Abstract
Development of kinase domain mutations is a major drug-resistance mechanism for tyrosine kinase inhibitors (TKIs) in cancer therapy. A particularly challenging example is found in Philadelphia chromosome–positive chronic myelogenous leukemia (CML) where all available kinase inhibitors in clinic are ineffective against the BCR-ABL mutant, T315I. As an alternative approach to kinase inhibition, an orally administered heat shock protein 90 (Hsp90) inhibitor, IPI-504, was evaluated in a murine model of CML. Treatment with IPI-504 resulted in BCR-ABL protein degradation, decreased numbers of leukemia stem cells, and prolonged survival of leukemic mice bearing the T315I mutation. Hsp90 inhibition more potently suppressed T315I-expressing leukemia clones relative to the wild-type (WT) clones in mice. Combination treatment with IPI-504 and imatinib was more effective than either treatment alone in prolonging survival of mice simultaneously bearing both WT and T315I leukemic cells. These results provide a rationale for use of an Hsp90 inhibitor as a first-line treatment in CML by inhibiting leukemia stem cells and preventing the emergence of imatinib-resistant clones in patients. Rather than inhibiting kinase activity, elimination of mutant kinases provides a new therapeutic strategy for treating BCR-ABL–induced leukemia as well as other cancers resistant to treatment with tyrosine kinase inhibitors.
Introduction
The human Philadelphia chromosome (Ph) arises from a translocation between chromosomes 9 and 22 [t(9;22)(q34;q11)].1 The resulting chimeric BCR-ABL oncogene encodes a constitutively activated, oncogenic tyrosine kinase that induces chronic myeloid leukemia (CML) and B-cell acute lymphoblastic leukemia (B-ALL). The BCR-ABL TKI, imatinib mesylate, induces a complete hematologic and cytogenetic response in the majority of chronic-phase CML patients,2 but is unable to completely eradicate BCR-ABL–expressing leukemic cells,3,4 suggesting that leukemia stem cells are not eliminated. Over time, patients frequently become drug resistant and develop progressive disease despite continued treatment.5-11 Resistance is predominantly due to emergence of kinase domain mutations. Three newly developed BCR-ABL kinase inhibitors—dasatinib,12 AP23464,13 and AMN10714 —inhibit most of imatinib-resistant BCR-ABL mutants at biochemical and cellular levels, but are ineffective against the BCR-ABL-T315I mutant.15,16 New approaches are needed to treat drug-resistant forms of CML as well as BCR-ABL–induced B-ALL, a leukemia that does not respond well to available TKIs.15,16
Heat shock protein 90 (Hsp90) is a highly conserved, constitutively expressed molecular chaperone that facilitates folding of client proteins such as BCR-ABL, and affects the stability of these proteins.17-21 When BCR-ABL contains resistance-conferring mutations, it becomes even more dependent on Hsp90 in vitro.20 We therefore evaluated the therapeutic effect of Hsp90 inhibition by using a novel water-soluble inhibitor, IPI-504,22 in drug-resistant animal models of leukemia induced by BCR-ABL-WT and T315I.
Materials and methods
Cell lines
The 32D myeloid cell line was grown in RPMI 1640 medium containing 10% FCS and 10% WEHI medium. The BaF/3 pre-B-cell line was grown in RPMI 1640 medium containing 10% FCS, 10% WEHI medium, and 50 μM 2-mercaptoethanol. To generate the BCR-ABL–expressing 32D or BaF/3 line, the cells were transduced with the BCR-ABL-WT- or BCR-ABL-T315I-IRES-GFP-MSCV retrovirus, and the BCR-ABL–expressing cells were selected by GFP sorting by fluorescence-activated cell sorter (FACS).
Histology
The lungs from the placebo- or drug-treated mice were fixed in Bouin fixative (Fisher Scientific, Pittsburgh, PA) for 24 hours at room temperature, followed by an overnight rinse in water. Ten-μm sections were stained with hematoxylin and eosin (H&E) and observed by a model DMRE compound microscope (Leica, Heidelberg, Germany). All sections were imaged with a 2.5 × PH1 objective (NPLan, NA 0.25) and 10 × PH1 objective (NPLan, NA 0.40). All images were imported into MetaMorph software (Molecular Devices, Downingtown, PA) as a series of tagged image files. All images were then constructed in Adobe Photoshop 6.0 (Adobe, San Jose, CA).
Antibodies and Western blot analysis
Antibodies against c-ABL, Hsp90, Hsp70, and actin were purchased from Santa Cruz Biotechnology (Santa Cruz, CA). Protein lysates were prepared by lysing cells in radioimmunoprecipitation (RIPA) buffer, and immunoprecipitation and Western blotting were carried out as described previously.23
Bone marrow transduction/transplantation
The retroviral vector MSCV-IRES-eGFP24 carrying the p210 BCR-ABL cDNA was used to make high-titer, helper-free, replication-defective ecotropic virus stock by transient transfection of 293T cells using the kat system,25 as previously described.26 Six- to 10-week-old wild-type BABL/c or C57BL/6 mice (The Jackson Laboratory) were used for leukemogenesis experiments. Induction of CML26 and B-ALL26,27 was as described previously. Briefly, to model CML, bone marrow from 5-FU–treated (200 mg/kg) donor mice was transduced twice with BCR-ABL retrovirus by cosedentation in the presence of IL-3, IL-6, and SCF. To model B-ALL, bone marrow from non–5-FU–treated donors was transduced without cytokines. Wild-type recipient mice were prepared by 900 cGy (for BABL/c) or 1150 cGy (for C57BL/6) gamma irradiation and a dose of 0.5 × 106 (CML) or 1.0 × 106 (B-ALL) cells transplanted via tail vein injection. Diseased mice were analyzed by histopathological and biochemical analyses as described previously.26
Flow cytometry
Hematopoietic cells were collected from peripheral blood and bone marrow of the diseased mice, and red blood cells were lysed with NH4Cl red blood cell lysis buffer (pH 7.4). The cells were washed with PBS, and stained with B220-PE for B cells, Gr1-APC for neutrophils, and Sca1-APC/c-kit-PE for hematopoietic stem cells. After staining, the cells were washed once with PBS and subjected to FACS analysis.
Culture of leukemia stem cells
Drug treatment
IPI-504 was dissolved in a solution containing 50 mM citrate, 50 mM ascorbate, 2.44 mM EDTA, pH 3.3. Imatinib was dissolved in water. The drugs were given orally in a volume of less than 0.5 mL by gavage (50 or 100 mg/kg, every other day for IPI-504, and 100 mg/kg, twice a day for imatinib) beginning at 8 days after bone marrow transplantation, and continuing until the morbidity or death of the leukemic mice. Placebo is a solution containing 50 mM citrate, 50 mM ascorbate, 2.44 mM EDTA, pH 3.3.
Results
Inhibition of Hsp90 by IPI-504 causes BCR-ABL protein degradation
IPI-504 is the hydroquinone hydrochloride derivative of the well-described Hsp90 inhibitor, 17-AAG; the chemical structure of IPI-504 is shown in Figure 1A. To examine the effects of IPI-504 on stability of BCR-ABL protein and to test whether the degradation of BCR-ABL protein is initiated through IPI-504–induced disassociation of BCR-ABL from Hsp90, T315I-32D myeloid cells were treated with IPI-504 for 30 minutes and 4 hours, respectively. Hsp90 protein was immunoprecipitated and Hsp90-associated BCR-ABL protein was assessed. IPI-504 induced complete disassociation of BCR-ABL and Hsp90 within 30 minutes, followed by loss of BCR-ABL protein at 4 hours (Figure 1B). These results demonstrate that BCR-ABL protein is degraded after inhibition of Hsp90 by IPI-504 and this degradation occurs after disassociation of BCR-ABL from Hsp90. To further demonstrate that IPI-504 mediates the degradation of BCR-ABL through the proteasome, T315I-32D myeloid cells were treated with IPI-504 alone for up to 8 hours or with both IPI-504 and a proteasome inhibitor PS-34130,31 that should inhibit BCR-ABL degradation caused by IPI-504. PS-341 restored IPI-504–mediated depletion of BCR-ABL protein (Figure 1C).
Inhibition of Hsp90 by IPI-504 causes BCR-ABL protein degradation. (A) Structure of IPI-504. (B) IPI-504–induced disassociation of BCR-ABL and Hsp90, and subsequent degradation of BCR-ABL protein. BCR-ABL-T315I–expressing 32D cells were treated with IPI-504 (2 μM) for 30 minutes and 4 hours, respectively. Protein lysates were analyzed by Western blotting using antibodies indicated. WCL indicates whole cell lysate; IP, immunoprecipitation; and IB, immunoblotting. (C) The proteasome inhibitor PS-341 restored IPI-504–mediated depletion of BCR-ABL protein. BCR-ABL-T315I–expressing 32D cells were treated with IPI-504 (2 μM) alone or IPI-504 plus PS-341 (100 nM) for 4 or 8 hours, respectively. Protein lysates were analyzed by Western blotting using antibodies indicated. The well-described Hsp90 client, Akt, was evaluated as a positive control. Note that the cells were pretreated with PS-341 for 30 minutes prior to the cotreatment with IPI-504 and PS-341. The black lines indicate that the lanes that were not adjacent on the same original Western blotting gel were brought together to generate this figure.
Inhibition of Hsp90 by IPI-504 causes BCR-ABL protein degradation. (A) Structure of IPI-504. (B) IPI-504–induced disassociation of BCR-ABL and Hsp90, and subsequent degradation of BCR-ABL protein. BCR-ABL-T315I–expressing 32D cells were treated with IPI-504 (2 μM) for 30 minutes and 4 hours, respectively. Protein lysates were analyzed by Western blotting using antibodies indicated. WCL indicates whole cell lysate; IP, immunoprecipitation; and IB, immunoblotting. (C) The proteasome inhibitor PS-341 restored IPI-504–mediated depletion of BCR-ABL protein. BCR-ABL-T315I–expressing 32D cells were treated with IPI-504 (2 μM) alone or IPI-504 plus PS-341 (100 nM) for 4 or 8 hours, respectively. Protein lysates were analyzed by Western blotting using antibodies indicated. The well-described Hsp90 client, Akt, was evaluated as a positive control. Note that the cells were pretreated with PS-341 for 30 minutes prior to the cotreatment with IPI-504 and PS-341. The black lines indicate that the lanes that were not adjacent on the same original Western blotting gel were brought together to generate this figure.
Hsp90 is a therapeutic target for BCR-ABL–induced CML
An investigation of whether Hsp90 is an effective target for the treatment of CML in vivo was conducted in the bone marrow transplantation (BMT) mouse model of CML, in which bone marrow cells from BALB/c donor mice pretreated with 5-fluorouracil (5-FU) and transduced with BCR-ABL results in development of CML in BALB/c recipient mice.26 Mice with WT or T315I-transduced bone marrow from 5-FU–treated WT BALB/c donor mice were treated with a placebo, the Hsp90 inhibitor IPI-504, or imatinib alone, or the 2 agents in combination. All placebo-treated mice developed and died of CML within 3 weeks after BMT (Figure 2A). As expected, imatinib treatment was effective in treating WT-induced CML but not CML induced by T315I (Figure 2A). In a dose-dependent manner, treatment with IPI-504 alone significantly prolonged survival of mice with WT CML, but even more markedly prolonged survival of mice with T315I-induced CML (Figure 2A, P < .001). Inhibition of Hsp90 by IPI-504 appears to be more effective in treating CML induced by T315I than by WT BCR-ABL, consistent with results in Figure 1A and in line with previously reported results with the Hsp90 inhibitor, 17-AAG.20 In both cases, inhibition of Hsp90 results in degradation of mutant BCR-ABL more readily than WT. Treatment of mice with WT CML with both IPI-504 and imatinib was slightly more effective (but statistically insignificant) than with imatinib alone in prolonging survival of the mice (Figure 2A), while treatment of mice with BCR-ABL-T315I–induced CML with these 2 drugs did not further prolong survival of the mice compared with the mice treated with IPI-504 alone (Figure 2A). Prolonged survival of IPI-504–treated CML mice correlated with decreased peripheral blood BCR-ABL–expressing (GFP-positive) leukemia cells during therapy (Figure 2B, P < .001) and less splenomegaly at necropsy (Figure 2C). As lung hemorrhage caused by infiltration of mature myeloid leukemia cells is a major cause of death of CML mice,26 we further evaluated the therapeutic effect of IPI-504 on CML by examining the severity of lung hemorrhages at day 15 after BMT. Compared with placebo-treated mice, fewer hemorrhages were observed in the lungs of IPI-504–treated mice with BCR-ABL-T315I–induced CML (Figure 2D). Western blot analysis of spleen-cell lysates from the treated CML mice showed that IPI-504 reduced the levels of BCR-ABL protein in CML mice (Figure 2E).
Hsp90 is a therapeutic target for CML induced by either BCR-ABL-WT or BCR-ABL-T315I. (A) Treatment with the Hsp90 inhibitor IPI-504 prolonged survival of CML mice. Mice with BCR-ABL-WT (left panel)– or BCR-ABL-T315I (right panel)–induced CML were treated with placebo (n = 15 for BCR-ABL-WT; n = 13 for BCR-ABL-T315I), imatinib (100 mg/kg, twice a day by gavage) (n = 8 for both BCR-ABL-WT and -T315I), IPI-504 (50 mg/kg, once every 2 days by gavage) (n = 20 for both BCR-ABL-WT and BCR-ABL-T315I), IPI-504 (100 mg/kg, once every 2 days by gavage) (n = 8 for both BCR-ABL-WT; n = 7 for BCR-ABL-T315I), and imatinib + IPI-504 (n = 12 for both BCR-ABL-WT and -T315I), respectively, beginning at day 8 after transplantation. The IPI-504–treated mice with BCR-ABL-T315I–induced CML lived longer than those with BCR-ABL-WT–induced CML (comparing between left and right panels). (B) Flow cytometric evaluation of the leukemic process in IPI-504– or imatinib-treated CML mice. The number of circulating leukemic cells (calculated as percentage of Gr-1+ GFP+ cells × white blood cell count) in mice with BCR-ABL-WT (left panel)– or BCR-ABL-T315I (right panel)–induced CML treated with placebo, imatinib, IPI-504, or the combination of imatinib and IPI-504 was determined on day 14 after transplantation. (C) Spleen weights of CML mice treated with placebo, imatinib, IPI-504, and combination of imatinib and IPI-504. (Left panel) BCR-ABL-WT. (Right panel) BCR-ABL-T315I. (D) Photomicrographs of hematoxylin and eosin–stained lung sections from drug-treated mice at day 14 after transplantation. (E) Western blot analysis of spleen-cell lysates for degradation of BCR-ABL in IPI-504–treated CML mice. IB indicates immunoblot.
