Abstract
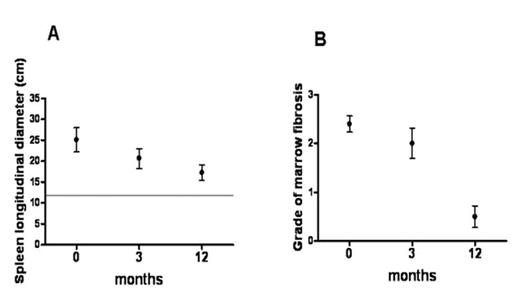
Allogeneic stem cell transplantation has been shown to restore normal hematopoiesis in patients with intermediate or high risk primary myelofibrosis (PMF) or myelofibrosis preceeded by polycythemia vera or essential thrombocythemia. However, in patients with PMF and extensive splenomegaly it is not clear whether transplant is associated with an unacceptable risk or if splenectomy should be performed prior to transplant. In this study, ten consecutive patients with myelofibrosis who were not splenectomized received an allogeneic hematopoietic stem cell transplantation (HSCT) from related or unrelated donors and were periodically monitored by ultrasound or CT scan for 12 months after transplant to assess the kinetics of the reduction of splenomegaly. These findings were correlated with the time to resolution of marrow fibrosis, time to engraftment and clinical outcome. Over a 12 month period a progressive reduction in spleen size was observed in all the patients and paralleled the reduction in marrow fibrosis (Figure 1). Of 10 patients, 5 with a splenic longitudinal diameter >30 cm showed a more prolonged time to engraftment ANC> 0.5 × 109/L (d 19±5 vs 13±2, p=0.05) and platelet > 20 × 109/L (d 75±104 vs 11±2, p=0.06). However, of the 5 patients with more extensive splenomegaly only 2 experienced delayed engraftment of platelets (d 77 and 256, respectively). Full donor chimerism was observed in all patients within 60 days after transplantation regardless of the size of the spleen. At a median follow-up of 54 months (range: 2–80) all the patients are alive but 1 who died of a TTP like syndrome 2 months after transplant and had a small spleen at the time of transplant. A clinical CR has been documented in 7 patients and 2 have achieved clinical improvement as assessed by IWG response criteria. These findings suggest that allogeneic HSCT with RIC regimen can be safely performed in patients with extensive splenomegaly. Although in these patients the time to engraftment may be prolonged, the significant risk of morbidity and mortality associated with splenectomy may be avoided.
Author notes
Disclosure: No relevant conflicts of interest to declare.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal