Abstract
Diamond-Blackfan anemia (DBA) is a congenital erythroid aplasia that usually presents as macrocytic anemia during infancy. Linkage analysis suggests that at least 4 genes are associated with DBA of which 2 have been identified so far. The known DBA genes encode the ribosomal proteins S19 and S24 accounting for 25% and 2% of the patients, respectively. Herein, we review possible links between ribosomal proteins and erythropoiesis that might explain DBA pathogenesis. Recent studies and emerging findings suggest that a malfunctioning translational machinery may be a cause of anemia in patients with DBA.
Introduction
Diamond-Blackfan anemia (DBA) is categorized as a congenital hypoplastic anemia, presenting during infancy with normochromic-macrocytic anemia, reticulocytopenia, and low numbers of erythroid precursors in the bone marrow. In addition to anemia more than 50% of patients with DBA have a short stature and/or various physical abnormalities.1 Already in 1938 L. K. Diamond and K. D. Blackfan discussed the cause of this bewildering disease and proposed: “…there may be congenital insufficiency of red marrow tissue and inability on the part of the hematopoietic system to respond to the need for more blood as the erythrocytes wear out.”2(p465) The pathogenetics causing DBA remained speculative until 1999 when a balanced reciprocal translocation t(X;19) was discovered in a patient, revealing the first DBA gene (DBA1).3 The identification of the affected gene in a congenital disorder, such as DBA, is often the key that suddenly enables understanding of the molecular pathogenesis and development of novel therapies. Surprisingly, DBA1 was identified as ribosomal protein S19 (RPS19), not a regulator of erythropoiesis as might be expected but a ribosomal protein that is vastly expressed in all tissues. Recently, the identification of a second DBA gene has established DBA as a ribosomal disorder because the affected gene encodes ribosomal protein S24 (RPS24).4 Herein, we review the major advances toward answering the question of how a deficiency of a ubiquitously expressed ribosomal protein can specifically affect erythroid development.
Clinical features and current treatment
DBA is a congenital hypoplastic anemia that develops within the first year of life, often with pallor as the only initial symptom. Typical laboratory findings include decreased hemoglobin levels, elevated mean corpuscular volume (MCV), and reticulocytopenia.5,6 Bone marrow examination reveals an isolated erythroid hypoplasia in normocellular marrow. Additional hematologic findings supporting the DBA diagnosis are elevated erythrocyte adenosine deaminase (eADA) activity,7 elevated fetal hemoglobin, and elevated serum erythropoietin. Growth retardation and/or thumb, craniofacial, heart, or urogenital anomalies further support the DBA diagnosis.1 Although not yet statistically validated, patients with DBA also seem to have an increased risk of acute myeloid leukemia (AML) and a wide variety of nonhematopoietic tumors, for example, osteogenic sarcomas.1,8-10 The main differential diagnosis is transient erythroblastopenia of childhood.6,11
After confirmed diagnosis of DBA, the initial therapeutic regimen consists of blood transfusions followed by corticosteroid treatment. The therapeutic mechanism of corticosteroids in DBA does not involve modulation of RPS19 expression, but rather increased sensitivity to erythropoietin (Epo) and a broad change of gene expression promoting erythroid differentiation.12,13 The response to steroid therapy varies considerably among patients. For an unknown reason, 20% go into remission, often after many years of steroid or transfusion therapy and maintain normal hemoglobin levels even without further treatment. Forty percent of patients with DBA remain transfusion independent on continuous steroid treatment, whereas the remaining 40% fail to respond or become irresponsive to steroids and need chronic transfusion therapy.1 Although long-term cortisone treatment can rid patients from transfusion dependence, it also puts them at risk of serious side effects such as Cushingoid features, growth retardation, and cataracts. Addition of iron-chelating therapy is required in the transfusion-dependent patients because long-term iron acquisition from chronic transfusion therapy can cause a potentially fatal iron overload in the liver; heart; pancreas; testicles; pituitary, thyroid, and parathyroid glands; and other organs. Allogenic bone marrow transplantation is the only curative treatment, but it is associated with risks of procedure-related early mortality, graft failure, graft-versus-host disease, and infections and is only available for patients with DBA that have access to a suitable donor. Although controversial, preimplantation HLA typing provides parents of children with genotyped DBA an option of ensuring that their next child is both healthy and a potential HLA-matched stem-cell donor, capable of curing the affected sibling.14
Pregnancies in DBA-affected women need to be followed carefully because they have a high risk of complications and fetal death.15 Because more than 50% of patients have physical malformations and/or growth retardation, the diagnosis of DBA must be accompanied with careful monitoring of growth rate and cardiac and genitourinary imaging. In addition, the responsible physician must be aware of the increased risk of malignancies, which requires a general attentiveness to signs of malignancy and routine blood counts.1,10
Inheritance and genetics
Most cases of DBA appear sporadic with an incidence of 5 to 7 per 1 000 000 live births at an equal sex ratio. Ten percent to 15% of patients have other family members with DBA, and another 30% have a first-degree family member with either elevated eADA levels or elevated MCV, possibly reflecting familial disease with incomplete penetrance.16,17 In families in which the DBA genotype is not characterized, relatives with elevated eADA and MCV may not be suitable as stem-cell donors because they possibly carry a silent DBA phenotype.16 Approximately 25% have a mutation in the RPS19 gene (Figure 1), whereas only 2% appear to have a mutation in the RPS24 gene.4 Linkage analysis further suggests that an unknown DBA gene is linked to chromosome 8p23,3-22.18 Because there is a group of non-RPS19 and non-RPS24 patients who are not linked to 8p23,3-22, at least 4 genes may be associated with DBA.
The RPS19 gene. The RPS19 gene consists of 6 exons. Exon 1 corresponds to the 5′ untranslated region of the mRNA and translation starts at the first nucleotide of exon 2. The point mutation hotspot region in patients with DBA is shown in yellow. Amino acid numbers are indicated at the start and end of exon 2 through 6. The illustration is not drawn to scale. Several studies have reported detailed mapping of RPS19 mutations in patients with DBA.20-22
The RPS19 gene. The RPS19 gene consists of 6 exons. Exon 1 corresponds to the 5′ untranslated region of the mRNA and translation starts at the first nucleotide of exon 2. The point mutation hotspot region in patients with DBA is shown in yellow. Amino acid numbers are indicated at the start and end of exon 2 through 6. The illustration is not drawn to scale. Several studies have reported detailed mapping of RPS19 mutations in patients with DBA.20-22
Most mutations in the RPS19 gene found in patients with DBA are predicted to cause either a nonfunctional protein or an abrogated translation (insertion, deletion, frame shift, and premature stop codon), whereas other mutations only change a single amino acid in the protein (missense mutation).16,19-22 Detailed family studies suggest that haploinsufficiency may be the genetic mechanism in most patients with DBA deficient in RPS19.22 RPS19 protein and mRNA expression analysis in several patients with RPS19-mutated DBA confirm that expression from the healthy RPS19 allele is not sufficient to compensate for the defective allele.21,23 It remains to be tested whether the mutated form of RPS19 may have a dominant-negative effect in some patients.
Erythropoiesis and cellular mechanisms in DBA
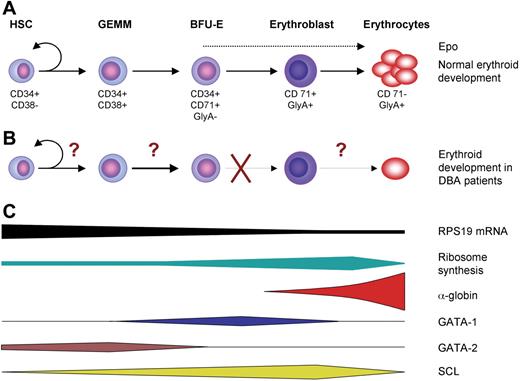
Erythropoiesis is the process in the BM where erythrocytes develop from hematopoietic stem cells (Figure 2A). Because hematopoietic progenitor cells are not morphologically distinguishable, they are best characterized by cell-surface marker expression. A common cell-surface marker used to enrich for human progenitor cells is CD34, whereas enrichment of erythroid-cell populations is based on CD71 and glycophorin A expression (Figure 2A). Transcriptional regulation of erythroid differentiation involves intrinsic spatiotemporal expression of transcription factors such as GATA-1, GATA-2, and SCL (Figure 2C).
Normal and DBA erythropoiesis. (A) Adult erythropoiesis is a process by which single hematopoietic stem cells in the bone marrow differentiate and proliferate into billions of red blood cells. The figure shows a simplified scheme of the series of differentiation processes that takes place during red cell development. The main regulator of terminal erythropoiesis is Epo. Commonly used cell-surface markers that are used to enrich for the different progenitor populations are shown below the cells. (B) In patients with DBA the erythroid development is severely compromised. One convincing study localizes the erythroid defect to the Epo-dependent stages after the BFU-E stage.13 However, since there are reports of decreased BFU-E colony formation and decreased proliferation of multipotent progenitors in patients with DBA, it is possible that more primitive progenitors are affected as well.26 (C) The expression of RPS19 is high in primitive progenitor cells and decrease in more mature erythroid cells. In contrast ribosome synthesis is low in primitive progenitors, whereas mature erythroid precursors have a very high rate of ribosome synthesis to meet the demand for globin synthesis. The illustration showing the timing of expression of erythroid transcription factors is a modified version of a figure by Anguita et al.88 Epo indicates erythropoietin; HSC, hematopoietic stem cell; GEMM, granulocyte/erythrocyte/macrophage/megakaryocute colony-forming unit; BFU-E, erythrocyte burst-forming unit; CD34, positive cell-surface marker for hematopoietic progenitor cells; CD38, negative cell-surface marker for primitive hematopoietic progenitor cells; CD71, transferrin receptor; GlyA, glycophorin A.
Normal and DBA erythropoiesis. (A) Adult erythropoiesis is a process by which single hematopoietic stem cells in the bone marrow differentiate and proliferate into billions of red blood cells. The figure shows a simplified scheme of the series of differentiation processes that takes place during red cell development. The main regulator of terminal erythropoiesis is Epo. Commonly used cell-surface markers that are used to enrich for the different progenitor populations are shown below the cells. (B) In patients with DBA the erythroid development is severely compromised. One convincing study localizes the erythroid defect to the Epo-dependent stages after the BFU-E stage.13 However, since there are reports of decreased BFU-E colony formation and decreased proliferation of multipotent progenitors in patients with DBA, it is possible that more primitive progenitors are affected as well.26 (C) The expression of RPS19 is high in primitive progenitor cells and decrease in more mature erythroid cells. In contrast ribosome synthesis is low in primitive progenitors, whereas mature erythroid precursors have a very high rate of ribosome synthesis to meet the demand for globin synthesis. The illustration showing the timing of expression of erythroid transcription factors is a modified version of a figure by Anguita et al.88 Epo indicates erythropoietin; HSC, hematopoietic stem cell; GEMM, granulocyte/erythrocyte/macrophage/megakaryocute colony-forming unit; BFU-E, erythrocyte burst-forming unit; CD34, positive cell-surface marker for hematopoietic progenitor cells; CD38, negative cell-surface marker for primitive hematopoietic progenitor cells; CD71, transferrin receptor; GlyA, glycophorin A.
To explain the role of insufficient RPS19 expression in DBA pathogenesis, it is important to first pinpoint the stage of erythroid failure in DBA. Ohene-Abuakwa et al13 suggested a defect in the terminal Epo-dependent erythroid maturation. In their study peripheral blood mononuclear cells from healthy donors and patients with DBA were compared in a 2-phase culture system.13 During the initial pre–Epo-dependant phase both normal and DBA-cell numbers declined 2-fold. When Epo was added for the second phase of culture, a wave of erythroid proliferation was seen in normal cells, whereas DBA cells failed to respond to Epo. Cells were also taken at the end of the pre–Epo-dependent culture and cultured in Epo containing semisolid medium. The number of erythroid colonies from healthy donors and patients with DBA were similar, whereas the colony size was dramatically smaller in the DBA cultures. This important observation strengthens earlier studies suggesting that the defect in DBA lies downstream of the colony-forming progenitors24,25 (Figure 2B). Seemingly in conflict with these data, RPS19 expression levels are high in primitive cells and progressively decrease in more mature cells such as erythroblasts.23,26,27 In addition, there may be a proliferative defect in more primitive hematopoietic progenitors because CD34+ CD38− multipotent progenitor cells from patients with RPS19-deficient DBA show a decreased proliferation rate in vitro, which can be corrected by RPS19 gene transfer.26
RPS19 deficiency and lack-of-function models
A DBA disease model is needed for evaluation of novel therapies and studies on molecular pathophysiology. Matsson et al28 attempted to create a murine model for RPS19-deficient DBA by targeted disruption of the Rps19 gene. However, the Rps19−/− homozygotes do not form blastocysts, and Rps19+/− heterozygous mice are viable but have a normal phenotype, displaying normal erythropoiesis. The RPS19 mRNA and protein expression levels are similar in Rps19+/+ and Rps19+/− mice.29 In these mice, which represent a single targeting event, a DBA phenotype does not develop such as in human patients with DBA. It is unclear why this single mouse strain fully compensates RPS19 expression from the remaining Rps19 allele. To create a mouse with anemia caused by RPS19 deficiency, different approaches are needed to generate a functional deficiency in RPS19. One such method is expression of short hairpin RNAs that specifically target and degrade RPS19 mRNA.30 Two studies using RNA interference (RNAi) to silence RPS19 expression in human CD34+ bone marrow (BM) cells showed that it is possible to induce a DBA phenotype in normal cells by reducing RPS19 expression. Importantly, the erythroid defect was rescued by expression of an RNAi-resistant RPS19 transcript, suggesting that an RNAi animal model can be used to evaluate effects of gene therapy.12,31 Analogous in vitro DBA models were created using erythroid leukemia TF-1 cell lines that harbor doxycycline-dependent RNAi-mediated RPS19 silencing.32 When induced to silence RPS19 expression, TF-1 cell proliferation decreased together with a marked reduction in the number of erythroid cells. These RPS19-deficient cell lines can greatly facilitate further molecular studies of DBA pathogenesis.33 Because RNAi-mediated RPS19 silencing can be used to create DBA phenotypes in human cells in vitro, this strategy may be a promising tool for creation of an appropriate RPS19-deficient mouse model for DBA.
Similarities to other ribosome-associated bone marrow failure disorders suggest a common link to the translational apparatus
DBA is the only known human disease caused by a deficiency of a ribosomal protein, which qualifies DBA into a small group of congenital bone marrow failure syndromes linked to nucleolus-associated processes and deficiencies in the translational machinery.34-36 The similarities between these bone marrow failure syndromes and DBA do not include isolated red-cell aplasia but rather resemblance in physical anomalies, growth retardation, and increased risk of cancer. The mutated SBDS gene in Shwachman-Diamond syndrome (SDS) codes for a nucleolus-associated protein,37 and phylogenetic profiling suggests a function in RNA metabolism and translation. Patients with SDS have neutropenia, mild anemia, increased risk of leukemia, and reduced numbers of CD34+ cells in the BM, skeletal abnormalities, and pancreatic insufficiency.38 Mutated dyskerin protein in X-linked dyskeratosis congenita (DKC) impairs maturation of ribosomal RNA (rRNA) and the RNA component of telomerase leading to increased cell mortality and subsequent BM failure. Although lymphoblastoid cell line studies ascribe the BM failure in DKC to malfunctioning telomerase activity,39 defective ribosomal biogenesis may contribute to DKC pathophysiology.34 Cartilage-hair hypoplasia (CHH) is a form of skeletal dysplasia leading to dwarfism.34 CHH is associated with hypoplastic hair, lymphopenia, anemia, and increased risk of malignancies. CHH is caused by mutations in the RMRP gene. The complex molecular pathogenesis in CHH involves failure in ribosomal assembly via defective endonucleolytic rRNA cleavage but also altered mRNA turnover and mitochondrial DNA replication.
Although not a bone marrow failure syndrome, Treacher-Collins syndrome (TCS) is another congenital disorder with a possible link to DBA pathophysiology because the craniofacial malformations seen in patients with TCS very much resemble those in patients with DBA and are caused by a defect in 18S rRNA methylation ultimately resulting from haploinsufficiency of the nucleolar phosphoprotein treacle.40
The individual gene products affected in DBA and the disorders mentioned in this section may have diverse functions throughout the cell; however, their functions also converge at the translational machinery. Therefore, we suggest that further attempts to understand DBA pathogenesis should naturally start with understanding the functional roles of RPS19 and RPS24 during ribosome assembly and translation.
Ribosomes and RPS19
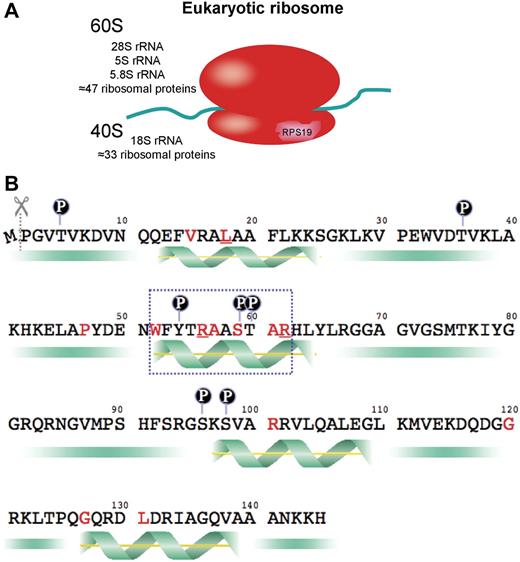
The ribosome is a very ancient and conserved catalytic machine responsible for translating the genetic code into polypeptides in all known forms of life. The mammalian ribosome is divided into a large (60S) and a small (40S) subunit, each composed of rRNA and ribosomal proteins (RPs). RPS19 is one of 33 RPs that together with the 18S rRNA constitutes the 40S ribosomal subunit (Figure 3A). Although the mammalian ribosome contains 80 ribosomal proteins, evidence indicates that the catalytic component translating information encoded in mRNA into polypeptides is RNA, not protein.41 RPs are suggested to have been added to the catalytic RNA backbone during evolution to improve ribosomal functions, such as pre-rRNA processing, ribosomal assembly and stability, intracellular trafficking, and translational efficiency and regulation.
The ribosome and RPS19. (A) The eukaryotic ribosome consists of ribosomal proteins and ribosomal RNA. The ribosome and its subunits are named by Svedberg units (S), which reflect the particles' sedimentation rate in an ultracentrifuge. The small subunit is named 40S, the large subunit 60S, and the complete ribosome 80S. The 40S subunit is a macromolecule composed by 18S rRNA together with 33 ribosomal proteins of which one is RPS19. (B) RPS19 consists of 144 amino acids because the first methionine is cleaved off. Amino acids predicted to be phosphorylated are labeled with a circled P. The 4 predicted α-helix structures are demonstrated by a green helix. Amino acids that are altered because of missense point mutations in patients with DBA are labeled with red letters. Amino acids mutated in multiple patients are red and underlined. A blue-dotted box marks the point mutation hotspot region.
The ribosome and RPS19. (A) The eukaryotic ribosome consists of ribosomal proteins and ribosomal RNA. The ribosome and its subunits are named by Svedberg units (S), which reflect the particles' sedimentation rate in an ultracentrifuge. The small subunit is named 40S, the large subunit 60S, and the complete ribosome 80S. The 40S subunit is a macromolecule composed by 18S rRNA together with 33 ribosomal proteins of which one is RPS19. (B) RPS19 consists of 144 amino acids because the first methionine is cleaved off. Amino acids predicted to be phosphorylated are labeled with a circled P. The 4 predicted α-helix structures are demonstrated by a green helix. Amino acids that are altered because of missense point mutations in patients with DBA are labeled with red letters. Amino acids mutated in multiple patients are red and underlined. A blue-dotted box marks the point mutation hotspot region.
Mammalian ribosomes are suggested to be quite heterogeneous macromolecules, capable of changing properties and thereby selectively regulating mRNA translation.42 One difference between ribosomes can be the phosphorylation state of its RPs, where the best-known example is phosphorylation of RPS6 in proliferating cells. RPS6 phosphorylation increases translational efficiency to meet the increased protein demand in proliferating cells.43 There is also a ribosomal difference between men and women because the X and Y chromosomes contain different versions of the RPS4 gene.44 Although it is widely believed that a single gene encodes each RP in mammals, the human genome contains more than 2000 RP pseudogenes and 16 duplicated RP genes,45 of which some may be translated under certain conditions. One example of such differential RP utilization is the expression of different RPS19 isoforms in oocytes and somatic cells of Ascaris lumbricoides.44 Several RP isoforms can also be expressed from the same gene by alternative mRNA splicing. One example is the preferential expression of an mRNA splice variant encoding a 130–amino acid RPS24 isoform in human primitive hematopoietic progenitor cells, whereas differentiated cells express more of a transcript encoding a 133–amino acid RPS24 isoform.4 Some RPs have extra ribosomal functions such as RPL13a, which is phosphorylated on IFN-γ stimulation and thereby released from the ribosome. The released RPL13a specifically binds to ceruloplasmin mRNA to inhibit translation of this acute-phase protein, whereas the overall protein synthesis rate appears unaffected by the loss of ribosome-bound RPL13a.46
RPS19 is 1 of 4 RPs of the 40S subunit that have homologs in eukaryote and archaebacterial ribosomes, but not in the eubacterial ribosome.47 Because RPS19 does not have a homolog in the well-characterized eubacterial ribosome, little is known about its function or structure. Immunoelectron microscope studies locate RPS19 to the external surface of the 40S subunit,48 where it is in close vicinity to RPS3a, RPS13/16, and RPS24, a region that interacts with eIF-2 during ribosomal scanning and translation initiation.49 RPS19 is a very conserved protein, and only a single amino acid has changed since rodents and primates diverged 100 million years ago. Two nontranscribed RPS19 pseudogenes are described in humans and one in mice.50,51 Human RPS19 mRNA codes for a 145–amino acid protein; however, the number of residues is reduced to 144 by post-transcriptional removal of the NH2-terminal methionone.52 The human RPS19 gene product is a basic protein, lacking cysteine residues.53 Structure prediction software analysis predicts human RPS19 to have 4 alpha-helix secondary structures,53 and at least 7 amino acids are predicted as possible phosphorylation sites by prediction software analysis, although phosphorylation has not been demonstrated under physiologic conditions54 (Figure 3B).
To reveal the function of RPS19 it is of great importance to characterize other proteins that interact with RPS19. As might be expected, cross-linking studies of 40S subunits in yeast reveal binding to several other RPs.55 Perhaps a more interesting binding partner is the nucleolar ribosome biogenesis protein, Nep1p, that binds 18S rRNA and possibly interacts with RPS19 during formation of preribosomal 40S particles in yeast.56 Another interesting RPS19-interacting protein is fibroblast growth factor-2, an important regulator of rRNA transcription,57 which interacts with a pool of free RPS19 in vitro.58 This suggests that free extraribosomal RPS19 might play a role in the signaling pathways that regulate rRNA transcription. RPS19 is also reported to interact with S19BP, a nucleolar protein with an unknown function,59 and the serine-threonine kinase PIM-1.60 The main hematologic finding in PIM-1–deficient mice is decreased erythrocyte size, whereas transgenic mice overexpressing PIM-1 exhibit an increase in MCV.61 RPS19/PIM-1 interaction in vitro leads to phosphorylation of RPS19. Interestingly, the most common missense mutations are located between amino acids 52 and 62, a region that contains both a serine and a threonine residue predicted to be phosphorylated by serine-threonine kinases (Figure 3B). This DBA point mutation hotspot region is highly conserved and is likely to be important for protein function, suggesting that PIM-1–mediated serine-threonine phosphorylation may be important for RPS19 function.
In human cells the highest concentration of RPS19 is within the nucleolus,62 the site of ribosome biogenesis. Interestingly, some patients with DBA have a mutation in the nucleolar localization signals located in the 15N-terminal or the 22 C-terminal amino acids of RPS19, causing impaired nucleolar localization of the mutated protein.62
As most if not all RPs, RPS19 interacts with rRNA, and it is predicted to bind to helix 45 of the 18S rRNA.56 Although this RPS19-18S rRNA interaction is not yet physically confirmed, RPS19 has been found to play a pivotal role in 18S rRNA maturation and 40S ribosomal subunit assembly. In RPS19-deficient yeast cells and human HeLa cells pre-40S subunits containing incompletely processed 18S rRNA accumulate in the nucleus, with a corresponding decrease in the amount of mature 40S subunits in the cytoplasm.63,64 A similar defect in 18S rRNA maturation and 40S biogenesis is seen in RPS19-deficient human hematopoietic TF-1 cell lines and RPS19-deficient and DBA patient BM cells.33 The 18S rRNA maturation defect causes a larger 21S precursor to accumulate in the cells. Because quantitative real-time polymerase chain reaction cannot distinguish mature 18S from the accumulated 21S precursor rRNA, the 3.5- to 7-fold increase of 18S rRNA seen in BFU-E cells from patients with RPS19-deficient DBA65 may be explained by high amounts of accumulated 21S precursor rRNA. The final maturation step of the 18S rRNA completes the 40S particle and enables initiation of translation; thus, RPS19-deficient cells suffer from a relative 40S subunit deficiency and have a reduced capacity for translation initiation.
Even though RPS19 is a part of the translational apparatus, it cannot be ruled out that RPS19 has a separate role outside the ribosomal complex. RPS19 dimers have been shown to be a chemotactic factor for monocytes, suggesting that the protein indeed has some extraribosomal functions.66
Possible molecular mechanisms of erythroid failure caused by RPS19 deficiency
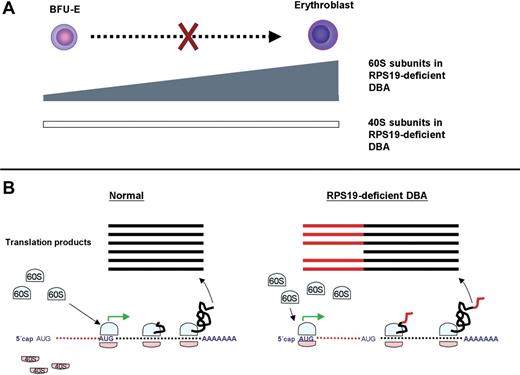
During vertebrate evolution the organism's demand for oxygen has forced erythroid development into becoming a tightly regulated and very dynamic process that ensures tissue oxygenation even after massive bleedings and nutritional deficits. To maintain physiologic erythrocyte levels the organism needs to express correct levels of specific proteins in certain cells at the right time. The regulation of gene expression therefore must extend beyond simply adjusting levels of mRNA transcription into also affecting the rate and start point of translation initiation. In RPS19-deficient DBA, the impaired 40S ribosomal subunit biogenesis together with the link to other ribosome-associated disorders point toward a disturbance of this second dimension of gene regulation as the mechanism that causes anemia, congenital anomalies, and increased risk of malignancy in DBA. In line with this theory global gene expression analysis shows a down-regulation of multiple ribosomal genes, as well as several genes, required for translation initiation and elongation, in RPS19-deficient DBA patient BFU-E cells compared with normal controls.65 Figure 4 illustrates a summary of known RPS19 actions and possible links between RPS19 and translational regulation.
Actions of RPS19. The illustration summarizes the known functions and interactions of RPS19. RPS19 is reported to interact with PIM-1, Nep1p, S19BP, FGF-2, and eIF-2α, as well as being phosphorylated in vitro. RPS19 is required for 18S rRNA and 40S subunit maturation. Most of the suggested functions of the RPS19 protein are within the translational machinery.
Actions of RPS19. The illustration summarizes the known functions and interactions of RPS19. RPS19 is reported to interact with PIM-1, Nep1p, S19BP, FGF-2, and eIF-2α, as well as being phosphorylated in vitro. RPS19 is required for 18S rRNA and 40S subunit maturation. Most of the suggested functions of the RPS19 protein are within the translational machinery.
We propose several hypotheses that may link DBA pathogenesis to functions of the 40S ribosomal subunit. These possible molecular explanations for failure of erythroid development are not mutually exclusive, and more than one of the proposed mechanisms may be acting in concert.
Erythroid progenitor-specific stoichiometric failure in 40S synthesis
One simple explanation as to why erythroid development is specifically affected by RPS19 deficiency may reflect a cell-specific acute deficiency of RPS19 (Figure 5A). This theory is based on the discrepancy between the high expression of RPS19 in primitive cells and the demand of ribosome biogenesis, which is low in primitive cells and increases in the proerythroblasts, to allow massive globin synthesis in their progeny (Figure 1). In patients with DBA these conditions may cause a tissue-specific stoichiometric failure in ribosome synthesis,36 whereby RPS19 is limiting in specific cells. During erythropoiesis, the impact of the RPS19 deficiency may become most limiting in proerythroblasts because they express low levels of RPS19, while the demand for ribosome biogenesis is high. These cells are then unable to compensate for the haploinsufficient RPS19 expression in patients with DBA. Insufficient 18S rRNA and 40S biogenesis in erythroid precursors might then trigger a p53-mediated cell-cycle arrest or apoptosis67 or fail to differentiate properly because of dysregulated translation.
Hypotheses linking 40S deficiency to anemia. (A) The erythroblast normally produces exceptionally high amounts of ribosomes. Erythroid development may come to a halt at the erythroblast stage in 40S-deficient cells, because they will have difficulties to meet the high demand of ribosome biogenesis. The relative 40S deficiency is expected to be most severe at this arrested stage of erythroid development. (B) Several transcription factors can be translated from alternative translation initiation sites in the 5′ untranslated region. A 40S subunit deficiency may cause translation from alternative translation initiation sites and produce protein isoforms with unwanted characteristics.
Hypotheses linking 40S deficiency to anemia. (A) The erythroblast normally produces exceptionally high amounts of ribosomes. Erythroid development may come to a halt at the erythroblast stage in 40S-deficient cells, because they will have difficulties to meet the high demand of ribosome biogenesis. The relative 40S deficiency is expected to be most severe at this arrested stage of erythroid development. (B) Several transcription factors can be translated from alternative translation initiation sites in the 5′ untranslated region. A 40S subunit deficiency may cause translation from alternative translation initiation sites and produce protein isoforms with unwanted characteristics.
Cells that contribute to erythroid failure in RPS19-deficient DBA have the most severe 40S deficiency
It will be important to more thoroughly pinpoint the stage of the erythroid defect in DBA erythropoiesis. On the basis of the assumption that DBA is caused by a relative 40S subunit deficiency, one might be able to determine the stage of erythroid development that is most prominently affected in DBA by sorting out different hematopoietic/erythropoietic-cell populations and determine which cell population that has the lowest 40S/60S ratio.
Deficiency of 40S subunits leads to altered polysome recruitment of specific mRNAs important for erythroid development
The 40S subunit together with initiation factors and Met-tRNA forms a 43S complex that scans the 5′ untranslated region (5′-UTR) of mRNAs. Depending on availability of 40S subunits68 and the other constituents of the 43S complex, mRNAs with different 5′-UTR characteristics are translated.69 A decrease in the 40S/total mRNA ratio may alter the relative proteome of the cell, because the protein output will preferentially decrease from transcripts with low translation initiation constants.68 DBA cells deficient of 40S subunits may recruit a different set of mRNAs to polysomes than healthy cells, suggesting that altered polysome recruitment possibly contributes to DBA pathogenesis.
Deficiency of 40S subunits affects the ratio of different transcription factor isoforms that are translated from transcripts with alternative in-frame translation initiation sites
Alternative translation initiation sites are found in mRNAs of several transcription factors and enable translation of different transcription factor isoforms, depending on the abundance of translation factors in the cell (Figure 5A). In humans 5 isoforms of the growth factor FGF-2 are produced by alternative initiation of translation.57 Interestingly, the smallest 18-kDa FGF-2 isoform, which is the only isoform translated from a standard Kozak AUG start codon, is shown to bind to RPS19 and also to stimulate rRNA transcription. A deficiency of 40S subunits may change the FGF-2 isoform ratio in the cell because of a decreased rate of translation initiation.
The transcription factor C/EBPα is translated into a short product in cells with high levels of eIF4E and eIF2α and a longer version in cells with low translation activity.70 Dysregulation of this translational control is part of AML pathogenesis.
Another transcription factor, GATA1, is similarly translated into 2 isoforms.71 The full-length GATA1 isoform is required for normal human erythroid development, and patients with mutations in GATA1 that result in translation of only the short GATA1 isoform develop macrocytic anemia.72
During commitment into the erythroid lineage translation of the transcription factor SCL is switched to a shorter isoform.69,73 Expression of the short SCL isoform is increased when increased activation of translation initiation changes the initiation site preference to the downstream in-frame AUG codon. Conversely, a low rate of translation initiation, as in elF2- and elF4E-deficient cells, does not allow expression of the short SCL isoform, suggesting that translation of the short isoform will be compromised in 40S-deficient cells interfering with erythroid lineage commitment.
Together these examples reflect the importance of usage of the correct translation initiation sites during translation of transcription factors. It will be important to investigate whether disturbed usage of alternative in-frame translation initiation sites contributes to the anemia and increased risk of leukemia in RPS19-deficient DBA.
Phosphorylation of RPS19 is a specific regulator of translation in a similar way as phosphorylation of RPS6 and RPL13a
Phosphorylation of RPs is a way to regulate cell cycle and proliferation.43,46,74 The best-characterized phosphoprotein in the mammalian ribosome is S6, which has 5 seryl residues at the carboxyl terminus that are phosphorylated after various stimuli leading to an increase in translation. Even though disturbed phosphorylation of RPS19 is an unlikely pathogenic mechanism in patients with DBA without mutations in RPS19, it will be interesting to follow up the hypothesis that Epo/STAT5 signaling induces expression of PIM-1, which forms a complex with RPS19 leading to phosphorylation and activation of the protein.60 If phosphorylation of RPS19 is a downstream target of Epo signaling, a defect could lead to decreased erythroid precursor proliferation.
Erythroid development is disturbed by the same mechanism in both RPS24-deficient and RPS19-deficent DBA patients
The exiting recent discovery that RPS24 is mutated in 2% of patients with DBA4 leads one to propose that the common pathogenic mechanism in DBA may involve deficiencies in ribosomal proteins that affect biogenesis of the 40S ribosomal subunit. Detailed functional studies of RPS24 are required to address this hypothesis. It will be interesting to investigate how RPS24 deficiency affects 18S rRNA maturation, 40S subunit biogenesis, translational regulation, and erythroid development.
Development of future therapies
Once the molecular mechanism of the various genetic types of DBA is better understood, specific and clever designs of novel small-molecule therapies for DBA may be possible. Despite the lack of insight into the precise molecular mechanism of DBA, several experimental therapies have been reported to benefit erythropoiesis in patients with DBA, for example, the immunomodulating drugs cyclosporine75 and the CD20 antibody rituximab,76 the anticonvulsant valproic acid,77 the erythroid progenitor-stimulating cytokine IL-3,78 and the prolactin-releasing drug metoclopramide.79 At present, however, corticosteroid therapy remains as the only evidence-based pharmacologic treatment of DBA.
Because patients with RPS19-deficient DBA can be cured by stem-cell transplantation from a healthy donor, they can also potentially be cured by gene therapy of the patient's hematopoietic stem cells followed by transplantation of the corrected cells. Preclinical in vitro experiments using γ retrovirus-mediated RPS19 transgene overexpression in CD34+ RPS19-deficient DBA cells showed a 3-fold increase in BFU-E formation.23 Lentivirus-mediated RPS19 gene transfer in addition to correcting the erythroid development of DBA cells also improved the proliferative defect of CD34+ CD38− primitive progenitor cells in vitro.26 If the correction of the proliferative defect in primitive progenitors holds true also in vivo, it is possible that it may be sufficient to correct only a fraction of the patients' stem cells to achieve a therapeutic benefit. Although preliminary, these results are very encouraging and demonstrate that gene replacement therapy of DBA may be feasible and lead to a permanent cure for patients with transfusion-dependent DBA. The crucial experiments that are needed to bring gene therapy from the laboratory to the clinic depend on the generation of proper animal models for RPS19-deficient DBA to ask whether gene transfer can correct the DBA phenotype.
Development of a human gene therapy protocol for RPS19-deficient DBA will face a number of fundamental challenges, including high enough gene transfer efficiency and transgene expression for sufficient therapeutic benefit and the development of safe vectors with minimal risks for insertional oncogenesis.80,81 In successful gene therapy trials for X-linked severe combined immunodeficiency (X-SCID), a lasting therapeutic benefit has been achieved in the majority of the 17 treated patients.82-85 However, 3 of the patients developed T-cell leukemia, probably, at least in part, as a result of insertional mutagenesis because of vector integration in the LMO2 gene encoding a transcription factor that is highly expressed during early T-cell development. However, these complications have only been reported in a minority of patients with X-SCID treated by gene therapy, and 2 additional disorders, adenosine deaminase–deficient SCID and chronic granulomatous disease, have been treated successfully by gene therapy.86,87 The 3 cases of insertional mutagenesis have emphasized the need to develop safer gene transfer vectors to minimize risks. For development of efficient and safe gene therapy of RPS19-deficient DBA, self-inactivating vectors, possibly containing chromatin insulators to minimize the risks and effects of insertional mutagenesis, will have to be developed and tested in a proper animal model for DBA. In the next 5 years, advances can be expected in the generation of proper animal models for DBA and the development of safe and effective vectors to correct the erythroid defect by gene transfer. Hopefully, these efforts will gradually lead to the development of a cure for RPS19-deficient DBA.
Conclusion
All patients with DBA, irrespective of the genetic mutation, have a similar disease phenotype. Therefore, the mutations in RPS19, RPS24, and the other unknown DBA genes may affect the same molecular pathways that lead to defects in erythroid development. On the basis of the assumption that DBA is a disease of the 40S subunit, attempts to identify the remaining DBA genes should include a thorough analysis of the other genes coding for proteins of the small ribosomal subunit. Once the genetic defects have all been identified and the molecular pathogenesis is better understood, animal models can be developed to test new curative therapies for all forms of DBA.
Authorship
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Correspondence: Johan Flygare, Molecular Medicine and Gene Therapy, Institute of Laboratory Medicine and The Lund Strategic Research Center for Stem Cell Biology and Cell Therapy, Lund University, BMC A12, 221 84, Lund, Sweden; e-mail: johan.flygare@med.lu.se; and Stefan Karlsson, Molecular Medicine and Gene Therapy, Institute of Laboratory Medicine and The Lund Strategic Research Center for Stem Cell Biology and Cell Therapy, Lund University, BMC A12, 221 84, Lund, Sweden; e-mail: stefan.karlsson@med.lu.se.
Acknowledgments
We thank Dr Ann Brun for scientific and artistic help with the design of the figures and Dr Steven R. Ellis for sharing his knowledge about ribosomal biogenesis, stimulating discussion, and comments on the manuscript. Finally, we thank Marie and Manny Arturi and the Daniella Maria Arturi Foundation for facilitating scientific communication within the DBA scientific community.
This work was supported by grants from The Swedish Cancer Society (S.K.), The European Commission (CONSERT) (S.K.), The Swedish Gene Therapy Program (S.K.), The Diamond-Blackfan Anemia Foundation (S.K.), The Swedish Medical Research Council (S.K.), The Swedish Children Cancer Foundation (S.K.); by a Clinical Research Award from Lund University Hospital (S.K.); by the Ronald McDonald Foundation (J.F.) and the Royal Physiographic Society in Lund (J.F.). The Joint Program on Stem Cell Research was supported by the Juvenile Diabetes Research Foundation and the Swedish Medical Research Council. The Lund Stem Cell Center is supported by a Center of Excellence grant in life sciences from the Swedish Foundation for Strategic Research.



This feature is available to Subscribers Only
Sign In or Create an Account Close Modal