Abstract
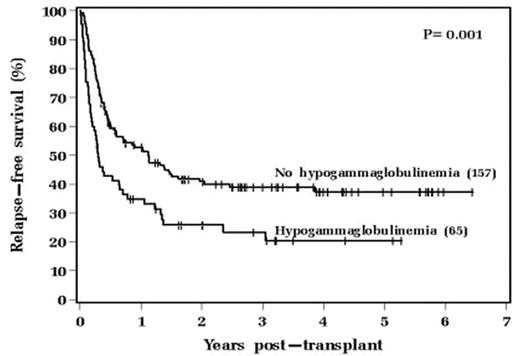
Hypogammaglobulinemia (HG) may increase the risk of infection after AHSCT. However, whether pre-transplant HG influences other outcomes after AHSCT is less certain. We therefore investigated the effect of pre-transplant serum immunoglobulin (Ig) levels on non-infectious post-transplant outcomes. From January 2001 to April 2007, 287 AHSCTs were performed at our institution. For the current analysis 65 were excluded (15 no baseline Ig data, 13 cord blood transplant, 3 <16 yrs of age, 26 with <8/8 HLA match, 8 2nd AHSCT). The median age was 43 yrs (range, 16–65), 119 (54%) were males, 90% were Caucasian, 148 had myeloid diseases (AML most common, 46%), 68 had lymphoid diseases (ALL most common, 19%) and median time from diagnosis to AHSCT was 6.4 mos (range, 0.2–106). The most common preparative regimen was busulfan/cyclophosphamide(Bu/Cy)-based (70%) followed by total body irradiation (TBI)-based conditioning. There were 134 (60%) matched related and 88 (40%) 8/8 HLA matched unrelated donors. HG was defined as serum Ig levels less than the normal ranges (NR) for IgG (717–1411 mg/dL), IgM (55–334 mg/dL) and IgA (78–391 mg/dL). The median pre-transplant Ig levels were IgG 953 (range, 18–2710) with 65 (29%) patients (pts) <NR; IgM 60 (range, 3–1160) with 101 (46%) pts <NR; IgA 160 (range, 12–769) with 40 (18%) pts <NR. Univariable and multivariable associations between pre-transplant HG and outcomes were assessed using Kaplan-Meier analysis and Cox proportional hazards analysis, respectively. HG was not found to correlate with CMV reactivation, other infections, graft rejection, acute or chronic GVHD. However, relapse was higher for pts with low baseline IgG (p=0.032) and IgM levels (p=0.07). In addition, both overall (OS) and relapse-free survivals (RFS) were significantly worse for those patients with baseline HG. This finding was most significant for those with low IgG levels (OS p=0.007 [Figure]; RFS p=0.001), then for those with low IgM levels (OS p=0.018; RFS p=0.016), and least for those with low IgA levels (OS p=0.017; RFS p=0.043). On multivariable analysis diagnosis, prior radiation therapy and a Bu/Cy/VP16 preparative regimen were prognostic for inferior OS and RFS, while low baseline IgG level was prognostic only for inferior RFS (p=0.05). We conclude that pre-transplant HG due to low IgG is correlated with inferior survival after AHSCT. The routine administration of prophylactic intravenous immunoglobulin until at least day +100 post-transplant for our pts may in part account for the lack of increased post-transplant infections in those with baseline HG. Low pre-transplant IgG levels may be of prognostic importance to identify pts who may be less likely to achieve graft-vs-malignancy responses and who may benefit from further treatment intensification strategies in order to improve post-transplant outcomes.
Author notes
Disclosure: No relevant conflicts of interest to declare.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal