Abstract
The detection of a monoclonal immunoglobulin in serum or urine usually raises concerns about the size of the underlying B-cell-derived clone and possible systemic effects caused by its expansion. However, a small clone can synthesize a very toxic protein, producing devastating systemic damage and protean clinical presentations. The resulting “monoclonal component-related diseases,” although difficult to diagnose, may be progressive and even fatal. The monoclonal protein can aggregate and deposit systemically as occurs in light-chain amyloidosis, monoclonal immunoglobulin deposition disease, crystal-storing histiocytosis, and monoclonal cryoglobulinemia. Alternatively, some monoclonal proteins possess antibody activity toward autogenous antigens and cause chronic cold agglutinin disease, mixed cryoglobulinemia, and peripheral neuropathies. Other humoral mediators may contribute to neuropathy in variant disorders such as the POEMS (polyneuropathy, organomegaly, endocrinopathy, M protein, and skin changes) syndrome. The clone synthesizing the noxious monoclonal proteins is often small, and sensitive techniques may be required to detect these immunoglobulins. A delay in diagnosis can allow irreversible organ damage and dramatically shorten survival. Prompt recognition of suggestive signs and symptoms should trigger a thorough diagnostic approach to reach the correct diagnosis quickly, because this is the key to effective therapy. Although the treatment of these conditions is not optimal, significant advances have been made, improving the duration and quality of life.
Introduction
The presence of monoclonal immunoglobulin in serum or urine is relatively frequent, being detected in approximately 3% of the general adult population (> 50 years)1 and in up to 7% of subjects seeking medical evaluation.2 Thus, the finding of a monoclonal protein represents one of the most common laboratory abnormalities in adults and one of the most frequent causes for hematology consultation. The approach of hematologists to an individual with a monoclonal component is mainly guided by concerns regarding the size of the B-cell clone and its potential aggressiveness. Thus, the conditions usually considered in the differential diagnosis are neoplasias such as multiple myeloma and Waldenström macroglobulinemia and the relatively common and asymptomatic monoclonal gammopathy of undetermined significance (MGUS). However, even a small clone, as seen in MGUS, may synthesize a noxious monoclonal protein that can be responsible for devastating systemic organ damage dominating the clinical presentation, altering the natural history, and determining the prognosis (Figure 1). The monoclonal protein can cause severe organ damage and dysfunction through its aggregation and deposition or through its antibody activity versus autoantigens, defining the group of monoclonal component-related diseases (Table 1). It is of vital importance that hematologists recognize these syndromes promptly. Appropriate early treatment can alleviate symptoms and, more importantly, prevent irreversible organ damage and extend survival. This is particularly true for the diseases caused by monoclonal protein aggregation and deposition because these are characterized by progressive organ damage: the more time that passes between the onset of the diagnosis and treatment, the more organ dysfunction accumulates, ultimately reaching the point of no return. Thus, early diagnosis is imperative. The purpose of this article is to highlight the principal clinical features of these diseases and the diagnostic challenges they pose.
Most common monoclonal component-related diseases
Diseases caused by M-protein aggregation |
| Light chain-cast nephropathy |
| AL amyloidosis |
| Light chain-deposition disease |
| Crystal-storing histiocytosis: adult Fanconi syndrome |
| Cryoglobulinemia type I |
| Diseases caused by M-protein antibody activity |
| Mixed cryoglobulinemia type II |
| Monoclonal cold agglutinins |
| Polyneuropathies |
Diseases caused by M-protein aggregation |
| Light chain-cast nephropathy |
| AL amyloidosis |
| Light chain-deposition disease |
| Crystal-storing histiocytosis: adult Fanconi syndrome |
| Cryoglobulinemia type I |
| Diseases caused by M-protein antibody activity |
| Mixed cryoglobulinemia type II |
| Monoclonal cold agglutinins |
| Polyneuropathies |
Diseases caused by the aggregation of monoclonal proteins
The monoclonal protein can aggregate, forming (1) amyloid fibrils, causing light-chain amyloidosis (AL); (2) amorphous punctate aggregates, as observed in monoclonal immunoglobulin deposition disease; (3) crystals, as in crystal-storing histiocytosis with involvement of the kidney proximal tubular cells resulting in acquired Fanconi syndrome; (4) microtubules causing vascular obstruction in small vessels in type I cryoglobulinemia. The urinary monoclonal light chain (Bence Jones protein) can interact specifically with the Tamm-Horsfall protein and precipitate in the distal tubules of the kidney, forming obstructive casts and causing so-called light-chain cast nephropathy.3 This condition, also known as “myeloma kidney,” is a common cause of renal failure in high-mass myeloma and is not discussed here.
Light-chain (primary) amyloidosis
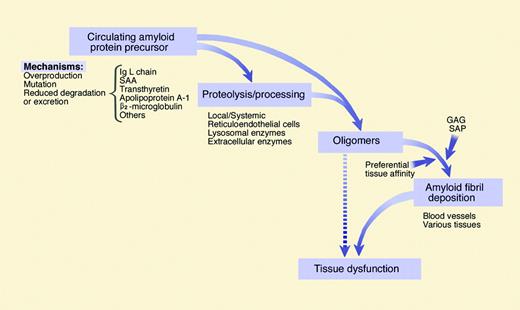
Molecular mechanisms. Amyloidosis is a protein misfolding disorder in which soluble proteins aggregate as extracellular insoluble amyloid fibrils, causing functional and structural organ damage.4 Amyloidosis is a generic term for a final common pathway of protein deposition in tissues (Figure 2).4,5 At least 24 different proteins can form amyloid deposits that may be localized or systemic, leading to pitfalls in the differential diagnosis. In AL amyloidosis the fibrils are formed by the N-terminal fragment of a monoclonal immunoglobulin light chain (LC) comprising the variable region and a portion of the constant region. There are anecdotal reports of amyloidosis caused by the deposition of γ or μ heavy-chain variable region fragments, possibly associated with the third constant domain (CH3), constituting heavy-chain amyloidosis (AH).6 Typically, the amyloid plasma cell clone infiltrates the bone marrow to a modest extent (median bone marrow plasma cell percentage, 7%).7 AL is characterized by low or undetectable plasma cell proliferation,8 and transformation to overt myeloma occurs infrequently. Only a small proportion of free monoclonal LCs form amyloid fibrils in vivo. Thus, the ability to form amyloid is probably related to individual structural characteristics of the LC variable region. Unlike most other plasma cell dyscrasias, the λ LC isotype is prevalent in AL (κ/λ ratio, 1:3), suggesting the existence of amyloid-associated Vλ germ line genes. Indeed, substantial overexpression of the Vλ6a and Vλ3r gene segments accounts for this phenomenon.9 For amyloid κ LC, the gene families VκI and VκIV appear to be more frequently rearranged in AL.10 The relationship between LC gene usage, somatic mutations, and amyloidogenicity has been reviewed.7,11
M-component-related diseases. In B-cell neoplasias (MM indicates multiple myeloma; WM, Waldenström macroglobulinemia; NHL, non-Hodgkin lymphoma; and CLL, chronic lymphocytic leukemia) the clinical pattern is usually dominated by systemic effects caused by expansion of the malignant clone, whereas the monoclonal protein may cause hyperviscosity syndrome or kidney damage. In less common disorders, the biologic effects of the monoclonal protein may account for most of the clinical manifestations and determine the prognosis. There are overlaps between these 2 groups; for instance, the IgM of a patient with Waldenström macroglobulinemia may have a cold agglutinin activity and a myeloma clone can secrete an amyloidogenic light chain. The left micrograph depicts myeloma bone marrow plasma cells stained with May-Grünwald-Giemsa; objective magnification, 100× (numeric aperture [NA] 1.30). The right micrograph depicts AL amyloidosis bone marrow plasma cells observed in immunofluorescence, using TRITC-conjugated anti-human lambda light chain antiserum from rabbit (Dako, Glostrup, Denmark), under a Nikon Eclipse E600 microscope (Nikon, Tokyo, Japan) equipped with a Nikon Pan Fluor 40×/0.75 NA objective. Image was photographed using a Leica DFC 480 camera (Leica Microsystems, Wetzlar, Germany), and was acquired using Leica IM50 Image Manager software. Illustration by Marie Dauenheimer.
M-component-related diseases. In B-cell neoplasias (MM indicates multiple myeloma; WM, Waldenström macroglobulinemia; NHL, non-Hodgkin lymphoma; and CLL, chronic lymphocytic leukemia) the clinical pattern is usually dominated by systemic effects caused by expansion of the malignant clone, whereas the monoclonal protein may cause hyperviscosity syndrome or kidney damage. In less common disorders, the biologic effects of the monoclonal protein may account for most of the clinical manifestations and determine the prognosis. There are overlaps between these 2 groups; for instance, the IgM of a patient with Waldenström macroglobulinemia may have a cold agglutinin activity and a myeloma clone can secrete an amyloidogenic light chain. The left micrograph depicts myeloma bone marrow plasma cells stained with May-Grünwald-Giemsa; objective magnification, 100× (numeric aperture [NA] 1.30). The right micrograph depicts AL amyloidosis bone marrow plasma cells observed in immunofluorescence, using TRITC-conjugated anti-human lambda light chain antiserum from rabbit (Dako, Glostrup, Denmark), under a Nikon Eclipse E600 microscope (Nikon, Tokyo, Japan) equipped with a Nikon Pan Fluor 40×/0.75 NA objective. Image was photographed using a Leica DFC 480 camera (Leica Microsystems, Wetzlar, Germany), and was acquired using Leica IM50 Image Manager software. Illustration by Marie Dauenheimer.
The molecular basis underlying the tissue localization of the deposits, with prevalent involvement of the heart, kidney, liver, or other organs, is one of the major unsolved issues in amyloid research. Elucidation of the molecular mechanisms involved in tissue targeting may lead to the development of innovative therapeutic agents. As first reported by Comenzo et al,12 LCs derived from the λ6a germ line gene are preferentially associated with kidney involvement possibly through receptor-mediated interactions with mesangial cells.13 Recognition of specific epitopes by LC dimers retaining antibody-binding activity14 can also play a role in tissue specificity.
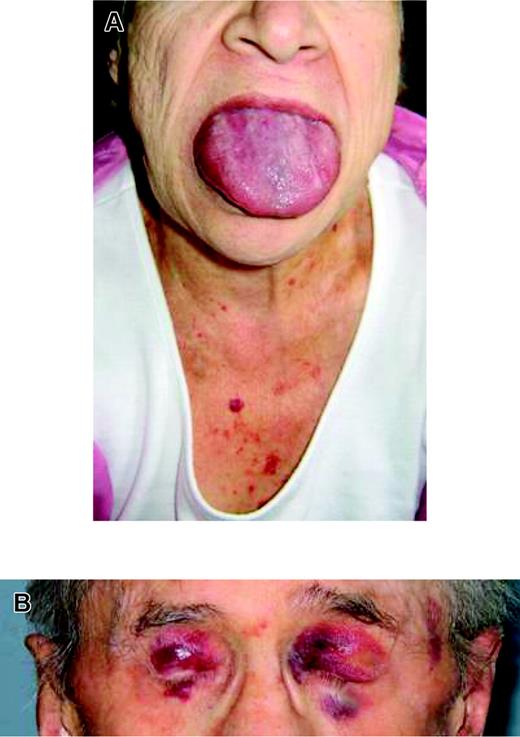
Clinical presentation. AL is the most common form of symptomatic systemic amyloidosis in western countries, with an estimated incidence of 0.8 per 100 000 person-years.15 The median age at diagnosis is about 60 years, with male preponderance (57%).16,17 AL amyloidosis is a systemic, progressive condition, and approximately 70% of patients present with 2 or more organs involved. The clinical manifestations of systemic AL are protean and depend on the organ system predominantly involved. Vague symptoms include fatigue, edema, and weight loss. Highly suggestive physical findings include tongue enlargement, periorbital purpura (Figure 3), and periarticular amyloid infiltration, although these occur collectively in only approximately 15% of patients.18 The organs most often involved are the kidney (74%), heart (60%), liver (27%), peripheral nervous system (22%), and autonomic nervous system (18%).17 Nephrotic syndrome is present in 50% and renal failure in 18% of patients. Heart involvement, usually manifested by congestive heart failure (> NYHA class II), arrhythmias, or both, is present in 37% of patients. Liver involvement most often manifests as palpable hepatomegaly with increased concentrations of serum alkaline phosphatase. Spleen involvement may result in the paradoxic findings of splenomegaly and functional hyposplenism with Howell-Jolly bodies present on a peripheral blood smear. Neuropathy can be axonal and demyelinating, starting with sensory symptoms in the lower extremities and progressing to motor changes and the upper extremities.18 Autonomic neuropathy can involve the upper gastrointestinal tract with pseudo-obstruction and vomiting and the lower tract with diarrhea or constipation.19 Postural hypotension, syncope, and impotence can also occur. Criteria for defining AL organ involvement and treatment response were recently defined by a consensus panel.20 Cardiac involvement is usually evaluated and monitored using echocardiography.21 Recently, 2 easily accessible and reproducible serum biomarkers, the N-terminal fragment of natriuretic peptide type B (NT-proBNP) and troponin T, were shown to reflect the myocardial dysfunction produced by AL. These biomarkers are useful for patient stratification and are powerful predictors of survival.22,23
The general mechanisms involved in amyloid formation. The amyloidogenic protein can be synthesized in excess and persist in serum at high concentrations, as for monoclonal light chains or the acute-phase protein serum amyloid A (SAA), or can reach high serum concentrations because of reduced clearance, such as β2-microglobulin in chronic hemodialysis, or can be mutated as in hereditary amyloidosis. Certain proteins with intrinsic amyloidogenic properties, such as transthyretin, can cause amyloidosis late in life, as in senile systemic amyloidosis. Some of these proteins undergo a proteolytic remodeling that facilitates polymerization. The early protein aggregates can exert a direct cytotoxic effect. However, the role of early aggregates/oligomers has not yet been defined in all types of amyloidosis. The concurrence of tissue components and common constituents, such as glycosaminoglycans (GAGs) and serum amyloid P (SAP) component favors formation and persistence of tissue deposits of amyloid fibrils which contribute to causing the dysfunction of the target organ. Illustration by Marie Dauenheimer, adapted from Stone.5
The general mechanisms involved in amyloid formation. The amyloidogenic protein can be synthesized in excess and persist in serum at high concentrations, as for monoclonal light chains or the acute-phase protein serum amyloid A (SAA), or can reach high serum concentrations because of reduced clearance, such as β2-microglobulin in chronic hemodialysis, or can be mutated as in hereditary amyloidosis. Certain proteins with intrinsic amyloidogenic properties, such as transthyretin, can cause amyloidosis late in life, as in senile systemic amyloidosis. Some of these proteins undergo a proteolytic remodeling that facilitates polymerization. The early protein aggregates can exert a direct cytotoxic effect. However, the role of early aggregates/oligomers has not yet been defined in all types of amyloidosis. The concurrence of tissue components and common constituents, such as glycosaminoglycans (GAGs) and serum amyloid P (SAP) component favors formation and persistence of tissue deposits of amyloid fibrils which contribute to causing the dysfunction of the target organ. Illustration by Marie Dauenheimer, adapted from Stone.5
Localized AL is an intriguing condition characterized by limited growth of monoclonal plasma cells and restriction of amyloid deposits to sites adjacent to those of the synthesis of the precursor. Although local evolution can be life threatening, the risk of developing a systemic disease is negligible.24
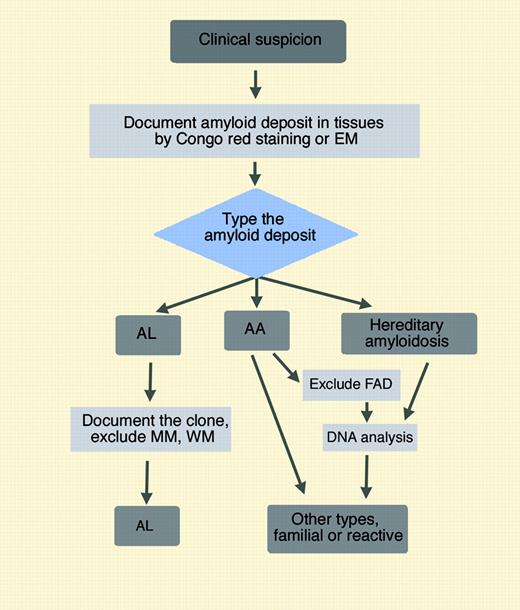
Diagnosis. Early diagnosis and unequivocal typing of the amyloid deposits are of vital importance. Early diagnosis depends on the level of alertness of the hematologist: any patient with nephrotic-range proteinuria, unexplained nonischemic cardiomyopathy, peripheral neuropathy, unexplained hepatomegaly or functional hyposplenism, and autonomic neuropathy with weight loss should be screened for amyloidosis.25 The diagnosis of AL is biopsy based and requires the presence of deposits with apple-green birefringence after Congo red staining, or the prototypic, nonbranching, 10-nm diameter fibrillar structures by electron microscopy. Fine-needle aspiration of abdominal fat is innocuous, fast, inexpensive, and sensitive (87%).17 If negative, the second-choice biopsy site at the Pavia Amyloid Center is the minor labial salivary glands. Renal and hepatic biopsies carry a small risk of bleeding and often require overnight hospitalization.26 Once the diagnosis of amyloidosis has been established histologically, the type must be determined. The typing of systemic amyloidoses involves a careful clinical evaluation associated with refined immunohistochemical/biochemical analyses and genetic testing (Figure 4). For biopsy-proven amyloidosis to be characterized as AL type, a plasma cell clone should be demonstrated.31 Screening serum electrophoresis is inadequate for this purpose because it does not show a M-spike in approximately 50% of patients. Therefore, all patients should undergo sensitive immunofixation electrophoresis of serum and urine which is able to detect a monoclonal component in up to 97% of patients.17 The quantification of serum-free light chain may complement immunofixation and is useful for monitoring response to therapy.32 The bone marrow should always be examined, bearing in mind that the absolute number of plasma cells may be within the normal range and that immunohistochemistry/immunofluorescence for κ and λ light chains may be necessary for detecting the small clonal population. Thus, we stress that an apparently normal bone marrow by routine morphology only should not be the basis for excluding the diagnosis of a potentially rapidly fatal disease, nor for withholding prompt, aggressive anticlone treatment.
Prototypic physical findings in AL. (A) A patient with macroglossia and purpura. Macroglossia is observed in 12% of patients with AL. (B) Periorbital purpura exacerbated by the Valsalva maneuver is seen in 6% of patients.
Prototypic physical findings in AL. (A) A patient with macroglossia and purpura. Macroglossia is observed in 12% of patients with AL. (B) Periorbital purpura exacerbated by the Valsalva maneuver is seen in 6% of patients.
Moreover, the possibility of a chance coexistence of a monoclonal protein in a patient with hereditary amyloidosis should always be considered in view of the relatively high prevalence of a monoclonal protein in the adult population.30,33 Mistyping of amyloidosis may have catastrophic therapeutic consequences, such as transplanting hematopoietic stem cells instead of liver. Clinically, it is difficult to distinguish AL from reactive, familial, and senile systemic forms of amyloidosis, because of their overlapping clinical presentations (Table 2) and the lack of an informative family history in half of the patients with hereditary amyloidosis. Immunohistochemistry is usually definitive in identifying or ruling out AA amyloidosis, but it is frequently not diagnostic with respect to AL amyloidosis.30 At the Pavia Amyloid Center, amyloid deposits are typed with the use of immunoelectron microscopy, which yields unequivocal results in virtually all patients.27 Genetic testing allows the identification of the specific mutation in the hereditary forms (see Figure 4 for details).
Clinical manifestations of some systemic amyloidoses
Site . | AL . | AA . | ATTR . | AApoAI . | AApoAII . | ALys . | AFib . | AGel . |
|---|---|---|---|---|---|---|---|---|
| Kidney | ++ | ++ | + | ++ | ++ | ++ | ++ | (+) |
| Heart | ++ | (+) | ++ | ++ | + | – | – | (+) |
| PNS | + | – | ++ | + | – | – | – | ++ |
| ANS | + | + | ++ | – | – | – | – | (+) |
| Liver/spleen | + | + | – | ++ | – | ++ | (+) | – |
| GI | + | + | – | – | – | + | – | – |
| CNS | – | – | +* | – | – | – | – | – |
| Skin | + | – | – | + | – | + | – | ++ |
| Eye | – | – | ++ | – | – | – | – | ++ |
| Testis | – | + | – | ++ | – | – | – | – |
Site . | AL . | AA . | ATTR . | AApoAI . | AApoAII . | ALys . | AFib . | AGel . |
|---|---|---|---|---|---|---|---|---|
| Kidney | ++ | ++ | + | ++ | ++ | ++ | ++ | (+) |
| Heart | ++ | (+) | ++ | ++ | + | – | – | (+) |
| PNS | + | – | ++ | + | – | – | – | ++ |
| ANS | + | + | ++ | – | – | – | – | (+) |
| Liver/spleen | + | + | – | ++ | – | ++ | (+) | – |
| GI | + | + | – | – | – | + | – | – |
| CNS | – | – | +* | – | – | – | – | – |
| Skin | + | – | – | + | – | + | – | ++ |
| Eye | – | – | ++ | – | – | – | – | ++ |
| Testis | – | + | – | ++ | – | – | – | – |
AA indicates reactive amyloidosis; ATTR, transthyretin familial amyloidosis; AApoAI, apolipoprotein-AI familial amyloidosis; AApoAII, apolipoprotein-AII familial amyloidosis; ALys, lysozyme familial amyloidosis; AFib, fibrinogen familial amyloidosis; AGel, gelsolin familial amyloidosis; PNS, peripheral nervous system; ANS, autonomic nervous system; GI, gastrointestinal tract; CNS, central nervous system; ++, common; +, observed in a minority of patients; (+), observed rarely; –, not observed
Leptomeningeal
Flow chart for typing amyloidoses. The crucial division is made from typing the amyloid deposits. This can be accomplished with immunohistochemistry or immunoelectron microscopy27 or by biochemical methods which are applicable also to formalin-fixed tissue samples.28 If a variant protein is identified, the specific mutation can be rapidly detected by DNA analysis. Genetic testing is also necessary for the diagnosis of familial autoinflammatory diseases (FADs) causing reactive amyloidosis (AA) in patients with characteristic clinical features.29 Immunohistochemistry is usually reliable for identifying or ruling out AA amyloidosis but is frequently not diagnostic with respect to AL amyloidosis.30 Immunoelectron microscopy (EM) and biochemical methods provide definitive results; however, they are labor intensive and require expertise. If these techniques are not available, the DNA analysis should be performed upfront to exclude the hereditary amyloidoses whose clinical presentation is consistent with the patient's manifestations. Illustration by Marie Dauenheimer.
Flow chart for typing amyloidoses. The crucial division is made from typing the amyloid deposits. This can be accomplished with immunohistochemistry or immunoelectron microscopy27 or by biochemical methods which are applicable also to formalin-fixed tissue samples.28 If a variant protein is identified, the specific mutation can be rapidly detected by DNA analysis. Genetic testing is also necessary for the diagnosis of familial autoinflammatory diseases (FADs) causing reactive amyloidosis (AA) in patients with characteristic clinical features.29 Immunohistochemistry is usually reliable for identifying or ruling out AA amyloidosis but is frequently not diagnostic with respect to AL amyloidosis.30 Immunoelectron microscopy (EM) and biochemical methods provide definitive results; however, they are labor intensive and require expertise. If these techniques are not available, the DNA analysis should be performed upfront to exclude the hereditary amyloidoses whose clinical presentation is consistent with the patient's manifestations. Illustration by Marie Dauenheimer.
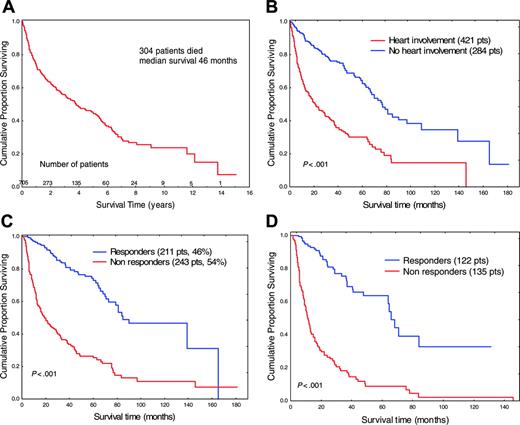
Prognosis. The median survival of patients with AL ranges from approximately 2 years to 3.8 years, depending in part on the treatment center and the nature of referral patterns.34 The median survival of 705 patients with AL followed in Pavia is 46 months (Figure 5A). Most patients with AL (76% in our patient population) die of cardiac complications, either congestive heart failure or sudden death. Median survival of patients with heart involvement was significantly shorter than that of patients without cardiac amyloidosis (Figure 5B), and patients who obtained a hematologic response to chemotherapy survived longer than other patients (Figure 5C).17 Cox multivariate analysis confirmed that the only 2 significant independent prognostic factors were response to therapy (protective) and cardiac involvement. Note that hematologic response translated into a significant survival benefit also in patients with cardiac involvement (Figure 5D).
Therapy. Once the diagnosis of AL has been firmly established, treatment should be tailored according to the age of the patient and the systemic damage caused by the amyloid process which renders this group of patients fragile and sensitive to treatment toxicity. The aims of treatment in AL amyloidosis are to reduce the supply of the amyloidogenic monoclonal LC rapidly and to restore organ function. The achievement of these 2 goals can be closely monitored by quantifying the amyloidogenic LC and a biomarker of heart function, NT-proBNP. It has been shown that a greater than 50% reduction of the circulating amyloidogenic LC translates into a reduction of amyloid load and extended survival,35 although in patients undergoing peripheral blood stem cell transplantation (PBSCT) it was not the percentage of reduction in free LC that predicted survival, but rather the absolute level of free LC achieved after therapy. Normalization of free LC levels after PBSCT predicted both complete hematologic response and organ response.36 NT-proBNP is a sensitive marker of amyloid heart dysfunction.22 Its concentration drops rapidly if the reduction of the concentration of LC is adequate.37 This allows titration of the anticlone treatment, improving the risk-benefit ratio and allowing a prompt change of therapy in the case of an inadequate response. Evidence of progression or regression of amyloid deposits can be obtained from SAP scintigraphy.38
Intravenous administration of high doses of the alkylating agent melphalan followed by PBSCT is considered the most effective treatment for selected patients with AL, with a response rate ranging from 50% to 60% together with a significant extension of survival. However, PBSCT is associated with a relatively high treatment-related mortality (the current rate being 13%-14%), particularly in patients with heart failure and multiorgan involvement.39,40 A risk-adapted approach has been proposed to modulate the dosage of melphalan according to the patient's age and organ involvement.41 However, risk-adjusted adaptation of the melphalan dose before stem cell transplantation is associated with a lower response rate.39,40 Dexamethasone-based regimens are also effective (reviewed in Merlini42 ). Dexamethasone alone provided a hematologic response in 53% of patients, but it still had substantial toxicity, with a 7% treatment-related mortality rate.43 The addition of oral melphalan to dexamethasone (M-Dex) provided a rapid response (median, 4.5 months) in 67% of patients with AL ineligible for PBSCT because of advanced disease, with a treatment-related mortality rate of 4%.44 The M-Dex regimen is a viable alternative to stem cell transplantation according to the results of a French phase 3 trial comparing PBSCT and the oral M-Dex regimen in AL. The trial showed that PBSCT was not superior to M-Dex in a multicenter setting and was associated with lower survival when patients were treated in centers without great experience.45 Thalidomide is poorly tolerated in patients with AL.42 However, its association with intermediate-dose dexamethasone (T-Dex) provided a clonal response in 48% of patients in a median time of 3.6 months. Severe adverse events related to T-Dex were frequent (65%), but no treatment-related deaths occurred.46 The thalidomide analog lenalidomide and the proteasome inhibitor bortezomib, both active in multiple myeloma, represent attractive but still experimental alternatives in the treatment of AL. Although the optimal treatment of AL remains uncertain, the therapeutic armamentarium is growing, and the availability of sensitive markers of clonal activity and organ damage allows more effective use of therapeutic resources. Supportive therapy is of paramount importance for gaining time while specific therapy takes effect (reviewed in Merlini42 ). Heart47 or kidney transplantation48 followed by PBSCT has been successfully applied in selected patients.
Survival in AL. (A) Overall survival of 705 patients with AL followed at the Pavia Amyloid Center. (B) Survival according to heart involvement. (C) Survival according to response to chemotherapy in 454 patients. (D) Survival according to response to chemotherapy in 257 patients with heart involvement. There was no significant difference in either echocardiographic features or in the serum concentration of the cardiac biomarker NT-proBNP in nonresponders (median, 3952 ng/L; range, 96-56 764 ng/L) and responders (median, 3490 ng/L; range, 386-76 927 ng/L), respectively.
Survival in AL. (A) Overall survival of 705 patients with AL followed at the Pavia Amyloid Center. (B) Survival according to heart involvement. (C) Survival according to response to chemotherapy in 454 patients. (D) Survival according to response to chemotherapy in 257 patients with heart involvement. There was no significant difference in either echocardiographic features or in the serum concentration of the cardiac biomarker NT-proBNP in nonresponders (median, 3952 ng/L; range, 96-56 764 ng/L) and responders (median, 3490 ng/L; range, 386-76 927 ng/L), respectively.
Monoclonal immunoglobulin deposition disease
Nonamyloidotic monoclonal immunoglobulin deposition disease includes 3 rare entities: light-chain deposition disease (LCDD), light- and heavy-chain deposition disease (LHCDD), and heavy-chain deposition disease (HCDD). The clinical features, immunopathology, and molecular mechanisms of these diseases have been reviewed.49,50
The LC is κ in the vast majority of the patients, and the deposits are Congo red negative, amorphous, and electron dense. As expected, the primary structure of the LC is the main determinant of their deposition in tissues also in LCDD, as suggested by data obtained in animal models.51,52 Analysis of the primary structures of LCDD-related κ LC showed unusual hydrophobic residues exposed to the solvent in CDR1 or CDR3 regions.53 The mesangial cells play a pivotal role in the pathogenesis of renal damage also in LCDD,13 with de novo expression of mesangial matrix components.54
Although AL amyloidosis and LCDD have several features in common, both being diseases caused by LC deposition, they are clinically distinct. Although LCDD is frequently associated with multiple myeloma (in 65% of cases in a recently reported large LCDD population),55 only one tenth to one fifth of AL is associated with clinically overt myeloma. The kidney is the organ most frequently involved in both conditions: in nearly all patients (96%) with LCDD and in approximately 75% of patients with AL. Renal function is more severely compromised in LCDD than in AL, with almost all cases of LCDD having renal insufficiency at presentation. Urinary protein excretion is important in both conditions, exceeding 3.5 g/d in 53% and 40% of patients with AL and LCDD, respectively.17,55 Albumin is the predominant component present in urine, but the monoclonal LC is usually detectable as well. Symptomatic extrarenal deposition in patients with LCDD is uncommon and involves the heart (21%), liver (19%), and peripheral nervous system (8%).55 The cardiac involvement produces clinical and echocardiographic findings similar to those of amyloid cardiomyopathy.56
LCDD should be suspected in patients with multiple myeloma or in patients with serum or urinary monoclonal proteins in the presence of progressive (acute or chronic) renal insufficiency, associated with proteinuria. LCDD is usually diagnosed by renal biopsy using fluorescent anti-LC antibodies and electron microscopy.55 Multiple patterns of monoclonal protein deposition frequently coexist, including myeloma cast nephropathy and AL amyloidosis. In particular, both fibrillar (amyloid) and nonfibrillar monoclonal LC deposits may coexist in the same patient, and the identity of the amino acid sequence of the deposited protein has been reported.57 Monoclonal protein is detected by immunofixation in serum or urine in 94% of patients with LCDD with marked preponderance of κ chains.55
In rare cases, the deposits may be formed by heavy chain (HC) instead of LC constituting the so-called heavy-chain deposition disease (HCDD).58 The predominant HC class is γ, but cases of α and μ HCs have also been reported. Although these HCs have a deletion of the CH1 domain, this deletion seems necessary but not sufficient for deposition, because VH probably also contributes to tissue deposition.59 The clinical features of HCDD include significant proteinuria, microhematuria, and hypertension, and the disease usually has an ominous course. Isolated cases of combined deposition of LC and HC (light- and heavy-chain deposition disease, LHCDD) have been reported.60,61
The overall survival of patients with AL and LCDD is similar, the median value being 46 and 49 months, respectively; 24% of AL and 31% of patients with LCDD are alive at 8 years.17,55 Death in patients with LCDD is due to cachexia (44%) and heart involvement (11%). Survival is correlated to age, the presence of multiple myeloma, and extrarenal LC deposition.55
Major therapeutic efforts have been directed toward reducing the synthesis of the monoclonal proteins, using the same chemotherapeutic regimens as those used in multiple myeloma but with modest benefit.55,62 PBSCT is safe and produces durable hematologic responses, regression of LC deposits, and improvement in renal function and should be offered to young patients.63 Kidney transplantation is not an option for patients with LCDD unless measures have been taken to reduce light-chain production.64
Crystal-storing histiocytosis: adult Fanconi syndrome
Crystal-storing histiocytosis, an intralysosomal accumulation of monoclonal light chains that aggregate in crystals, is observed in association with both plasma cell and lymphoid disorders.65,66 The type of LC involved is almost exclusively κ, although there is not a consistent association with a particular heavy chain. Crystals can form in either histiocytes in soft tissues or parenchymal cells in bone marrow, lymph nodes, spleen, liver, stomach, adrenal glands, renal proximal tubules, and thyroid follicles. The initial clinical presentation depends on the site of crystal formation and is, therefore, varied. Some patients present with soft tissue masses in which predominantly histiocytes, but also fibroblastic cells, contain crystals. The crystal formation in renal proximal tubules is at the basis of adult Fanconi syndrome (FS).
Almost all κ LCs in patients with FS belong to the Vκ1 subgroup and derive from 2 germ line genes, O2/O12 or O8/O18.67 The pathogenic effect of FS light chains can be ascribed to a peculiar structure of the Vκ domain. Unlike other monoclonal LCs, which, after endocytosis, are degraded in the lysosomal compartment of proximal tubular cells, LCs from patients with FS are usually resistant to proteolysis and form organized crystals in the endocytic compartment of proximal tubule cells.68 However, as recently suggested, the molecular characteristics of κ LCs in FS are probably more heterogeneous.69
The clinical and pathologic features of LC-associated FS are heterogeneous. Typically, but with notable exceptions, FS occurs in patients with smoldering myeloma or precedes the development of overt myeloma (Figure 6).70,71 Less frequently, FS may be observed in the setting of high-tumor mass myeloma with typical cast nephropathy and may or may not be associated with crystals in proximal tubules.72 Principal laboratory abnormalities include aminoaciduria, renal glycosuria, hypophosphatemia, hyperchloremic metabolic acidosis, hypokalemia, proteinuria of tubular origin, and hypouricemia. The major manifestations include osteomalacia, polyuria, chronic acidosis, and episodes of dehydration. FS frequently evolves into renal failure.
It has been shown in an animal model of FS that the morphologic alterations of the proximal tubule are reversible following suppression of the synthesis of LCs.73 This finding, together with the frequent evolution of FS into renal failure, suggests that patients with FS should be treated with chemotherapy to suppress the production of the nephrotoxic monoclonal LCs.
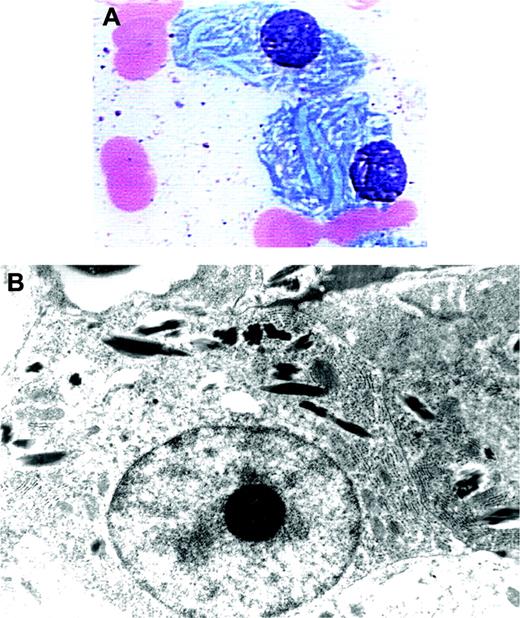
Crystalloid cytoplasmic inclusions in bone marrow plasma cells of a patient with Fanconi syndrome. A 70-year-old woman with indolent myeloma (IgGκ) developed mild renal failure. Bone marrow examination showed 17% plasmacytosis. The light microscopic (A) (Wright stain; original magnification, × 1000) and electron microscopic (B) (original magnification, × 13 680) photographs of marrow plasma cells displayed crescent-shaped cytoplasmic inclusions. The patient had low levels of serum bicarbonate and uric acid and elevated urine lysozyme (see Phillips et al70 ).
Crystalloid cytoplasmic inclusions in bone marrow plasma cells of a patient with Fanconi syndrome. A 70-year-old woman with indolent myeloma (IgGκ) developed mild renal failure. Bone marrow examination showed 17% plasmacytosis. The light microscopic (A) (Wright stain; original magnification, × 1000) and electron microscopic (B) (original magnification, × 13 680) photographs of marrow plasma cells displayed crescent-shaped cytoplasmic inclusions. The patient had low levels of serum bicarbonate and uric acid and elevated urine lysozyme (see Phillips et al70 ).
Type I cryoglobulinemia
Cryoglobulins are immunoglobulins that precipitate or gel reversibly at temperatures below 37°C. This temperature-sensitive precipitation has been reported in many disorders and usually indicates the presence of a monoclonal plasma cell dyscrasia, a circulating immune complex, or both. Type I cryoglobulins are rarely observed. They are composed of a monoclonal immunoglobulin, mainly IgG (IgG1 or IgG3) and occasionally IgM or IgA. Their solubility is often concentration dependent. Usually, they are reported in association with multiple myeloma or Waldenström macroglobulinemia. Presenting clinical features include cold sensitivity with Raynaud phenomenon, acrocyanosis, necrosis, purpura and ulcers of the extremities, cold urticaria, and renal insufficiency. The clinical manifestations are usually caused by capillary obstruction because of precipitation of the cryoprotein. Capillary obstruction can also occur in the kidney.74
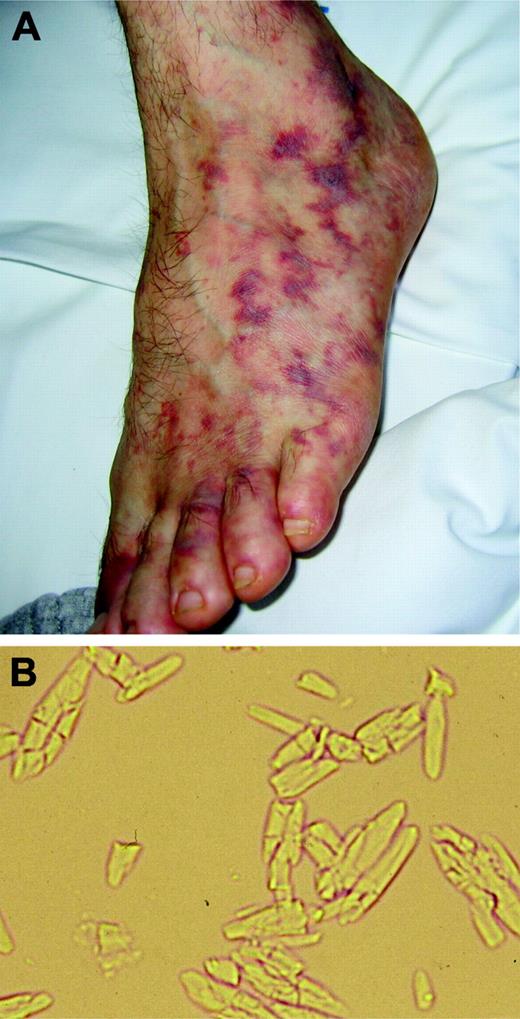
Rare forms of organized monoclonal immunoglobulin deposits related to type I cryoglobulins also include cryocrystalglobulinemia and so-called glomerulonephritis with organized microtubular monoclonal immunoglobulin deposits (GOMMID) (Table 3).75,76 These conditions are associated with various B-cell-derived immunoproliferative disorders, including chronic lymphocytic leukemia76 and multiple myeloma.77 The organized formations, crystals or microtubules, are present within the synthesizing B cells. In addition to kidney involvement, patients with cryocrystalglobulinemia may have systemic vasculopathy (Figure 7) and widespread erosive arthropathy, mimicking rheumatoid arthritis.75
Disorders related to monoclonal protein tissue deposition
Disease . | M-protein . | Ultrastructure . | Target organs/systems . | Association with MM or WM . | Sources . |
|---|---|---|---|---|---|
| Amyloidosis | κ/λ ratio, 1:3 | Fibrils (8-12 nm in diameter) | Kidney, heart, liver, PNS, ANS | 10%-20% | Kyle and Gertz,16 Obici et al17 |
| LCDD | κ/λ ratio, 3:1 | Amorphous | Kidney≫heart, liver, PNS | 40%-65% | Buxbaum and Gallo,49 Pozzi et al,55 Lin et al,61 Heliman et al62 |
| Crystal-storing histiocytosis | κ/λ ratio, 9:1 | Crystals (intracellular) | Kidney (adult Fanconi syndrome), BM, LN, liver, spleen and diverse additional sites | Frequently associated with smoldering MM or lymphomas | Lebeau et al,66 Messiaen et al72 |
| Cryoglobulinemia type I | IgG > IgM, IgA | Granular often with substructure | Vessels, kidney | Frequently associated with MM or WM | Karras et al74 |
| Cryocrystalglobulinemia | IgG | Crystals | Vessels, kidney, synovium | Various B-cell disorders, including MM | Papo et al,75 Ball et al77 |
| GOMMID* | Mostly IgG | Microtubules (20-60 nm) | Kidney | Frequently associated with CLL | Bridoux et al76 |
Disease . | M-protein . | Ultrastructure . | Target organs/systems . | Association with MM or WM . | Sources . |
|---|---|---|---|---|---|
| Amyloidosis | κ/λ ratio, 1:3 | Fibrils (8-12 nm in diameter) | Kidney, heart, liver, PNS, ANS | 10%-20% | Kyle and Gertz,16 Obici et al17 |
| LCDD | κ/λ ratio, 3:1 | Amorphous | Kidney≫heart, liver, PNS | 40%-65% | Buxbaum and Gallo,49 Pozzi et al,55 Lin et al,61 Heliman et al62 |
| Crystal-storing histiocytosis | κ/λ ratio, 9:1 | Crystals (intracellular) | Kidney (adult Fanconi syndrome), BM, LN, liver, spleen and diverse additional sites | Frequently associated with smoldering MM or lymphomas | Lebeau et al,66 Messiaen et al72 |
| Cryoglobulinemia type I | IgG > IgM, IgA | Granular often with substructure | Vessels, kidney | Frequently associated with MM or WM | Karras et al74 |
| Cryocrystalglobulinemia | IgG | Crystals | Vessels, kidney, synovium | Various B-cell disorders, including MM | Papo et al,75 Ball et al77 |
| GOMMID* | Mostly IgG | Microtubules (20-60 nm) | Kidney | Frequently associated with CLL | Bridoux et al76 |
MM indicates multiple myeloma; WM, Waldenström macroglobulinemia; GOMMID, glomerulonephritis with organized microtubular monoclonal immunoglobulin deposits; PNS, peripheral nervous system; ANS, autonomic nervous system; ≫, much more frequent than; BM, bone marrow; LN, lymph nodes; >, more frequent than; CLL, chronic lymphocytic leukemia
Cryoglobulins are sometimes, but not always, detectable in patients with GOMMID
Treatment is focused on the underlying B-cell neoplasia. Corticosteroids and removal of the monoclonal immunoglobulin by plasmapheresis produce prompt symptomatic relief while systemic therapy takes effect. Table 3 summarizes the pathologic and clinical features of the main diseases caused by the tissue deposition of monoclonal proteins in relation to their ultrastructural organization.
Features of cryocrystalglobulinemia. (A) Painful vasculitis produced by an IgGκ cryocrystalglobulin. Plasmapheresis rapidly resolved the vasculitis, and subsequent treatment with high-dose dexamethasone significantly reduced (by 70%) the concentration of the monoclonal IgGκ, leading to complete clinical remission. (B) Crystals formed after storing the serum at 4°C for 24 hours. Image was visualized using a Nikon Eclipse E600 microscope equipped with a Nikon Pan Fluor 20 ×/0.50 NA objective with no staining. Image was acquired using a Leica DFC 480 camera and Leica IM50 Image Manager software.
Features of cryocrystalglobulinemia. (A) Painful vasculitis produced by an IgGκ cryocrystalglobulin. Plasmapheresis rapidly resolved the vasculitis, and subsequent treatment with high-dose dexamethasone significantly reduced (by 70%) the concentration of the monoclonal IgGκ, leading to complete clinical remission. (B) Crystals formed after storing the serum at 4°C for 24 hours. Image was visualized using a Nikon Eclipse E600 microscope equipped with a Nikon Pan Fluor 20 ×/0.50 NA objective with no staining. Image was acquired using a Leica DFC 480 camera and Leica IM50 Image Manager software.
Autoantibody activity of monoclonal immunoglobulins
Some monoclonal proteins, in most cases IgM from patients with Waldenström macroglobulinemia or individuals with IgM MGUS, possess antigen-binding activity directed to autogenous or foreign antigens (Table 4).78-81 These monoclonal IgM autoantibodies include cold agglutinins, mixed cryoglobulins, and antineural components. In the absence of overt Waldenström macroglobulinemia these conditions are referred to as “IgM-related” disorders.82 Because of the antigen-antibody interaction, patients with these monoclonal autoimmune syndromes often present with hemolytic anemia, mixed cryoglobulinemia, or peripheral neuropathy at an earlier stage than patients with typical Waldenström macroglobulinemia who do not have evident antibody activity.79,83 The presence of monoclonal macroglobulin autoreactive antibodies thus influences the clinical presentation and natural history.
Some clinical manifestations and antigen specificities of human monoclonal IgM
Syndrome . | Autoantigen . | Possible foreign antigen . |
|---|---|---|
| Cold agglutinin immune hemolytic anemia | I/i red cell antigens | Bacterial lipopolysaccharides |
| Mixed cryoglobulinemia | IgG Fc | Hepatitis C virus |
| Peripheral neuropathies | Neural carbohydrate groups | Bacterial lipopolysaccharides |
Syndrome . | Autoantigen . | Possible foreign antigen . |
|---|---|---|
| Cold agglutinin immune hemolytic anemia | I/i red cell antigens | Bacterial lipopolysaccharides |
| Mixed cryoglobulinemia | IgG Fc | Hepatitis C virus |
| Peripheral neuropathies | Neural carbohydrate groups | Bacterial lipopolysaccharides |
Chronic cold agglutinin disease
Cold agglutinins (CAs) are human autoantibodies to red cell carbohydrate antigens. They are frequently found at a low titer in healthy adults. The vast majority are IgM proteins.79,80 Monoclonal CAs often have a high thermal amplitude, which contributes to their pathogenicity in causing complement-dependent immune hemolysis and cold sensitivity. The monoclonal CAs in chronic cold agglutinin disease differ from the lower-titer polyclonal IgM CAs associated with Mycoplasma pneumoniae and viral infections that can cause transient hemolytic anemia. Many patients with chronic cold agglutinin disease belong to the group of patients with IgM-related disorders, but some have clinically overt Waldenström macroglobulinemia. The VH4-34 gene segment is required to encode anti-I and anti-i specificities,84,85 and these antibodies share cross-idiotypic specificity. The same gene sequence has been found to encode bacterial antilipopolysaccharide reactivity, supporting the possibility that B cells containing this VH gene segment belong to the first line of defense against pathogens and are thus an integral part of the innate immune system. Regardless of their developmental pathway, monoclonal CAs clearly bind to autoantigens and cause disease. The IgM autoantibodies attach to red cells at temperatures that vary from patient to patient but may be close to 37°C. At temperatures below that threshold value, the IgM binds the red cell antigen and complement is fixed, causing subsequent intravascular hemolysis. Acrocyanosis and Raynaud phenomenon are commonly seen. The direct antiglobulin test is positive with anti-C3 and should be negative with anti-IgG. In vitro agglutination interferes with automatic blood cell counts, causing false increases in the mean corpuscular volume and false decreases in the red cell count. Treatment for CAs consists mainly of avoiding cold exposure. Rituximab is the only treatment showing acceptable response rates,86 although the effect may be transient.87
Type II mixed cryoglobulinemia
Type II mixed cryoglobulins (MCs) are monoclonal IgM complexed with polyclonal IgG. The monoclonal IgM is an autoantibody reacting with the FC portion of IgG (monoclonal rheumatoid factors).79-81 The cryoprecipitating property results from the size and limited solubility of the IgM-IgG immune complex. The systemic vasculitis that characterizes the disease appears to be caused by deposition of immune complexes on the walls of small vessels and subsequent activation of the complement cascade.
In the majority of patients, MCs are associated with hepatitis C virus (HCV) infection, which is considered the triggering factor of the disease.88,89 The virus is not directly oncogenic but infects hepatocytes and some B cells. Not all patients infected with HCV have MCs, but their presence correlates with duration of the hepatitis. The cryoprecipitable immune complexes contain HCV core proteins and specific anti-core IgG which are bound to IgM with rheumatoid factor activity. This large complex binds specifically to endothelial cells through the C1q receptor.90 The monoclonal IgM rheumatoid factors are generated by an antigen-driven process.91
HCV infection results in a spectrum of lymphoproliferative responses that are usually limited but become overtly malignant in about 10% of patients. Waldenström macroglobulinemia is the most frequent, but not the only, B-cell non-Hodgkin lymphoma associated with HCV and mixed cryoglobulinemia.92,93 Regression of splenic lymphoma and reduction in viremia with interferon treatment suggest some role for the virus in the pathogenesis of lymphoma.94
The clinical features of MCs are purpura, arthralgias, weakness, liver involvement, renal involvement (cryoglobulinemic glomerulonephritis), peripheral neuropathy, and widespread vasculitis. The severity of vasculitic manifestations has little relationship with the serum level of cryoglobulins (cryocrit) or complement. Thermal amplitude, the temperature at which the immune complex precipitates, appears to be more important.
Because HCV is the trigger to MCs in most patients, eradication of the viral infection is the main target of treatment. This is pursued using interferon-α either alone or with ribavirin. Inhibition of HCV replication is associated with a reduction of cryocrit and significant clinical improvement.95 Rituximab has been used successfully to target the B-cell clone specifically. The drug is safe and effective in most patients with MCs,96 although increased viremia was reported in responders.97 Symptoms may be alleviated by low-dose corticosteroids, and plasma exchange may be useful in active cryoglobulinemic nephropathy.
Neuropathies
Polyneuropathies are frequent in patients with monoclonal gammopathies, especially those with IgM MGUS or Waldenström macroglobulinemia. Some are autoimmune processes with the monoclonal macroglobulin having antibody activity to myelin or other neural components. Although compressive radiculopathy occurs in 5% of patients with myeloma, peripheral neuropathy is rare. Neuropathy can also occur in patients with amyloidosis, cryoglobulinemia, POEMS syndrome, and scleromyxedema.
In patients with IgM monoclonal protein and neuropathy at least 5 different carbohydrate antigenic targets have been identified associated with distinct clinical presentations: (1) myelin-associated glycoprotein (MAG): demyelinating sensorimotor neuropathy; (2) sulfatide: demyelinating predominantly sensory neuropathy; (3) GD1b ganglioside: demyelinating sensory neuropathy; (4) GM1 ganglioside: progressive lower-motor neuron syndrome, which is often asymmetric; and (5) the trisulfated heparin disaccharide: painful, predominantly sensory neuropathy with axon loss (reviewed in Stone et al79 and Kornberg and Pestronk98 ).
As with CAs and mixed cryoglobulins, microbial antigens may have a pathogenic role in some immune-mediated polyneuropathies (Table 4). Thus crossreactivity of human monoclonal IgM anti-GM1 antibodies with Campylobacter jejuni lipopolysaccharides has been reported in patients with Guillain-Barré syndrome.99
Most patients present with principally sensory complaints consisting of paresthesias, aching discomfort, dysesthesias, or lancinating pains. Imbalance and gait ataxia resulting from loss of proprioception occur commonly. Leg muscle atrophy may be present in advanced stages. Motor neuropathy is associated with antibody to GM1 ganglioside. Specific antibody reactivity (eg, anti-MAG) may be demonstrated serologically or on nerve biopsy.
It is imperative that neurologists and hematologists work together, especially in establishing the diagnosis and serially evaluating response to treatment (reviewed in Dispenzieri and Kyle100 and Levine et al101 ). The rate of progression and response to treatment vary widely.
Therapy is graduated according to the severity of the neuropathy. According to recently issued management guidelines for paraproteinemic demyelinating neuropathies,102 patients who have IgM demyelinating neuropathy without significant disability may require only symptomatic relief of tremor and paresthesias. In patients with significant disability or rapid worsening, high-dose intravenous immunoglobulin or plasma exchange should be considered as initial treatment, although their efficacy is unproven. For those patients with moderate or severe disability immunosuppressive treatment (with chlorambucil or cyclophosphamide in association with corticosteroids or, as reported anecdotally, with fludarabine, cladribine, PBSCT) should be considered, although long-term efficacy is unproven. Preliminary reports suggest that rituximab may be a promising therapeutic approach.102
Although most symptoms in patients with small clonal mass disorders are ascribed to the monoclonal protein, other humoral mediators may contribute to neuropathy in variant disorders such as the POEMS syndrome.
POEMS syndrome
This acronym derives from several dominant features of the syndrome (polyneuropathy, organomegaly, endocrinopathy, M-protein, and skin changes) which does, however, include other features such as sclerotic bone lesions, Castleman disease, thrombocytosis, polycythemia, papilledema, peripheral edema, ascites, clubbing, weight loss, and hyperhidrosis. This syndrome has been comprehensively reviewed.103,104 The minimum features required for diagnosis are peripheral neuropathy, osteosclerotic myeloma, or Castleman disease and at least one of the other features listed earlier.
The cause of POEMS syndrome is undetermined. The strikingly high frequency of λ light chain suggests a role of this protein although not related to its deposition. Antibodies to human herpes virus 8 are common.105 Although it has been known that these patients have increased blood concentrations of proinflammatory cytokines (IL-1β, TNF-α, and IL-6), attention has been focused on the more common high concentration of vascular endothelial growth factor (VEGF),106,107 possibly produced by plasma cells and platelets. VEGF promotes vascular permeability and angiogenesis and could account for organomegaly, edema, and skin lesions. The role of VEGF in the development of polyneuropathy is still unsettled.
The bone marrow plasma cell infiltration is modest (median, 5%), and the monoclonal protein (predominantly IgA), with virtually always a λ light chain, is usually small, frequently requiring immunofixation for its detection. The neuropathy dominates the clinical picture, resembles chronic inflammatory demyelinating polyneuropathy (CIDP), and is typically symmetric, motor, sensory, and autonomic. The diagnosis may be delayed by misdiagnosis of CIDP. Clues to an early diagnosis include thrombocytosis and sclerotic bone lesions. The mainstays of therapy are (1) irradiation of the osteosclerotic lesion, if solitary; (2) alkylator-based therapy, and (3) corticosteroids, which should be considered a temporary remedy. PBSCT is emerging as the most effective therapy, resulting in marked and sustained reduction of VEGF coincident with the clinical improvement.104,108
Scleromyxedema
Scleromyxedema is a rare progressive and disabling disease (only 114 cases were reviewed in 2001),109 characterized by a small IgGλ monoclonal protein, papular mucinous deposits of 2 to 3 mm in diameter, symmetric, and arranged in a linear array, most commonly located on the face, neck, upper trunk, forearm, and hands. With time the skin stiffens with reduced mobility of the mouth and joints, leading to a scleroderma-like appearance. Extracutaneous manifestations include upper gastrointestinal dysmotility, muscle weakness, joint contractures, sclerodactyly, carpal tunnel syndrome, and neurologic manifestations such as peripheral neuropathy, seizures, encephalopathy, psychosis, stroke, and coma. The pathogenic role of the monoclonal protein is undefined. Diagnosis relies on the presence of skin lesions with typical histologic features (dermal mucin deposits, fibroblast proliferation, and fibrosis),109 an IgGλ monoclonal protein, and absence of thyroid disorder. Congo red stain should be performed to rule out amyloidosis. There is no standard therapy for the systemic treatment of scleromyxedema. Corticosteroids and low-dose melphalan or cyclophosphamide produced variable results. Thalidomide has been reported to be effective in resistant cases. PBSCT led to complete resolution of most cutaneous and systemic symptoms in some patients with scleromyxedema,110 but its efficacy and safety need confirmation.
Conclusions
Small secretory B-cell clones which exert their noxious effects through the biologic activity of their monoclonal protein products are uncommon but pathogenic. Because of their low frequency and insidious clinical presentations, they are frequently overlooked. Clinical manifestations are protean. Any heart, kidney, or liver abnormality; the presence of dysautonomic symptoms with possible marked weight loss or peripheral neuropathy; or signs of systemic vasculitis in an individual with a monoclonal component should induce the hematologist to initiate a careful evaluation to detect these treacherous diseases. As a result of the systemic damage caused by toxic monoclonal proteins, the patient starts a diagnostic odyssey between various specialty physicians (eg nephrologists, cardiologists, neurologists, and gastroenterologists) who frequently seek advice and guidance from hematologists. It is vital not to miss the chance of diagnosing these diseases, because early recognition and appropriate treatment can prevent or reverse the organ damage, improve the quality of life, and significantly extend survival. Finally, the rarity of these conditions demands cooperation among hematologists to better define the natural history, perform controlled clinical trials, and improve the care of patients with these frequently subtle but clinically relevant diseases.
Prepublished online as Blood First Edition Paper, June 22, 2006; DOI 10.1182/blood-2006-03-001164.
Supported by the Italian Ministry of Health, Foundation IRCCS Policlinico San Matteo, Fondazione Cassa di Risparmio Province Lombarde (CARIPLO), and the Edward and Ruth Wilkof Foundation.

![Figure 1. M-component-related diseases. In B-cell neoplasias (MM indicates multiple myeloma; WM, Waldenström macroglobulinemia; NHL, non-Hodgkin lymphoma; and CLL, chronic lymphocytic leukemia) the clinical pattern is usually dominated by systemic effects caused by expansion of the malignant clone, whereas the monoclonal protein may cause hyperviscosity syndrome or kidney damage. In less common disorders, the biologic effects of the monoclonal protein may account for most of the clinical manifestations and determine the prognosis. There are overlaps between these 2 groups; for instance, the IgM of a patient with Waldenström macroglobulinemia may have a cold agglutinin activity and a myeloma clone can secrete an amyloidogenic light chain. The left micrograph depicts myeloma bone marrow plasma cells stained with May-Grünwald-Giemsa; objective magnification, 100× (numeric aperture [NA] 1.30). The right micrograph depicts AL amyloidosis bone marrow plasma cells observed in immunofluorescence, using TRITC-conjugated anti-human lambda light chain antiserum from rabbit (Dako, Glostrup, Denmark), under a Nikon Eclipse E600 microscope (Nikon, Tokyo, Japan) equipped with a Nikon Pan Fluor 40×/0.75 NA objective. Image was photographed using a Leica DFC 480 camera (Leica Microsystems, Wetzlar, Germany), and was acquired using Leica IM50 Image Manager software. Illustration by Marie Dauenheimer.](https://ash.silverchair-cdn.com/ash/content_public/journal/blood/108/8/10.1182_blood-2006-03-001164/4/m_zh80200602430001.jpeg?Expires=1767734456&Signature=OqLLVD4BGp7FQvrYUs35b2uJLAQr8XZnxzC2VukUxMm4~iqzr37d0-1oeFIGr-jmGXWo4FysuXmBvi3owfj3gJQ4AeN6lk6kI9DZWS-kLsemqXXZmGw0zrTYEjqVzOqQsTUGPF905~68e3FSCLIUwy4iuigAJfBAxBz5ON8oAlcTlMYl0WeONU~QYUa4j3XqIdCa0o2935~MHWIz~eCKOTKaNdjcC6brCIli9WZ4D1vpXjgqG7Zbc3klQ~YLR4O22HB8T~CrBbL36hV~hOM7krthSkD4EEagm~Ec7BwgTwVhE06onqh8ptNXXVlkvSbNb8FYOWfe617lEl73cOMBIQ__&Key-Pair-Id=APKAIE5G5CRDK6RD3PGA)
This feature is available to Subscribers Only
Sign In or Create an Account Close Modal