Abstract
Introduction: Mortality rates associated with stem cell transplantation are considerably higher than those of autologous stem cell transplantation for other hematologic malignancies. The efficacy of stem cell transplantation in amyloidosis largely is determined by treatment-related mortality rates (range, 11%-25%). Appropriate patient selection is essential to avoid this high mortality rate.
Patients & Methods: The primary end point of the study was death from any cause between 4 days before transplantation and d+100 after transplantation. Patient characteristics are shown.
Patient characteristics (N=271)
| Characteristic . | Median (range) . | Comment . |
|---|---|---|
| Age, y | 58 (33–75) | |
| Male | 159 (59%) | |
| Renal involvement | 184 (68%) | |
| Cardiac involvement | 147 (54%) | |
| Peripheral neuropathy | 30 (11%) | |
| Hepatic involvement | 28 (14%) | |
| Albumin, g/dL | 2.8 (0.8–4.4) | |
| Creatinine, mg/dL | 1.1 (0.6–12.0) | 90% of patients had levels ≤1.7 mg/dL |
| Alkaline phosphatase, U/L | 93 (31–1,395) | 25% of patients had levels >132 U/L |
| Urinary total protein, g/d | 3.35 (0.01–35.4) | |
| Percentage of plasma cells in the marrow | 7 (0–78) | 90% of patients had <17% plasma cells |
| Interventricular septal thickness, mm | 13 (7–25) | |
| Ejection fraction, % | 65 (28–84) | |
| Time between diagnosis and stem cell transplantation, mo. | 4 (0.8–75) | |
| Troponins,μg/L | 0.01 (0.01–1.0) | 75% of patients had levels ≤0.03 g/L |
| 90% of patients had levels ≤0.08 g/L |
| Characteristic . | Median (range) . | Comment . |
|---|---|---|
| Age, y | 58 (33–75) | |
| Male | 159 (59%) | |
| Renal involvement | 184 (68%) | |
| Cardiac involvement | 147 (54%) | |
| Peripheral neuropathy | 30 (11%) | |
| Hepatic involvement | 28 (14%) | |
| Albumin, g/dL | 2.8 (0.8–4.4) | |
| Creatinine, mg/dL | 1.1 (0.6–12.0) | 90% of patients had levels ≤1.7 mg/dL |
| Alkaline phosphatase, U/L | 93 (31–1,395) | 25% of patients had levels >132 U/L |
| Urinary total protein, g/d | 3.35 (0.01–35.4) | |
| Percentage of plasma cells in the marrow | 7 (0–78) | 90% of patients had <17% plasma cells |
| Interventricular septal thickness, mm | 13 (7–25) | |
| Ejection fraction, % | 65 (28–84) | |
| Time between diagnosis and stem cell transplantation, mo. | 4 (0.8–75) | |
| Troponins,μg/L | 0.01 (0.01–1.0) | 75% of patients had levels ≤0.03 g/L |
| 90% of patients had levels ≤0.08 g/L |
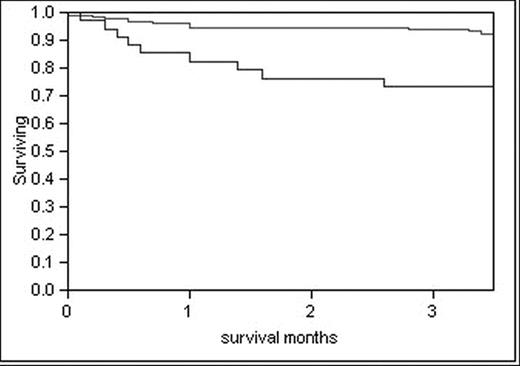
Results: Among 271 patients undergoing stem cell transplantation, troponin T was a powerful predictor of treatment-related mortality. Patients with troponin levels of 0.06 mg/L or higher had a day 100 all-cause mortality rate of 28%.
Day-100 Survival Rate (N=271)
| Patients . | Troponin level ≥0.06 μg/L, no. of patients (n=40) . | Troponin level <0.06 μg/L, no. of patients (n=231) . | Total no. of patients . |
|---|---|---|---|
| *P<.001 | |||
| Died before day 100* | 11 | 16 | 27 |
| Survived beyond d+100 | 29 | 215 | 244 |
| Patients . | Troponin level ≥0.06 μg/L, no. of patients (n=40) . | Troponin level <0.06 μg/L, no. of patients (n=231) . | Total no. of patients . |
|---|---|---|---|
| *P<.001 | |||
| Died before day 100* | 11 | 16 | 27 |
| Survived beyond d+100 | 29 | 215 | 244 |
Patients with troponin levels less than 0.06 mg/L had a day-100 all-cause mortality rate of 7% (P<.001).
Despite possibly having multiple causes of death, for 7 of 11 patients with elevated troponin levels, cardiac causality could be inferred. For patients with low levels of troponin, clear cardiac causality was observed in 4 of 16. Among the 40 patients with troponin levels of 0.06 mg/L or higher, the conditioning dosage of melphalan was reduced for 31 patients (78%). Among the patients with troponin levels less than 0.06 mg/L, the dosage of melphalan was reduced for 29% of patients.
Conclusion: Troponin levels should be measured in all patients before transplantation. Those with troponin levels exceeding 0.06 mg/L should be considered for less toxic therapies until the clinically optimal use of stem cell transplantation is better defined by randomized clinical trials. The chemotherapy dosage was reduced for 77% of patients in the high troponin group, but acceptable treatment-related mortality rates were not achieved. Clearly, a risk-adapted approach that modified the dosage of conditioning chemotherapy did not compensate for poor patient health or advanced cardiac involvement.
Author notes
Disclosure: No relevant conflicts of interest to declare.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal