Background: Primary amyloidosis (AL) is characterized by multi-organ deposition of light chain derived amyloid protein, resulting in organ dysfunction of varying severity. High dose chemotherapy and autologous stem cell transplantation (ASCT) is an effective treatment for AL, but is limited in applicability due to high transplant related mortality in patients with advanced organ dysfunction. Serum LDH, an enzyme that catalyzes the conversion of lactate to pyruvate, is present in large amounts in heart, kidney, liver, and muscle and is elevated with abnormalities in one or more of the organs. It is commonly elevated in a variety of hematologic malignancies. Given the multi-organ involvement in AL, we examined the prognostic value of LDH in AL.
Methods: We examined our transplant database to assess the prognostic value of LDH. Laboratory values from pre-ASCT evaluation were used for the analysis.
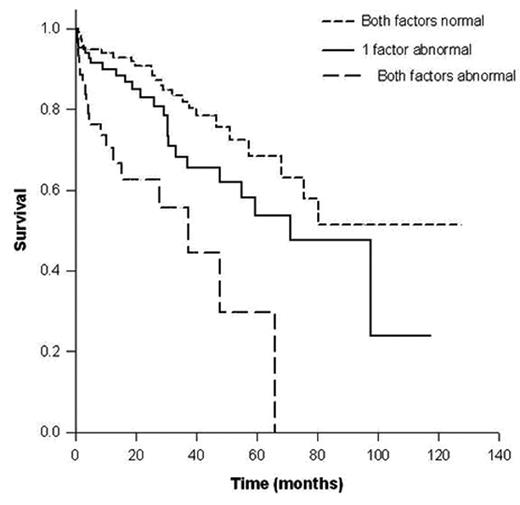
Results: Three hundred and thirteen pts who underwent ASCT between March 1997 and March 2007 were included in this analysis. The median age at ASCT was 57.5 years (range, 33–73); and 183 pts (58.3%) were male. The median duration from diagnosis to transplant was 4.1 months (range, 1–75) and the median follow up post transplant was 28.3 months (range, 1 m to 10 years) for the 229 pts (73%) alive at the time of analysis. The median LDH was 194 IU (range, 92-441) and 138 pts (44%) had an LDH > 200. The median overall survival post-ASCT for patients with an LDH > 200 was 59.4 mos (95% CI; 37.9, 80.8) compared to not reached for the rest (Figure). The prognostic value of LDH for post transplant OS was independent of cardiac troponin (cTnT). The median OS post ASCT for patients with cTnT > 0.035 (n=208) was 37.4 months (95% CI; 17, 57.9) compared to 97.5 months (95% CI; 64.8, 130.2) for the rest. In a Cox proportional hazards model, cTnT > 0.035 was associated with a 2.5 fold risk of death (p = 0.0013) and an LDH > 200 was associated with 1.7 fold risk (p = 0.04). We then examined if LDH added to the cTnT in a prognostic model for survival post ASCT. Pts with both cTnT < 0.035 and LDH < 200 (n=133) had a median OS that was not reached compared to 71 mos (95% CI; 48.3, 94) if one factor was abnormal (n=89) and 37.4 mos (95% CI; 16.1, 58.8) if both cTnT and LDH were abnormal as above (n=45); p < 0.001 (Figure 2).
Conclusions: In this study we have demonstrated the prognostic value of serum LDH in AL pts undergoing ASCT. Serum LDH appears to add to the value of troponin in prognostic staging of these patients. These results need to be examined in a larger cohort of patients undergoing different treatments. It is possible that LDH is able to globally assess abnormalities of multiple organs including heart, liver and lung. Prospective studies looking at the different LDH fractions are ongoing.
Disclosure: No relevant conflicts of interest to declare.


This feature is available to Subscribers Only
Sign In or Create an Account Close Modal