D) Mitotic index after nocodazole treatment. HL-derived cell lines arrest in mitosis less efficiently than lymphoblastoid cells, indicating an impaired mitotic checkpoint.
Alterations in the mitotic spindle checkpoint in H/RS cells. (A) Analysis of centrosomes in tissue sections from HL tumors. Immunofluorescence staining for pericentrin-2 (red) and CD30 (green) revealed structural and numeric aberrations in H/RS cells. Images were obtained with a TCS-SP2-AOBS-UV confocal microscope equipped with a PL-APO 100 ×/1.40-0.70 oil-immersion objective lens and LCS software (Leica Microsystems, Bannockburn, IL). (B) Cell-cycle profiles of HL-derived cell lines and lymphoblastoid B cells (PBL-B) treated with nocodazole. (C) Quantification of the percentage of apoptotic and hyper-G2/M cells in panel B. Lymphoblastoid cells displayed a normal response to nocodazole (mitotic arrest preceding massive apoptosis), whereas HL-derived cell lines had a lower apoptotic index and higher hyper-G2/M fraction at late time points. (D) Mitotic index after nocodazole treatment. HL-derived cell lines arrest in mitosis less efficiently than lymphoblastoid cells, indicating an impaired mitotic checkpoint.
The second half of the genes are overexpressed by the neoplastic H/RS cells, as confirmed by immunohistochemical analyses, and comprises (1) genes related to signaling/apoptosis, in agreement with previous observations about the relationship between apoptosis regulation and clinical outcome in HL tumors8,9,28 ; and (2) cell-cycle regulatory genes, related mainly to mitosis, underlining the relationship between the regulation of the spindle checkpoint and chemoresistance.42 These findings are consistent with multiple previous observations performed in other tumor types. Thus, overexpression of MAD2L1, a component of the mitotic spindle checkpoint, causes mitotic defects leading to chromosome instability and aneuploidy and is correlated to poor prognosis in neuroblastoma.43 STK6 (Aurora A), a kinase implicated in spindle pole formation, is frequently amplified and/or overexpressed in epithelial malignancies, and STK6 amplification overrides the mitotic checkpoint and induces resistance to taxol.44 The checkpoint kinase CHEK1 is required for the DNA damage checkpoint and also participates in mitotic spindle formation; inhibition of CHEK1 or its chaperone HSP90 sensitizes various tumor cells to gemcitabine or cytarabine.45,46
Other genes that are overexpressed in treatment-resistant HL cases, but are not directly implicated in the mitotic checkpoint, have also been related to chemoresistance. RRM2 overexpression, which may result from gene amplification,47 is associated with resistance to gemcitabine in pancreatic adenocarcinoma cells, and suppression of RRM2 expression by RNA interference enhances the cytotoxicity of this drug.48 Amplification and/or overexpression of TYMS, the primary target for chemotherapeutic agents such as 5-fluorouracil, has oncogenic activity49 and is associated with chemotherapy resistance in colorectal cancer.50,51
In agreement with the results of the gene expression analysis, we have demonstrated the existence of a deficient mitotic checkpoint response in HL cell lines, which are thought to derive from chemoresistant H/RS cells. The importance of the deregulation of the mitotic checkpoint in H/RS cells is further suggested by several well-known features of this cellular population, such as morphologic abnormalities (presence of multinucleated cells), aneuploidy with complex karyotypes and frequent polyploidy,52,53 chromosomal instability,34,52 and centrosome alterations (Martín-Subero et al34 ; this report).
An additional link between the mitotic checkpoint and chemotherapy that is particularly relevant to our study was provided by Eom et al,54 who recently demonstrated that adriamycin can induce cell death through mitotic catastrophe by down-regulating several molecules with mitotic checkpoint function, most of which belong to our cell-cycle signature (eg, CHEK1, MAD2L1, CDC2, BUB1). What is clear is that there are connections between a weakened mitotic checkpoint, aneuploidy, and resistance to chemotherapy. New insights into the molecular links between the mitotic checkpoint and the apoptotic machinery are now needed for rational improvements to be made in the therapeutic targeting of mitosis. Notably, some of the genes that we found to be associated with outcome encode cell-cycle regulatory enzymes (such as STK6, CHEK1, or HSP90) that can be targeted with small molecule inhibitors. Moreover, some of these drugs are already available and are being tested in clinical trials for the treatment of different tumor types, which might accelerate the eventual evaluation of their efficacy for the treatment of HL.
In summary, we have described specific gene signatures associated with treatment response in patients with HL. Our results have identified (1) general processes affecting treatment response, such as specific immune responses and alterations of the spindle checkpoint; (2) potential prognostic biologic markers, as demonstrated by immunohistochemical techniques in an independent series of HL samples; and (3) potential therapeutic targets for the treatment of HL.
Appendix
The following centers and investigators participate in the Spanish Hodgkin Lymphoma Study Group: P. Domínguez, C. Jara (Fundación Hospital Alcorcón, Madrid, Spain); M. J. Mestre, R. Quibén, M. Méndez, L. Borbolla (Hospital de Móstoles, Madrid, Spain); M. A. Martínez, C. Grande (Hospital 12 de Octubre, Madrid, Spain); M. García-Cosío, C. Montalbán, J. García-Laraña (Hospital Ramón y Cajal, Madrid, Spain); C. Bellas, M. Provencio (Hospital Puerta de Hierro, Madrid, Spain); A. Castaño, P. Sánchez-Godoy (Hospital Severo Ochoa, Leganés, Madrid, Spain); C. Martín, R. Martínez, (Hospital Clínico Universitario San Carlos, Madrid, Spain); J. Menárguez, P. Sabín, E. Flores (Hospital Gregorio Marañón, Madrid, Spain); J. González-Carrero, C. Ponderós (Hospital Xeral-Cies, Vigo, Spain); T.Álvaro, L. Font (Hospital Verge de la Cinta, Tortosa, Spain); V. Romagosa, A. Fernández de Sevilla (Institut Catala d'Oncologia, Barcelona, Spain); M. Mollejo, M. A. Cruz (Hospital Virgen de la Salud, Toledo, Spain); H.Álvarez-Arguelles, M. Llanos (Hospital Universitario Canarias, Spain); C. Morante (Hospital Cabueñes, Gijón, Spain); F. Mazorra, E. Conde (Hospital Marqués de Valdecilla, Santander, Spain); M. F. Fresno, C. Rayón, C. Nicolás (Hospital Central de Asturias, Oviedo, Spain); T. Flores, R. García-Sanz (Hospital Universitario de Salamanca, Spain); J. Guma (Hospital Sant Joan, Reus, Spain); P. Gonzalvo (Hospital Comarcal de Jarrio, Coaña, Spain); G. Fernández (Hospital Alvarez Buyllas, Mieres, Spain); J. Forteza, M. Fraga, J. L. Bello (F Med Santiago de Compostela, Spain); J. R. Méndez (Hospital Valle de Nalón, Asturias, Spain); and J. F. García, M. M. Morente, and M. A. Piris (CNIO, Madrid, Spain).
Prepublished online as Blood First Edition Paper, March 21, 2006; DOI 10.1182/blood-2005-12-5125.
A complete list of members of the Spanish Hodgkin Lymphoma Study Group appears in “Appendix.”
Supported by the Fondo de Investigaciones Sanitarias (FIS, grants PI020323 and G03/179); the Comunidad Autónoma de Madrid (CAM, grant 08.1/0042.1/2003), Spain; and a fellowship from the CAM and the European Social Fund (A.S.-A.).
A.S.-A. and C.M. contributed equally to this article.
The online version of this article contains a data supplement.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 U.S.C. section 1734.
We are indebted to Dr U. Knippschild (Department of Surgery, Universitätsklinikum, Ulm, Germany) for his kind gift of pericentrin-2 antibody and to Ana Díez, Raquel Pajares, and M. Jesús Acuña for their technical assistance with immunohistochemical techniques and TMA construction. We also thank Irene Cuenca, Laura Cereceda, and Cesareo Corbacho at the CNIO Tumor Bank for collecting the human tumor samples and for their excellent assistance with data management.


This feature is available to Subscribers Only
Sign In or Create an Account Close Modal