Sometimes a title says it all. But not always. Therefore, we would encourage the readers of Blood to go beyond the title of the paper by de Fost et al, “Superior effects of high dose enzyme replacement therapy in type 1 Gaucher disease on bone marrow involvement and chitotriosidase levels: a 2-center retrospective analysis.”1
For many years now, we have urged our colleagues to use small doses of enzyme in the treatment of patients with Gaucher disease.2 Our own investigations and exhaustive meta-analyses showed clearly that the clinical effect of 15 U/kg to 30 U/kg per month was indistinguishable from the much larger dose of 130 U/kg per month that is most commonly administered.3,4 Although small doses are often used outside the United States, within the United States our recommendations are only occasionally followed. Part of the reason that large doses are administered is that almost every article written on this topic avers that the administration of small doses is “controversial.” Now, moreover, we read that the high dose is, indeed, “superior”—at least in the title of the article. Were we wrong? Have we been misled in our thinking by the vagaries of meta-analysis, in which comparisons are, of necessity, made between groups that may not be strictly comparable? In the current issue of Blood, we now have a study that uses a more robust approach, the retrospective matching of patients. In fact, it is perhaps the best study to date in which high-dose and low-dose therapy have been compared in matched cases. And we read in the title, at least, that “superior” results are achieved with high doses. But read on—at least the abstract.
Here is a direct quote: “Improvement in hemoglobin, platelet count, and hepatosplenomegaly was not significantly different between both cohorts, whereas plasma chitotriosidase and bone marrow involvement by magnetic resonance imaging improved more quickly and was more pronounced in the higher-dosed group.” Although high-dose enzyme therapy did have a superior effect on 2 surrogates of the disease, it had no greater effect on the actual disease manifestations of the patients.
Thus, while the title implies that the high doses of enzyme replacement for Gaucher disease are, after all, superior to the low doses that we have recommended, the conclusions that the authors draw in the paper itself are quite the opposite: low-dose therapy had the same effect as high-dose therapy on all of the important clinical manifestations of the disease. The response of the blood hemoglobin concentration, platelet count, regression of spleen and liver, and the frequency of bone crises were the same. “Superiority” of the high dose, which costs about $400 000 more per year for a 70-kg patient, was limited to the response of 2 surrogate markers, serum chitotriosidase and MRI scanning of the marrow.
So let us look a little further at the surrogates and what they tell us. The fact that chitotriosidase levels decrease more rapidly with high-dose therapy than with low-dose therapy has been found in 2 other less well controlled studies,5,6 and the confirmation of this finding is welcome. The finding that marrow fat increases more rapidly with high-dose treatment is, as far as we know, a unique finding. But for the clinician the important question is whether these parameters measure disease severity in a meaningful way. While the authors suggest that they may, our experience and the published literature suggest otherwise.
Two studies have compared disease severity and chitotriosidase activity in untreated Gaucher disease. One of these reports a faint correlation (r = 0.351) between the severity score and the level of the enzyme.6 The other avers, “None of the markers correlated with the occurrence of the following complications of Gaucher disease: avascular necrosis, fragility fracture, osteoporosis, liver disease, polyclonal or clonal gammopathy.... Of the blood markers only ACE was associated with a severity score index.(37) Correction for multiple comparisons(43) abrogated the significance of this relationship.”7(p263) One must ask, then, whether a marker that does not correlate with severity of disease is to be taken so seriously that one gives a larger dose of enzyme to lower it more rapidly.
What about the MRI findings? What is their clinical significance? As Gaucher cells occupy the marrow, normal marrow fat is displaced, changing the MRI signal.8,9 When the Gaucher cells are cleared from the marrow by enzyme replacement therapy, fat returns to the marrow. It is perhaps ironic that the removal of Gaucher cells, which are lipid storage cells from the marrow, results in an increase in marrow fat. However, this is what happens, and a number of studies have shown that marrow fat, as measured by MRI, increases with enzyme replacement therapy. The question that has not been adequately addressed before is whether the rate of disappearance is proportional to the enzyme dose given. In an earlier study from the Dutch group10 there seemed to be no difference, but in the current larger comparative study, the return of fat to the marrow was considerably more rapid at high enzyme doses.
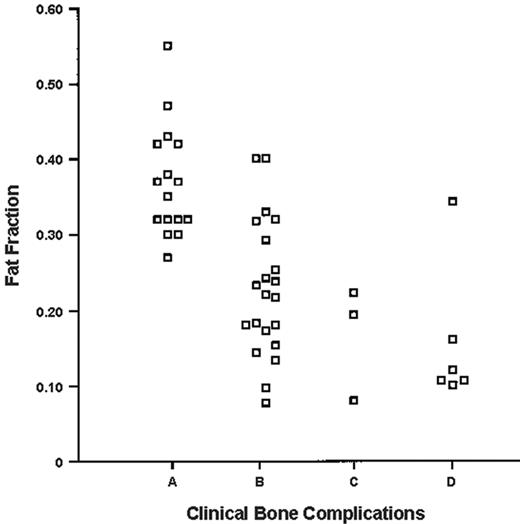
Again, we must ask, does it matter? Because the marrow resides within the skeleton, changes in bone marrow MRI are sometimes uncritically regarded as surrogates of skeletal disease. While there may be a relationship between marrow and skeletal lesions because of the intimate contact between them, this is by no means necessarily true. Indeed, in the present study both hematologic recovery (representing marrow function) and clinical bone disease were dose independent. Do the MRI measurements have any relationship to bone disease at all? de Fost et al state, “Fat fraction measurements of the lumbar spine... [show] a close correlation of the appearance of clinical complications,” citing one of their earlier studies,11 but as shown in Figure 1, which was taken from that publication, there is, in fact, scarcely any relationship at all.
So the conclusions to be drawn from this excellent clinical study are clear: more is not better. The fact that high-dose enzyme replacement therapy is “superior” when 2 surrogates of disease activity are measured should not influence our choice of treatment regimens. Would we prescribe an antileukemic drug really because it lowered the white count if it failed to decrease morbidity or increase lifespan? Of course not. Would we prescribe an anticholesterol drug that lowered the blood cholesterol level if it had no effect on lifespan or the incidence of heart attack or stroke? We wouldn't do that either. So why would we prescribe a very expensive treatment schedule that affected a serum marker and an MRI measurement that had no effect on the clinical course? As physicians, our concern must be the regression of organomegaly, development of clinically meaningful bone disease, and the correction of anemia and thrombocytopenia, when it exists. What de Fost et al have shown once again is that these important aims can be achieved and at a cost much lower than that of high-dose therapy. Physicians have the responsibility to be prudent in expending society's resources. This is a case where we really can make a difference.
Plot of distribution of fat fraction in relation to clinical bone complications. (A) Healthy. (B) Gaucher disease without complications. (C) Gaucher disease with mild complications. (D) Gaucher disease with severe complications. Reprinted with permission from the American Journal of Roentgenology.11
Plot of distribution of fat fraction in relation to clinical bone complications. (A) Healthy. (B) Gaucher disease without complications. (C) Gaucher disease with mild complications. (D) Gaucher disease with severe complications. Reprinted with permission from the American Journal of Roentgenology.11
Prepublished online as Blood First Edition Paper, April 25, 2006; DOI 10.1182/blood-2006-03-010801.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal