Abstract
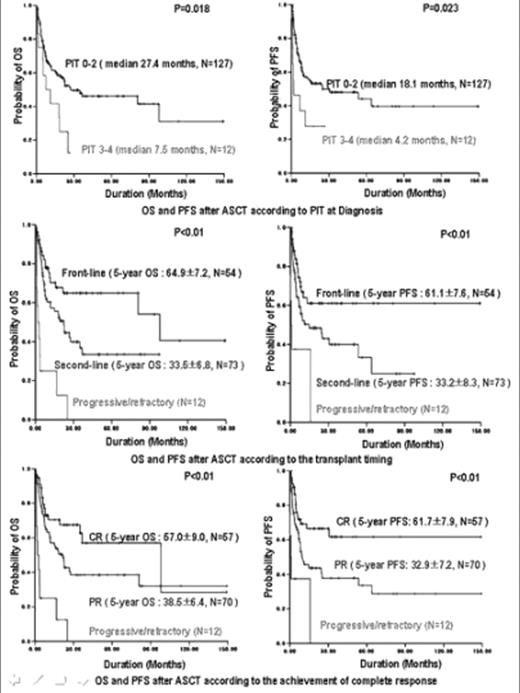
Peripheral T cell lymphoma (PTCL) is a heterogenous group of aggressive lymphoma, which T-cell phenotype itself associated with unfavorable prognostic factors when compare to patients with B-cell phenotype lymphoma. High-dose chemotherapy (HDT) followed by autologous stem cell transplantation (ASCT) has represented a rescue option from poor prognosis. We retrospectively investigated the clinical outcomes of ASCT in 139 Korean patients with PTCL between December 1994 and June 2007. The overall survival (OS) and progression-free survival (PFS) were measured from the date of transplantation and were estimated using the Kaplan-Meier method. The median age at transplantation was 41 years. The histological subtypes had 45.3% PTCL-unspecified, 13.7% anaplastic large cell (ALK +/−: 15.7/57.8%), 10.8% angioimmunoblastic T cell, 21.6% extranodal NK/T cell, and 8.6% others. Disease status at transplantation consisted of 54 patients (38.8%) with first complete response (CR)/partial response (PR), 58 patients (41.7%) with chemosensitive-relapsed CR/PR, 15 patients (10.8%) with refractory CR/PR and 12 patients (8.6%) with progressive or refractory. At a median follow-up of 29.3 months, the 5-year probability of OS and PFS was 42.3±4.9% and 42.2±5.9%, respectively. The 5-year OS and PFS rates in patients with 1st CR/PR were 64.9±7.2% and 61.1±7.6%, compared to those in patients with chemosensitive-relapsed and refractory CR/PR were 33.5±6.8% and 33.2±8.3%, respectively. Early transplant-related mortality was 10.1%. Histological subtypes, bulky (≥10cm), prognostic index for PTCL (PIT) at diagnosis (0–2 vs 3–4), age-adjusted IPI at diagnosis, disease status at transplantation, the transplant timing (front-line vs second-line) and conditioning regimen were significant differences of survivals in univariate analysis. PIT, the transplant timing and the achievement of CR before transplantation were the variable prognostic for OS and PIT, bulky, and the achievement of CR provided significant independent factors for PFS in multivariate analysis. Our data showed that patients with PTCL who had low PIT and achieved CR before ASCT improved the OS and PFS regardless of the transplant timing and front-line ASCT of primary chemosensitive patients was effective in the OS.
Author notes
Disclosure: No relevant conflicts of interest to declare.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal