Abstract
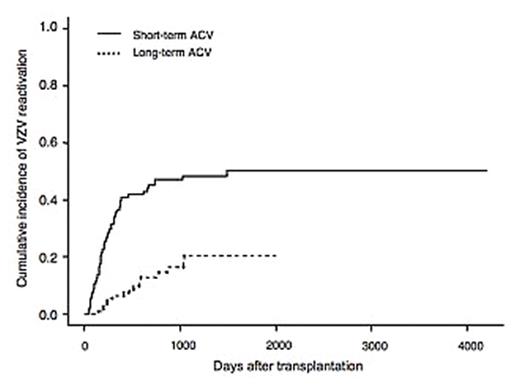
Varicella-zoster virus (VZV) infection remains a common complication after hematopoietic stem cell transplantation (HSCT). The introduction of long-term prophylaxis with low-dose acyclovir against VZV reactivation has been investigated, because VZV-related complications including post-herpetic neuralgia and secondary infection significantly affect the patient’s quality of life. We started long-term oral acyclovir at 200 mg/day in July 2001. Acyclovir was continued until the end of immunosuppressive therapy and at least one year after transplantation. To evaluate the efficacy of this long-term prophylaxis with ultra low-dose acyclovir against VZV reactivation, we analyzed the records of 242 Japanese adult patients who underwent allogeneic HSCT for the first time from June, 1995 to November, 2006 at University of Tokyo Hospital. Sixty-six patients developed VZV reactivation at a median of 248 days after HSCT, with a cumulative incidence of 34.7%. There was no VZV-related death. Only one breakthrough reactivation occurred during long-term acyclovir, responding well to the therapeutic dose of valacyclovir. The use of long-term acyclovir was the only independent determinant that significantly decreased the overall incidence of VZV reactivation (20.4% vs 50.5%, P<0.0001). As for VZV-related complications, only post-herpetic neuralgia was seen in three patients with long-term prophylaxis, whereas serious complications including CNS involvement, motor neuropathy and ophthalmic complications were involved in 14 without long-term prophylaxis. Eleven of 16 patients with long-term prophylaxis were treated as outpatients, whereas 39 of 50 patients without long-term prophylaxis required hospitalization (hospitalization 31% vs 78%, P=0.0015). Fifteen of the 57 patients who discontinued long-term acyclovir developed VZV reactivation at a median of 147 days after the discontinuation of acyclovir, with a cumulative incidence of 32.1%. VZV reactivation following discontinuation predominantly occurred in patients who were receiving immunosuppressive therapy at the cessation of acyclovir (44% vs 20%, P=0.12). These findings suggest that long-term prophylaxis of ultra-low-dose acyclovir resulted in a successful prevention of severe VZV-related symptoms and death, with a significantly decreased overall incidence of VZV reactivation. With this prophylaxis, visceral dissemination and serious complications other than post-herpetic neuralgia were completely eliminated, and thereby need for hospitalization was significantly reduced. To continue acyclovir for patients with profound immunosuppression might be important to further decrease the overall incidence of VZV reactivation.
Author notes
Disclosure: No relevant conflicts of interest to declare.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal