Abstract
Background: Early absolute lymphocyte count (ALC) recovery after autologous peripheral hematopoietic stem cell transplantation (ASCT) has been reported as an independent prognostic factor for overall survival and progression-free survival for patients with hematological and non-hematological cancers. Early immune reconstitution appears to have a protective effect against residual disease after ASCT.
End points: Assessment of factors impacting on early ALC recovery after ASCT.
Methods: Retrospective analysis of the ASCT procedures done between 2000 and 2007 in Hemorio. Early lymphocyte recovery (ELR) was defined as an ALC ≥500/μL at day 12 after ASCT.
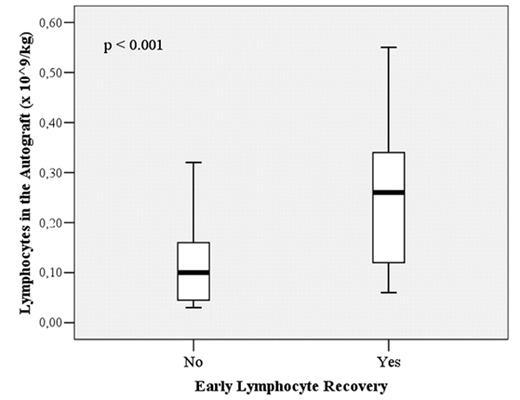
Results: A total of 53 of 66 consecutive ASCT (80,3%) were eligible for this study. Of the 53 ASCT, 9 were for lymphoma, 22 for multiple myeloma and 22 for acute myelogenous leukemia. Median age of the group was 34 years (range: 13–65). All patients except one were mobilized with chemotherapy plus granulocyte colony-stimulating factor (G-CSF). ELR was observed in 41% of the patients. Univariate analysis identified an association between the following factors and ELR: median pre-mobilization ALC (1920 vs 1060 lymphocytes/μL; p=0.003), pre-collection ALC (1637 vs 747 lymphocytes/μL; p<0.001), dose of leukocytes infused (1.21 x 109 vs 0.65 x 109 leukocytes/kg; p=0.002), dose of lymphocytes infused (0.26 x 109 vs 0.10 x 109 lymphocytes/kg; p<0.001), dose of CD4+ lymphocytes infused (0.075 x 109 vs 0.034 x 109 CD4+ lymphocytes/kg; p<0.001) and dose of CD8+ lymphocytes infused (0.11 x 109 vs 0.03 x 109 CD8+ lymphocytes/kg; p<0.001) were all higher in the ELR group. Patient diagnosis, number of previous cycles of chemotherapy and number of CD34+ cells collected were not correlated with ELR. Forward stepwise regression identified the pre-mobilization ALC and the number of lymphocytes in the autograft as factors related to ELR (p=0.013 and p<0.001; respectively). Multivariate analysis demonstrated that the lymphocyte dose in the graft can be predicted by the pre-collection ALC and the number of aphereses carried out (p<0.001 for both). Median pre-mobilization ALC was higher than pre-collection ALC (1335 vs 975 lymphocytes/μL respectively; p=0.013). This difference was most significant in the group of patients without ELR (1060 vs 747 lymphocytes/μL respectively; p=0.004). Among patients with ELR, the difference was not significant (1920 vs 1637 lymphocytes/μL respectively; p=0.53).
Conclusions: These results indicate that ELR after ASCT depends on the pre-mobilization ALC and the lymphocyte dose in the autograft. The number of aphereses performed for stem cell collection and the pre-collection ALC predict the number of lymphocytes collected. Stem cell mobilization with chemotherapy and G-CSF significantly reduces the ALC at the time of collection, specially in patients with lower ALC at the time of the mobilization. Strategies to improve immunologic recovery may have an impact on the results of ASCT.
Author notes
Disclosure: No relevant conflicts of interest to declare.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal