Abstract
In the developing myocardium, vascular endothelial growth factor (VEGF)–dependent neovascularization occurs by division of existing vessels, a process that persists for several weeks following birth. During this remodeling phase, mRNA expression of β3 integrin in the heart decreases significantly as vessel maturation progresses. However, in male mice lacking β3, coronary capillaries fail to mature and continue to exhibit irregular endothelial thickness, endothelial protrusions into the lumen, and expanded cytoplasmic vacuoles. Surprisingly, this phenotype was not seen in female β3-null mice. Enhanced VEGF signaling contributes to the β3-null phenotype, because these vessels can be normalized by inhibitors of VEGF or Flk-1. Moreover, intravenous injection of VEGF induces a similar angiogenic phenotype in hearts of adult wild-type mice. These findings show a clear vascular phenotype in the hearts of mice lacking β3 and suggest this integrin plays a critical role in coronary vascular development and the vascular response to VEGF.
Introduction
Integrins often cooperate with angiogenic growth factor receptors and are critical components of signaling pathways leading to angiogenesis.1 Integrins provide physical and chemical links between cells and extracellular matrix, serving as structural organizers, mechanotransducers, and signaling molecules. In this context, integrin-mediated signaling could uniquely affect the structure and function of an individual cell based on its microenvironment (extracellular matrix components, tissue oxygenation, and growth factor concentration) and expression of particular integrin subunits and/or growth factor receptors. Integrin αvβ3 is either absent or expressed at low levels on normal endothelial cells in vivo but is significantly elevated on the angiogenic blood vessels associated with wounds, inflammatory sites,2 or tumors.3 Accordingly, integrin αvβ3 antagonists promote tumor regression by inducing apoptosis of angiogenic blood vessels while sparing the quiescent endothelial cells on pre-existing vessels.3,4 These results support the concept that αvβ3 regulates endothelial-cell survival to support tumor growth and angiogenesis.
However, in apparent disagreement with studies using αvβ3 integrin antagonists, mice lacking β3 actually show an enhanced angiogenic response in tumors.5 Despite this apparent controversy, β3-null mice provide an interesting tool to study the requirement of αvβ3 and αIIbβ3 in various tissues and cell types (reviewed by Hynes and Hodivala-Dilke6 ). The β3-null mouse was originally described as a model of Glanzmann thrombasthenia,7 a pathology that is often associated with impaired αIIbβ3 expression or function in platelets. The β3-null mouse shows defects in platelet aggregation and bleeding7 as well as enhanced vascular endothelial growth factor (VEGF)–induced endothelial-cell migration, proliferation, permeability, and angiogenesis.5,8 Enhanced tumor growth in β3-null mice has been attributed to increased endothelial-cell expression of the VEGF receptor Flk-1/KDR9 and decreased macrophage infiltration.9,10 β3-null mice also have enhanced inflammatory11 and wound healing responses,12 the latter due to increased fibroblast infiltration and increased TGF-β1 expression.12 Together, these results suggest that β3 expression on the host vasculature may actually suppress tumor growth and angiogenesis.
To address the role of β3 integrin during physiologic angiogenesis, we examined the vascular proliferation that occurs in the heart during the first few postnatal weeks. In this time frame, the vasculature in the heart remodels dramatically as the number of capillaries increases significantly by division of pre-existing vessels.13 This neonatal vascular remodeling phase supports homogeneous oxygen delivery for hypertrophying cardiomyocytes and has been associated with high levels of basic fibroblast growth factor (bFGF) and VEGF expression.13 In fact, development during the first 4 postnatal weeks requires VEGF activity, because VEGF gene ablation or receptor blockade during this period resulted in growth arrest and lethality in mice.14 The adult coronary vasculature can also remodel in response to VEGF, because adenoviral VEGF expression induces a rapid increase in Flk-1 expression on normal cardiac capillaries, which stimulates formation of mother vessels and subsequent division into daughter vessels.15 The mature adult heart also has the capacity to remodel in response to oxygen demand, because coronary capillary density can substantially increase due to chronic exercise.16 Hypoxia promotes cardiac capillary-cell growth in part by inducing myocyte VEGF expression,17 suggesting an intricate feedback system for localized control of angiogenesis.
Aside from an enhanced responsiveness to vascular insult, no study has defined a vascular phenotype for the β3-null mice. Here, we report that coronary capillaries in the adult male β3-null mouse fail to mature, and they resemble the immature vessels observed during early postnatal development. Dysregulated VEGF and Flk-1 signaling contributes to the vascular phenotype in the β3-null mouse, because inhibitors of this pathway can induce capillary maturation. Furthermore, intravenous injection of VEGF into normal mice induces a similar vascular phenotype in coronary capillaries, suggesting that coronary blood vessels (compared with those from other organs) are highly reactive to changes in VEGF concentration. We report here that expression of β3 integrin in the heart decreases significantly during the first few postnatal weeks, concurrent with the cessation of physiologic angiogenesis and maturation of coronary capillaries. Together, these findings support a role for β3 integrin in cardiac vascular development as well as responsiveness to VEGF signaling.
Materials and methods
Pharmacologic agents
The SU1498 Flk inhibitor (20 mg/kg intraperitoneally daily, 385 nM) and Cyclo-VEGI (CBO-P11) VEGF inhibitor (2 mg/kg intraperitoneally daily, 13 nM) were purchased from Calbiochem (San Diego, CA). The SKI-606 Src family kinase inhibitor18,19 was injected twice daily (10 mg/kg intraperitoneally, 236 nM). These dosing conditions effectively block tumor-cell extravasation in mice.20
Mice
Mice with gene-targeted deletion of β3-integrin are available from The Jackson Laboratory (Bar Harbor, ME). β3-deficient mice on the SV129 background were provided by Drs D. Sheppard and R. Hynes and were genotyped as previously described.7
Ultrastructural analysis by scanning electron microscopy
Mice were killed and perfused via the left ventricle with saline followed by phosphate buffer containing 2% paraformaldehyde and 4% glutaraldehyde. Tissue was excised, immersion fixed overnight, transferred to 0.1 M sodium cacodylate buffer (pH 7.3) containing 1% osmium tetroxide for 2 hours, and then dehydrated in graded alcohols. Tissue was freeze-fractured in liquid nitrogen, stored in 100% ethanol, and subjected to critical point drying and sputter coating. Samples were viewed on a Hitachi S-2700 scanning electron microscope (Hitachi, Schaumburg, IL).
Ultrastructural analysis by transmission electron microscopy
Mice were killed and perfused via the left ventricle with 0.1 M sodium cacodylate buffer (pH 7.3) containing 4% paraformaldehyde and 1.5% glutaraldehyde. Tissue was excised and fixed for 2 hours, transferred to 5% glutaraldehyde overnight, and then into 1% osmium tetroxide for 1 hour. Blocks were washed, dehydrated, cleared in propylene oxide, infiltrated with Epon-Araldite, and embedded in resin. Ultrathin sections were stained with uranyl acetate and lead citrate and viewed using a Philips CM-100 transmission electron microscope (Philips, Mahwah, NJ). Negatives were scanned on an Epson 1680 scanner (Epson, Long Beach, CA) using Adobe Photoshop 7.0 software (Adobe Systems, San Jose, CA).
Immunohistochemistry
Routine immunostaining and imaging of frozen sections was performed as previously described1 using primary antibodies from BD Biosciences (San Diego, CA): integrin β3/CD61 (550541); Flk-1 (550549); PECAM-1/CD31 (550274); rat IgG2a,κ isotype control (559073); and hamster IgG1, κ isotype control (550344). Images were acquired using an Olympus BX60 light microscope (Olympus, Center Valley, PA) equipped with a UPlanFl 10×/0.30 numerical aperature (NA) or a UPlanApo 20×/0.70 NA objective and a SPOT camera (model 2.2.1; Diagnostic Instruments, Sterling, Heights, MI).
Analysis of mRNA expression
Total RNA was isolated with TRIZOL (Invitrogen, Carlsbad, CA), and reverse transcriptase–polymerase chain reaction (RT-PCR) was performed using Invitrogen Superscript III kit. Real-time PCR reactions were performed using Absolute QPCR Mix (ABgene, Rochester, NY) and cDNA analyzed using a Cepheid (Sunnyvale, CA) SmartCycler. Primer sequences are listed in Table 1. GAPDH was evaluated using 1 cycle (92°C, 900 seconds) and 40 cycles (95°C, 15 seconds; 60°C, 60 seconds). VEGF, Flk, and Flt were evaluated using 1 cycle (92°C, 900 seconds) and 40 cycles (95°C, 15 seconds; 60°C, 30 seconds; 72°C, 30 seconds). Cycle threshold was determined for each sample, samples were normalized to GAPDH, and relative gene expression levels were determined as previously described.21
Primers for mRNA expression
| Primer . | Sequence . |
|---|---|
| VEGF164-S | GCC AGC ACA TAG AGA GAA TGA GC |
| VEGF164-AS | CAA GGC TCA CAG TGA TTT TCT GG |
| VEGF164-probe | TxRED-ACA GCA GAT GTG ATG GCA GAC CAA AGA AAG-BHQ2a |
| FLK-S | CGA CAT AGC CTC CAC TGT TTA TG |
| FLK-AS | TTT GTT CTT GTT CTC GGT GAT GT |
| FLK-probe | TET-TTC ATC GCC TCT GTC AGT GAC CAG CAT-BHQ1 |
| FLT-S | ACC TGT CCA ACT ACC TCA AGA GC |
| FLT-AS | CTG GTT CCA GGC TCT CTT TCT T |
| FLT-probe | TxRED-TTC TGT CTC AAC AAG GAC GCA GCC TT-BHQ2a |
| GAPDH-S | CCT GCA CCA CCA ACT GCT TA |
| GAPDH-AS | TCA TGA GCC CTT CCA CAA |
| GAPDH-probe | FAM-CCT GGC CAA GGT CAT CCA C-BHQ1 |
| Primer . | Sequence . |
|---|---|
| VEGF164-S | GCC AGC ACA TAG AGA GAA TGA GC |
| VEGF164-AS | CAA GGC TCA CAG TGA TTT TCT GG |
| VEGF164-probe | TxRED-ACA GCA GAT GTG ATG GCA GAC CAA AGA AAG-BHQ2a |
| FLK-S | CGA CAT AGC CTC CAC TGT TTA TG |
| FLK-AS | TTT GTT CTT GTT CTC GGT GAT GT |
| FLK-probe | TET-TTC ATC GCC TCT GTC AGT GAC CAG CAT-BHQ1 |
| FLT-S | ACC TGT CCA ACT ACC TCA AGA GC |
| FLT-AS | CTG GTT CCA GGC TCT CTT TCT T |
| FLT-probe | TxRED-TTC TGT CTC AAC AAG GAC GCA GCC TT-BHQ2a |
| GAPDH-S | CCT GCA CCA CCA ACT GCT TA |
| GAPDH-AS | TCA TGA GCC CTT CCA CAA |
| GAPDH-probe | FAM-CCT GGC CAA GGT CAT CCA C-BHQ1 |
S indicates sense; AS, antisense.
For integrin β3 mRNA expression, quantitative PCR was performed on a Cepheid SmartCycler using 1 cycle (92°C, 900 seconds) and 40 cycles (95°C, 15 seconds; 66°C, 30 seconds, 72°C, 45 seconds) with SYBR Green (Molecular Probes, Carlsbad, CA) at 1:10 000. Primers were from Maxim Biotech (San Francisco, CA): 5′-GGAAGCAGCGCCCAGATCAC and 3′-TTGTCCACGAAGGCCCCAAA.
Statistical analysis
Results
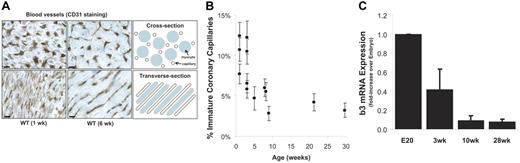
Myocardial vascular development in mice persists for several weeks following birth and is dependent on bFGF and VEGF signaling pathways.13 Vascular remodeling in the postnatal heart is characterized by division of existing vessels to support significant cardiac myocyte hypertrophy. Figure 1A. illustrates the significant reorganization of endothelial cells (identified by PECAM-1/CD31 staining) between 1 and 6 weeks of age, providing a uniform distribution of capillaries adjacent to each myocyte to support homogeneous tissue oxygenation in the adult heart tissue.
Postnatal angiogenesis and vascular remodeling in the heart. The cardiac coronary capillary bed undergoes significant vascular remodeling during a postnatal period of myocyte hypertrophy. (A) Immunostaining for PECAM-1/CD31 shows capillaries in cross section (top) or transverse section (bottom) for 1- and 6-week-old wild-type mice. The schematic illustrates how myocytes (blue) and capillaries (brown) are organized in the adult heart for homogeneous tissue oxygenation. Using TEM, a blinded observer examined several hundred coronary capillaries per mouse and recorded the frequency of luminal filopodia, expanded vacuoles, and/or intussusception. These characteristics of immature, angiogenic blood vessels were observed more frequently in neonatal mice (1 to 3 weeks old) of either sex (B). β3 integrin mRNA expression, considered a marker of angiogenic endothelium, decreases rapidly with age following birth on a similar time scale as capillary maturation (C). (A) Scale bar = 5 μm. (B-C) Data represent mean ± SE.
Postnatal angiogenesis and vascular remodeling in the heart. The cardiac coronary capillary bed undergoes significant vascular remodeling during a postnatal period of myocyte hypertrophy. (A) Immunostaining for PECAM-1/CD31 shows capillaries in cross section (top) or transverse section (bottom) for 1- and 6-week-old wild-type mice. The schematic illustrates how myocytes (blue) and capillaries (brown) are organized in the adult heart for homogeneous tissue oxygenation. Using TEM, a blinded observer examined several hundred coronary capillaries per mouse and recorded the frequency of luminal filopodia, expanded vacuoles, and/or intussusception. These characteristics of immature, angiogenic blood vessels were observed more frequently in neonatal mice (1 to 3 weeks old) of either sex (B). β3 integrin mRNA expression, considered a marker of angiogenic endothelium, decreases rapidly with age following birth on a similar time scale as capillary maturation (C). (A) Scale bar = 5 μm. (B-C) Data represent mean ± SE.
To observe the properties of these angiogenic vessels throughout the cardiac vascular hierarchy, transmission electron microscopy (TEM) was employed. For quantification, a blinded observer examined several hundred coronary capillaries per heart by TEM to determine what percentage contained angiogenic/immature vessels as evidenced by the presence of luminal protrusions, enlarged vacuoles, or thickened endothelium. Consistent with previous findings,13 we found that coronary capillaries continue to remodel for several weeks following birth. Specifically, neonate and weanling mice of either sex have a significant percentage of immature or angiogenic coronary capillaries (6% to 12%) compared with adult and senescent mice (3% to 6%) (Figure 1B).
Integrin αvβ3 is associated with angiogenic vessels in tumors, inflammation, or wounds.2,3 Therefore, we evaluated β3 mRNA expression levels in left ventricle homogenates of mice ages E20 (late-stage embryo), 3 weeks (weanling), 10 weeks (adult), and 28 weeks (senescent adult). We found that β3 expression decreases significantly with age (Figure 1C) on a time line similar to the maturation of coronary capillaries (Figure 1B). These findings suggest that elevated β3 expression is associated with angiogenic, activated endothelium and that the loss of β3 parallels the transition into mature, quiescent endothelial cells lining the coronary capillaries.
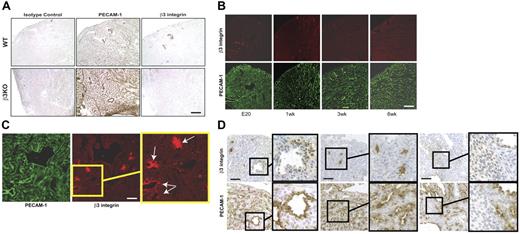
To determine the temporal expression and localization of this integrin during development in wild-type mice, we evaluated the protein expression of β3 integrin in the heart at different developmental stages. Figure 2A.shows validation of the hamster anti–mouse β3 integrin antibody for immunohistochemistry, because the antibody positively stains the wild-type but not β3 knockout heart. This reagent produced similar staining patterns using either immunofluorescence or immunoperoxidase staining. Similar to mRNA expression (Figure 1C), β3 protein expression in the heart decreased with age (Figure 2B). In adult hearts, β3 staining was detected only in nonendothelial cells on coronary arteries (Figure 2A-B). In the late-stage embryo hearts, the most obvious β3-positive staining was evident near areas of vascular remodeling where vascular structures of different sizes were clustered (Figure 2C, arrows). In addition, β3 staining in the late-stage embryo heart was associated with arteries (Figure 2D, left panel), interstitial cells (Figure 2D, middle panel), and myocytes (Figure 2D, right panel).
β3 integrin protein expression in the mouse heart. Immunostaining serial sections for PECAM-1 and β3 integrin confirms the hamster antimouse antibody can detect β3 protein expression in wild-type (but not β3-null) mouse hearts (A). During the first few postnatal weeks, β3 protein expression decreases and is only faintly detected on smooth muscle cells on small arteries in the adult heart (B). In late-stage embryo hearts, β3 integrin is found near areas of vascular remodeling (C, arrows indicate clusters of vessels) or associated with vascular structures (D, left), interstitial cells (D, middle), and myocytes (D, right). Bar = 100 μm (A-B) or 200 μm (C-D).
β3 integrin protein expression in the mouse heart. Immunostaining serial sections for PECAM-1 and β3 integrin confirms the hamster antimouse antibody can detect β3 protein expression in wild-type (but not β3-null) mouse hearts (A). During the first few postnatal weeks, β3 protein expression decreases and is only faintly detected on smooth muscle cells on small arteries in the adult heart (B). In late-stage embryo hearts, β3 integrin is found near areas of vascular remodeling (C, arrows indicate clusters of vessels) or associated with vascular structures (D, left), interstitial cells (D, middle), and myocytes (D, right). Bar = 100 μm (A-B) or 200 μm (C-D).
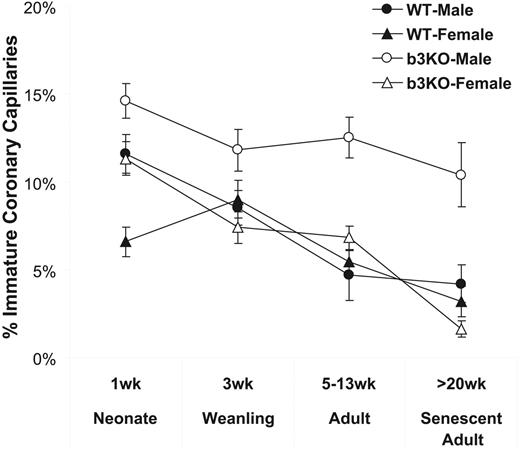
To test whether the loss of β3 expression is required for coronary maturation, we examined hearts from mice lacking β3 integrin. Previous findings have suggested that β3-null mice have no vascular defect.5,7–9 After examining the coronary vasculature of β3-null mice during the phase of VEGF-dependent postnatal vascular remodeling in the heart, we found that myocyte growth and angiogenesis was similar between genotypes. Specifically, there is no evidence that the vascular organization or coronary capillary density is different in the β3-null mouse heart after careful evaluation using immunohistochemistry and intravenous lectin perfusion (data not shown). However, adult β3-null males but not females have considerably more immature vessels than their wild-type counterparts (13% ± 1% versus 5% ± 1% of vessels examined for β3-null and wild-type male mice, respectively). While the percentage of immature coronary capillaries decreases with age, 27-week-old senescent male β3-null mice continue to exhibit 10% ± 2% immature vessels (Figure 3). This immature blood vessel phenotype appears to be restricted to the capillaries in the hearts of male β3-null mice, because capillaries in liver, lung, brain, or skin did not contain thickened endothelial cells, luminal filopodia, or expanded vacuoles (not shown). Previously, we have used electron microscopy to observe vascular leak in the heart at the ultrastructural level.20,23 We identified leak as gaps between adjacent endothelial cells exposing basement membrane, attraction of platelets, platelet activation and aggregation, capillary occlusion or collapse, extravasation of blood cells, and interstitial edema. In the current study, we examined a large number of electron micrographs, but we did not observe these signs of vascular leak in the β3-null mouse heart. Thus, it appears that vascular leak is not a consequence of the immature capillaries in β3-null mice.
Immature coronary capillaries in the male β3-null mouse heart. Using TEM, we evaluated whether coronary capillary maturation is affected by null expression of β3 integrin. Whereas the frequency of immature vessels decreases with age in male and female wild-type mice as well as female β3-null mice, β3-null mice continue to display these immature characteristics, even in senescent (27-week-old) mice.
Immature coronary capillaries in the male β3-null mouse heart. Using TEM, we evaluated whether coronary capillary maturation is affected by null expression of β3 integrin. Whereas the frequency of immature vessels decreases with age in male and female wild-type mice as well as female β3-null mice, β3-null mice continue to display these immature characteristics, even in senescent (27-week-old) mice.
By 5 weeks of age in wild-type mice, the coronary vasculature is composed of mature vessels with consistent endothelial-cell thickness and a smooth luminal surface with very few protrusions (Figure 4A-B). In contrast, coronary capillaries in adult male mice lacking β3 integrin closely resemble angiogenic blood vessels and immature blood vessels previously reported in neonatal mice.13 To our surprise, we observed no such defect in female mice lacking αvβ3. While normal blood vessels have a uniform endothelial thickness (Figure 4A-B), endothelial-cell thickness in male β3-null hearts varies considerably (Figure 4C-D). The thickened endothelium is often associated with the more frequent appearance of organelles such as mitochondria or ribosomes (Figure 4C-D). Like the invasive filopodia, these are characteristics of activated, angiogenic endothelial cells, such as those on immature neonatal blood vessels.24
Male β3-null coronary capillaries appear immature and angiogenic.Transmission electron micrographs show that coronary capillaries from adult wild-type mice (A-B) are composed of endothelial cells with a smooth luminal surface and uniform thickness around the vessel perimeter. In contrast, coronary capillaries from adult male β3-null mice (C-E) often have irregular endothelial-cell thickness (arrows) along with filopodia extending into the vessel lumen (arrows). The luminal filopodia can originate from cell-cell junctions as well as from the central region of a single endothelial cell (E). All filopodia appear to extend toward the vessel lumen rather than into the extravascular space. The frequent presence of organelles such as mitochondria and ribosomes in regions of thickened endothelium is consistent with activated endothelial cells. Luminal filopodia in male β3-null coronary capillaries appear to extend toward (F) or interact with (G-H) adjacent filopodia. The presence of electron-dense staining at points of contact suggests that interactions between filopodia may represent adhesive events. Connections between filopodia appear to form pockets within a single vessel lumen, consistent with angiogenesis by division of existing vessels. Bar = 500 nm.
Male β3-null coronary capillaries appear immature and angiogenic.Transmission electron micrographs show that coronary capillaries from adult wild-type mice (A-B) are composed of endothelial cells with a smooth luminal surface and uniform thickness around the vessel perimeter. In contrast, coronary capillaries from adult male β3-null mice (C-E) often have irregular endothelial-cell thickness (arrows) along with filopodia extending into the vessel lumen (arrows). The luminal filopodia can originate from cell-cell junctions as well as from the central region of a single endothelial cell (E). All filopodia appear to extend toward the vessel lumen rather than into the extravascular space. The frequent presence of organelles such as mitochondria and ribosomes in regions of thickened endothelium is consistent with activated endothelial cells. Luminal filopodia in male β3-null coronary capillaries appear to extend toward (F) or interact with (G-H) adjacent filopodia. The presence of electron-dense staining at points of contact suggests that interactions between filopodia may represent adhesive events. Connections between filopodia appear to form pockets within a single vessel lumen, consistent with angiogenesis by division of existing vessels. Bar = 500 nm.
The filopodia observed in β3-null mouse coronary capillaries are exclusively luminal processes, as opposed to the outward sprouting of endothelial cells often associated with some angiogenic blood vessels. The luminal protrusions appear to originate from cell-cell junctions (Figure 4D, arrow) as well as from the continuous cytoplasm within a single endothelial cell (Figure 4C, arrow). An example of a single endothelial cell from which luminal protrusions are extending from cell junctions on either side as well as from the middle of the cytoplasm (arrows) is shown in Figure 4E. Despite the immature vascular phenotype, adhesive junctions between adjacent endothelial cells appear to remain intact (Figure 4D-E), suggesting that the vascular barrier is not disrupted. In many cases, filopodia protruding into the lumen often appear to extend toward (Figure 4F) and make additional adhesive contacts with adjacent filopodia or endothelial-cell membrane (Figure 4G-H). Electron-dense patches between endothelial cells are representative of adhesive contacts,25 suggesting that the tips of these filopodia are actively forming intercellular junctions leading to communication or adhesion events within these capillaries. These interactions between filopodia often appear to partition a portion of the capillary lumen, which is consistent with angiogenesis by the division of existing vessels. Some β3-null coronary capillaries appear to contain expanded vacuoles of varying size (Figure 5A-D). Because no cell-cell junctional staining is visible, these vacuoles appear to be contained within the cytoplasm of a single endothelial cell. Although less frequent, we did observe capillaries that appear to be dividing by intussusception (Figure 5E), the formation of transluminal pillars to facilitate vessel division.26
Expanded vacuoles and intussusception in male β3-null coronary capillaries. Transmission electron micrographs show that coronary capillaries from male β3-null mice contain single endothelial cells with expanded vacuoles (A-D) that, like pockets formed by interacting filopodia, are consistent with angiogenesis by division of existing vessels. Some vessels have a limited luminal area and appear to be composed of a single endothelial cell (B), because cell-cell junctions are not visible. Although less frequent, some endothelial cells have luminal processes that extend across the lumen, resembling angiogenesis by intussusception (E). Asterisks indicate expanded vacuoles; arrows, intussusception. Bar = 500 nm.
Expanded vacuoles and intussusception in male β3-null coronary capillaries. Transmission electron micrographs show that coronary capillaries from male β3-null mice contain single endothelial cells with expanded vacuoles (A-D) that, like pockets formed by interacting filopodia, are consistent with angiogenesis by division of existing vessels. Some vessels have a limited luminal area and appear to be composed of a single endothelial cell (B), because cell-cell junctions are not visible. Although less frequent, some endothelial cells have luminal processes that extend across the lumen, resembling angiogenesis by intussusception (E). Asterisks indicate expanded vacuoles; arrows, intussusception. Bar = 500 nm.
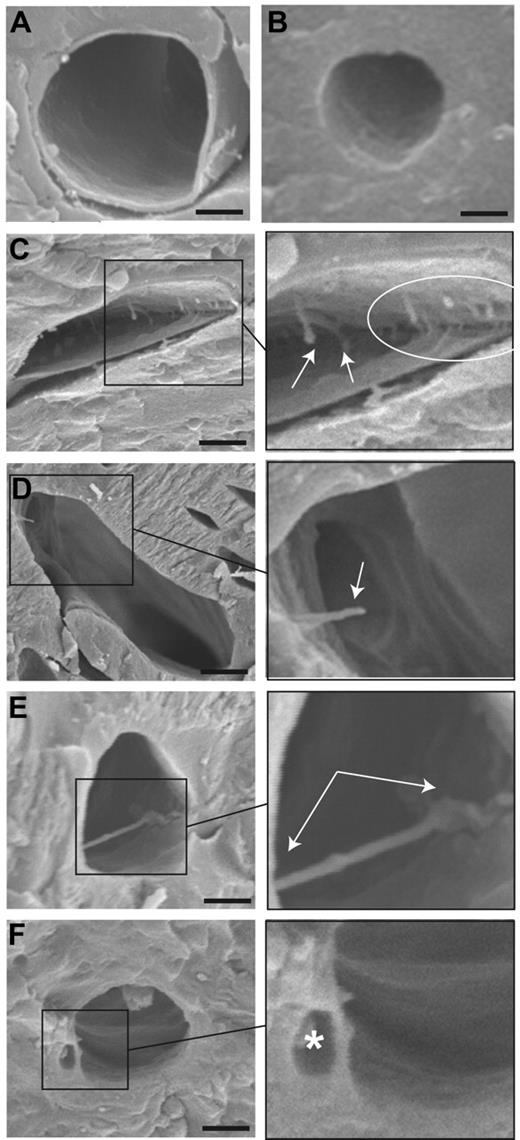
These ultrastructural observations made using TEM were also confirmed using scanning electron microscopy (SEM). Hearts from adult wild-type mice reveal normal coronary capillaries with smooth luminal surfaces (Figure 6A-B). However, invasive filopodia extending into the lumen of coronary capillaries can be observed in the adult male β3-null mouse heart (Figure 6C-E, arrows). In some β3-null vessels, filopodia appear to bridge across the lumen to contact the opposing vessel wall (Figure 6E, arrow). Pockets consistent with the extended vacuoles observed via TEM can also be observed (Figure 6F, asterisk).
Blood vessel phenotype in male β3-null mice is confirmed by scanning electron microscopy. Coronary capillaries from adult wild-type mice (A-B) have a smooth luminal surface consistent with images acquired using TEM. Freeze-fractured samples prepared for SEM reveal filopodia extending into the vessel lumen (C-D) or across the lumen to make adhesive contact with the opposite wall (E). Luminal divisions are visible, which may represent the expanded vacuoles observed via TEM (F). Arrows indicate filopodia; asterisk, expanded vacuole. Bar = 500 nm.
Blood vessel phenotype in male β3-null mice is confirmed by scanning electron microscopy. Coronary capillaries from adult wild-type mice (A-B) have a smooth luminal surface consistent with images acquired using TEM. Freeze-fractured samples prepared for SEM reveal filopodia extending into the vessel lumen (C-D) or across the lumen to make adhesive contact with the opposite wall (E). Luminal divisions are visible, which may represent the expanded vacuoles observed via TEM (F). Arrows indicate filopodia; asterisk, expanded vacuole. Bar = 500 nm.
Enhanced responsiveness to VEGF in the β3-null mice has previously been attributed to increased endothelial-cell expression of Flk-1.5,9 Therefore, we evaluated Flk-1, Flt-1, and VEGF mRNA levels in total left ventricle homogenates from adult β3-null male mice compared with wild type. We found no significant differences in VEGF, Flt-1, or Flk-1 mRNA expression levels between adult male wild-type and β3-null mice (Table 2). However, we did detect a 60% reduction in VEGF mRNA expression in female β3-null mice relative to wild-type mice (Table 2), which may represent a compensatory mechanism to facilitate vessel maturation not observed in male mice.
Messenger RNA expression
| . | Flk-1 . | Flt-1 . | VEGF . |
|---|---|---|---|
| Male | |||
| WT | 1.0 ± 0.2 | 1.0 ± 0.3 | 1.0 ± 0.2 |
| β3KO | 1.1 ± 0.2 | 0.7 ± 0.2 | 1.1 ± 0.3 |
| Female | |||
| WT | 1.0 ± 0.2 | 1.2 ± 0.2 | 0.8 ± 0.2 |
| β3KO | 0.8 ± 0.3 | 0.7 ± 0.2 | 0.4 ± 0.5 |
| . | Flk-1 . | Flt-1 . | VEGF . |
|---|---|---|---|
| Male | |||
| WT | 1.0 ± 0.2 | 1.0 ± 0.3 | 1.0 ± 0.2 |
| β3KO | 1.1 ± 0.2 | 0.7 ± 0.2 | 1.1 ± 0.3 |
| Female | |||
| WT | 1.0 ± 0.2 | 1.2 ± 0.2 | 0.8 ± 0.2 |
| β3KO | 0.8 ± 0.3 | 0.7 ± 0.2 | 0.4 ± 0.5 |
Shown are fold increases relative to wild-type male, ± SEM.
WT indicates wild type; β3KO, β3 knockout.
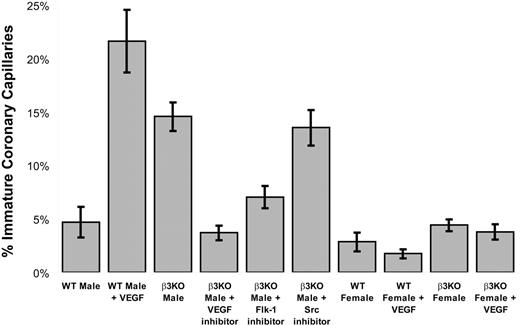
Together, these findings suggest that the immature blood vessel phenotype may be due to increased sensitivity to VEGF rather than an increase in either VEGF or VEGF receptor expression in the male β3-null mice. To determine whether VEGF signaling directly contributes to the angiogenic phenotype in the β3-null mouse, we treated mice with inhibitors of either VEGF or Flk-1 and examined their coronary arteries to quantify the level of vascular maturation by enumerating the frequency of luminal protrusions, thickened endothelium, or enlarged vacuoles. We found that the angiogenic phenotype in adult male β3-null mice could be suppressed by treatment with inhibitors of either VEGF or Flk-1 but not by treatment with inhibitors of other downstream signaling molecules such as Src family kinases (Figure 7). This experiment confirms that blocking VEGF (or Flk-1) activity in the β3-null male mouse is sufficient to inhibit the immature, angiogenic characteristics of the endothelial cells lining the capillaries in the heart.
VEGF/Flk-1 activity contributes to immature vascular phenotype in male β3-null mice. Two hours following intravenous injection of VEGF into adult male wild-type mice, 22% of coronary capillaries examined exhibited luminal filopodia, extended vacuoles, and/or intussusception. These characteristics following VEGF injection are of a similar frequency as observed for untreated adult male β3-null mice. When adult male β3-null mice are treated for 2 days with pharmacologic inhibitors of either Flk-1 or VEGF (but not downstream signaling molecules such as Src kinases), the frequency of immature coronary capillaries is reduced to normal levels. These findings suggest that enhanced VEGF signaling through Flk is responsible for the vascular phenotype in adult male β3-null mice. Interestingly, VEGF injection into adult female wild-type or β3-null mice did not produce the angiogenic phenotype. Data represent mean ± SE.
VEGF/Flk-1 activity contributes to immature vascular phenotype in male β3-null mice. Two hours following intravenous injection of VEGF into adult male wild-type mice, 22% of coronary capillaries examined exhibited luminal filopodia, extended vacuoles, and/or intussusception. These characteristics following VEGF injection are of a similar frequency as observed for untreated adult male β3-null mice. When adult male β3-null mice are treated for 2 days with pharmacologic inhibitors of either Flk-1 or VEGF (but not downstream signaling molecules such as Src kinases), the frequency of immature coronary capillaries is reduced to normal levels. These findings suggest that enhanced VEGF signaling through Flk is responsible for the vascular phenotype in adult male β3-null mice. Interestingly, VEGF injection into adult female wild-type or β3-null mice did not produce the angiogenic phenotype. Data represent mean ± SE.
Because the hypersensitivity to VEGF in the β3-null male mouse could effectively be normalized by treatment with inhibitors of either VEGF or Flk-1, we tested whether the mature endothelium in a wild-type mouse could likewise remodel in the presence of increased VEGF concentration. Therefore, we performed a direct intravenous injection of VEGF and examined the coronary endothelial cells for the presence of luminal protrusions, thickened endothelium, or enlarged vacuoles. We found that simple injection of VEGF induces these angiogenic characteristics in the wild-type mouse heart to a similar extent as we observed in the male β3-null mouse (Figure 7). This finding suggests that increased VEGF concentration alone is sufficient to induce an immature or angiogenic phenotype in the coronary capillaries in an otherwise normal mouse. However, when we injected VEGF into female wild-type or β3-null mice, we did not observe the angiogenic phenotype in the coronary capillaries (Figure 7). These data are consistent with the concept that females are protected from the occurrence or progression of some types of vascular disease. This finding warrants further investigation to determine how VEGF signaling in blood vessels in females may differ from counterparts in males. Taking all data into account, there appears to be a fine balance of VEGF signaling that dictates the morphology of the endothelial luminal surface.
Discussion
We have established that cooperative signaling between growth factors and integrins regulates blood vessel development in the postnatal heart. This regulatory phase of VEGF-mediated vascular development depends in part on integrin β3, because (1) β3 expression decreases as vessels mature in wild-type mice, (2) male mice lacking β3 show immature capillary vessels throughout adulthood, (3) immature capillaries can be induced in wild-type mice via intravenous injection of VEGF, and (4) the β3-null phenotype can be normalized by treatment with VEGF or Flk-1 inhibitors. We report a vascular phenotype consisting of immature coronary capillaries selectively in the hearts of male β3-null mice. The endothelial cells within these vessels contain luminal protrusions that fuse to divide the vessel lumen, similar in appearance to the VEGF-dependent vascular remodeling that occurs during the first few postnatal weeks. Female β3-null mice express 60% lower levels of VEGF mRNA in their hearts, suggesting a possible compensatory mechanism accounting for their lack of a vascular phenotype. Our findings raise important questions: What role do β3 integrins play during vascular development, and how do β3 integrins influence growth factor receptor signaling and angiogenesis?
Role of β3 integrins during vascular development
Integrin αvβ3 is highly expressed on angiogenic blood vessels, such as those associated with tumors,3 ischemic tissues,27 or inflammatory sites.2 During development, β3 integrin expression is restricted to a limited number of tissues compared with αv expression.28 Previous studies report that β3 mRNA expression levels are not detectable on a whole tissue basis except for the liver in the developing embryo.28 In situ hybridization shows very localized β3 expression in platelet-precursor megakaryocytes in the liver and in the border between developing smooth muscle and submucosa in the gastrointestinal tract.28 Endothelial cells in culture often express β3 integrin, although these cells are grown under proliferative culture conditions rather than the quiescent situation in vivo. Although β3 integrin mRNA expression has been detected in vitro on cultured myocytes, fibroblasts, and endothelial cells isolated from adult hearts,29 β3 is not normally expressed in adult blood vessels, except for microvessels in the lung.30,31 Following myocardial infarction, β3 mRNA expression has been detected in the heart on vascular structures at the edge of the infarct zone.32 In this study, we report that β3 mRNA and protein expression in the left ventricle decreases significantly with age following birth on a similar time line as the maturation of coronary capillaries (Figures 1–2).
Immunohistochemical staining suggests that β3 protein expression is associated only with arteries in the adult heart but with a variety of cell types in the developing heart (Figure 2). These data raise the interesting question: If β3 expression is not present on capillaries, why are capillaries affected in β3-null mice? There are several possible explanations: (1) β3 may indeed be expressed on capillaries, but below levels of detection using immunohistochemistry, yet it is possible that relatively low β3 expression on adult endothelium may provide an important signal to maintain vessel maturity. (2) β3 may be absent on capillaries, but lack of expression may be relevant on supporting stromal cells or other cell types that influence vascular maturation. It is feasible that supporting stromal cells contribute to normal vascular development by their direct interaction with vascular cells or by producing and releasing growth factors, cytokines, or extracellular matrix. Myocytes, smooth muscle cells, or fibroblasts may secrete growth factors that influence capillary maturation. This possibility is supported by the established roles of bFGF and VEGF during postnatal vascular development in the heart13 and by our own data in Figure 7 suggesting that inhibitors of Flk-1 signaling can offset the loss of β3 integrin. (3) The lack of β3 expression may change the fate of endothelial cells or angiogenic precursor cells at the stem-cell level. The lack of β3 on endothelial-cell precursors could potentially prevent the later evolution of these cells into mature, quiescent endothelium. Generating a mouse with endothelial-specific knockout of β3 integrin may provide means to address these issues as well as determine whether the lack of αIIbβ3 on platelets in the β3-null mouse contributes to the phenotype we have observed.
Regulation of growth factor signaling and angiogenesis by β3 integrins
Previous studies show that antagonists of αvβ3 cause apoptosis of endothelial cells growing in vivo.2,4 Consistent with this, others have reported that αvβ3 is part of an angiogenic “off switch,” which could be caused by the ability of this and other integrins in their unligated forms to induce integrin-mediated death.33–35 Our data support the hypothesis that a reduction in αvβ3 expression may be required during later stages of heart development to create mature, quiescent blood vessels. It is also possible that very low levels of αvβ3 expression contribute to a quiescent EC phenotype but could allow for a rapid angiogenic response dictated by local growth factor concentrations. Previous studies involving β3-null mice also support the notion that αvβ3 expression dampens excessive VEGF and TGF-β1 signaling.5,12 In fact, there is evidence of a direct interaction between αvβ3 and Flk-1 among endothelial cells in vitro.36 If present in vivo, this interaction could act as a brake on the system to limit the extent of VEGF signaling. This pathway may involve different signaling complexes, because integrins are essential for shear stress–induced activation of Flk-1 but not for VEGF-induced Flk-1 activation.37
Reynolds and coworkers have previously reported that lung endothelial cells isolated from β3-null mice show increased expression of Flk-1, which they suggest as an explanation for the enhanced angiogenic response in these mice.5 It is possible that cultured cells grown under proliferative conditions may show differential expression or activity of a variety of proteins that are not relevant to those expressed on endothelial cells within blood vessels. It is unclear whether the coronary capillary phenotype we observe is due to altered endothelial-cell expression of Flk-1 that we cannot resolve in our whole tissue homogenates or whether Flk-1 expression is not altered in these mice in vivo. To investigate whether localized changes in Flk-1 expression may account for the angiogenic phenotype in the β3-null male mice, we evaluated whether Flk-1 protein expression was increased in the coronary capillaries in β3-null mice compared with wild type. However, immunostaining revealed no overt differences in Flk-1 expression or localization between genotypes (data not shown). Consistent with this, we found no significant differences in Flk-1 mRNA expression in β3-null mice (Table 2). Interestingly, we found Flk-1 protein expression on capillaries in the heart but not on arteries, arterioles, venules, or veins (data not shown). This differential expression suggests that the angiogenic or vascular permeability responses to VEGF via Flk-1 may occur solely within the capillary compartment in the adult heart.
To address the mechanism of increased VEGF sensitivity, we have shown that inhibiting VEGF signaling via treatment with an Flk-1 inhibitor is sufficient to normalize the immature capillary phenotype (Figure 7). We also report that female β3-null mice that do not exhibit this phenotype have lower VEGF expression (Table 2). Lastly, we show that injecting normal mice with VEGF can induce this phenotype (Figure 7). Together, these studies suggest that a balance between VEGF expression and Flk-1 activity can dictate capillary maturation in the postnatal heart and that β3 integrin expression plays a role in this VEGF/Flk-1 balance.
Some but not all aspects of the male β3-null cardiac vascular phenotype are consistent with postnatal or VEGF-induced capillary remodeling. While β3-null capillaries exhibit endothelial thickening and luminal protrusions, these apparently do not result in increased capillary density. This suggests that the β3-null coronary vasculature is not receiving all of the necessary signals to induce actual vessel division and capillary proliferation, such as removal of pericyte coverage or disruption of the underlying basement membrane. This concept is consistent with the hypothesis that increased endothelial-cell VEGF responsiveness is responsible for the angiogenic vessel phenotype, which can be normalized in β3-null mice by treatment with pharmacologic inhibitors of Flk-1 or VEGF or induced in wild-type mice by intravenous injection with VEGF. Compared with adenoviral VEGF expression, intravenous VEGF injection provides a much more transient stimulus, and thus may induce an endothelial-cell reaction, but would not be expected to produce a long-term angiogenic response.
A sex-specific vascular phenotype
Female β3-null mice, which display no overt phenotype, express lower levels of VEGF in the heart compared with their male counterparts. Interestingly, male (but not female) wild-type mice subjected to intravenous VEGF for just 2 hours develop the same angiogenic phenotype. Taken together, these findings suggest that the balance between VEGF concentration and VEGF receptor activation can shift cardiac endothelial cells from a quiescent to an angiogenic phenotype. The finding that VEGF did not induce this phenotype in female mice could be attributed to the fact that estrogen modulates cytokine-induced activation of endothelial cells38 and influences angiogenesis and VEGF receptor expression in coronary vessels.39 A recent review by Cid and coworkers examines the impact of estrogens on the vascular endothelium.40 Furthermore, steroid hormones can regulate expression of many genes (including integrins41 ) by altering their mRNA stability.42 It is possible that estrogen participates in a feedback mechanism regulating VEGF signaling, which could explain sex-specific influence of β3-null expression. However, if hormones protect young β3-null females, this difference should balance out in old age. However, we found that even senescent (more than 20-week-old) β3-null females had normal coronary capillary endothelial cells (not shown), suggesting that β3 integrins may be required for proper cardiovascular development rather than maintenance of a quiescent endothelium.
Previous reports on β3-null mice have not specified whether experiments used male or female mice. In these studies, individual experiments may have pooled data from both sexes, thereby masking the magnitude of consequences of β3-null expression. Our only clue as to the mechanism for this sex-specific genotype is our finding that female β3-null mice have lower VEGF mRNA expression in their hearts despite equivalent Flk-1 expression. Our data may provide unique insight as to sex-specific responses to ischemic insult, hypoxia, and VEGF regulation during cardiovascular disease and cancer. Notably, we have provided the first demonstration of a sex-specific phenotype in an integrin knockout mouse. The relationship between integrins, hormones, and growth factors warrants further investigation despite significant advances in our understanding of the molecular and cellular basis of cardiovascular sex differences.43
Conclusions
Our data support a role for β3 integrin in dictating sensitivity to VEGF signaling, because we can block the capillary phenotype in β3-null mice by treatment with a Flk-1 inhibitor and can induce this phenotype in normal mice by injection with VEGF. It is this finding that is particularly interesting, because previous studies have not adequately addressed whether β3 expression on tumor-associated blood vessels is a proangiogenic or antiangiogenic response. We have used TEM to examine tumor-associated blood vessels that express high levels of β3 and found endothelial-cell protrusions similar to the ones in immature coronary vessels (data not shown). In this respect, our data suggest that increased β3 expression on small vessels may serve to counteract angiogenic stimuli and promote vessel quiescence rather than potentiate blood vessel proliferation.
The endothelial-cell abnormalities in β3-null mice do not appear to impact cardiac development and function, suggesting that the physiologic significance may be modest. However, modest changes in β3 expression could impart angiogenic properties to endothelial cells and thus could contribute to the pathologic progression of disease. In fact, β3 integrin is not expressed on normal blood vessels,3,27 but its expression increases in tumor endothelium,3 cardiac blood vessels following myocardial infarction,32 and cerebral blood vessels following ischemic stroke.27 Our data show malformed vessels in integrin knockout mice not previously known to have a vascular phenotype and suggest a new link between integrins and VEGF. Because female mice appear to produce less VEGF in their hearts, regulation of VEGF expression may play a compensatory role in vascular homeostasis, which is itself a very important observation. Our data raise the following new and important questions: What does the dysregulation of VEGF do? How is VEGF sensitivity in the heart different from that in other organs? Is vascular development and remodeling in the heart unique? Understanding these issues will be critical for treating cardiovascular disease and cancer, for which VEGF is a current therapeutic target.
In summary, we have defined a vascular phenotype for male β3-null mice in which coronary capillary maturation does not occur during the first few postnatal weeks, suggesting a role for integrin β3 during VEGF-dependent postnatal vascular remodeling in the heart. The capillary maturation process is dependent on VEGF and Flk-1 signaling, because inhibitors of these pathways normalize the immature coronary capillaries in β3-null mice and intravenous injection of VEGF into normal wild-type mice induces a similar angiogenic phenotype. Together, these studies suggest that β3 integrin plays a critical role in vascular development/maturation and regulating the vascular sensitivity to VEGF in the heart.
Authorship
Contribution: S.M.W. designed research, performed research, collected data, analyzed data, and wrote the paper; J.N.L. designed research, performed research, and collected data; L.A.B., K.M.L.-F., and J.C. performed research and collected data; M.R.W. performed electron microscopy; and D.A.C. designed research, analyzed data, and wrote the paper.
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Correspondence: David Cheresh, Moores UCSD Cancer Center, 3855 Health Sciences Dr #0803, La Jolla CA 92093-0803; dcheresh@ucsd.edu.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 USC section 1734.
Acknowledgments
This work was supported by National Institutes of Health (NIH) grants CA50286, CA45726, CA95262, HL57900, and HL78912 (D.A.C.) and 1F32HL69701 (S.M.W.).
We thank Peggy Hogan and Theresa Fassel for technical assistance and Steve Barlow for performing the scanning electron microscopy at the San Diego State University Electron Microscopy Facility. Dean Sheppard and Richard Hynes kindly provided founder mice for our β3-null mouse colony.



This feature is available to Subscribers Only
Sign In or Create an Account Close Modal