Hsp90 is a therapeutic target for CML induced by either BCR-ABL-WT or BCR-ABL-T315I. (A) Treatment with the Hsp90 inhibitor IPI-504 prolonged survival of CML mice. Mice with BCR-ABL-WT (left panel)– or BCR-ABL-T315I (right panel)–induced CML were treated with placebo (n = 15 for BCR-ABL-WT; n = 13 for BCR-ABL-T315I), imatinib (100 mg/kg, twice a day by gavage) (n = 8 for both BCR-ABL-WT and -T315I), IPI-504 (50 mg/kg, once every 2 days by gavage) (n = 20 for both BCR-ABL-WT and BCR-ABL-T315I), IPI-504 (100 mg/kg, once every 2 days by gavage) (n = 8 for both BCR-ABL-WT; n = 7 for BCR-ABL-T315I), and imatinib + IPI-504 (n = 12 for both BCR-ABL-WT and -T315I), respectively, beginning at day 8 after transplantation. The IPI-504–treated mice with BCR-ABL-T315I–induced CML lived longer than those with BCR-ABL-WT–induced CML (comparing between left and right panels). (B) Flow cytometric evaluation of the leukemic process in IPI-504– or imatinib-treated CML mice. The number of circulating leukemic cells (calculated as percentage of Gr-1+ GFP+ cells × white blood cell count) in mice with BCR-ABL-WT (left panel)– or BCR-ABL-T315I (right panel)–induced CML treated with placebo, imatinib, IPI-504, or the combination of imatinib and IPI-504 was determined on day 14 after transplantation. (C) Spleen weights of CML mice treated with placebo, imatinib, IPI-504, and combination of imatinib and IPI-504. (Left panel) BCR-ABL-WT. (Right panel) BCR-ABL-T315I. (D) Photomicrographs of hematoxylin and eosin–stained lung sections from drug-treated mice at day 14 after transplantation. (E) Western blot analysis of spleen-cell lysates for degradation of BCR-ABL in IPI-504–treated CML mice. IB indicates immunoblot.
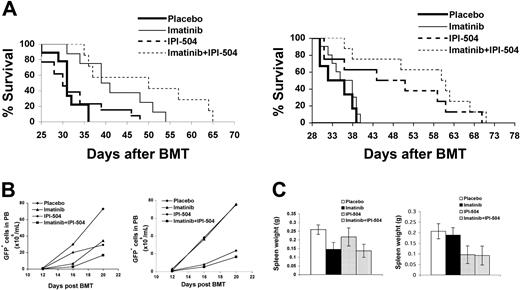
Hsp90 is also a therapeutic target for B-ALL induced by BCR-ABL-T315I
CML often initiates in a chronic phase and eventually progresses to a terminal blastic phase, in which either acute myeloid or acute B-lymphoid leukemia develops.32 Some Ph+ leukemia patients have B-ALL as their first clinical appearance. B-ALL is similar pathologically to acute B-lymphoid leukemia in the blastic phase of CML. Notably, both forms of acute leukemia do not respond well to available BCR-ABL kinase inhibitors.15,16 To model B-ALL in mice, BCR-ABL–transduced bone marrow cells from donor mice that are not pretreated with 5-FU are transplanted into BALB/c mice.26,33 In this model, the malignant pre-B cells express the cell surface markers B220 and CD19, and phenotypically resemble de novo Ph+ B-ALL and lymphoid blast crisis of CML.26,27 To determine whether inhibition of Hsp90 is effective in treating WT or T315I-induced B-ALL, these mice were treated with a placebo, IPI-504 alone, imatinib alone, or the 2 agents in combination (Figure 3). All placebo-treated recipients of WT or T315I-transduced bone marrow developed and died of B-ALL within 5 to 6 weeks after BMT (Figure 3A). IPI-504 treatment did not prolong survival of mice with BCR-ABL-WT–induced B-ALL (Figure 3A), in contrast to its therapeutic effect on CML induced by BCR-ABL-WT (Figure 2A). Given the dose response seen in the CML study and significant improvement in survival when the dose of IPI-504 is increased from 50 to 100 mg, a similar increase in dose may be needed in B-ALL. However, similar to the effect seen in CML (Figure 2A), IPI-504 treatment significantly prolonged survival of mice with T315I- B-ALL (Figure 3A, P < .001). Prolonged survival of IPI-504–treated B-ALL mice correlated with decreased numbers of peripheral blood BCR-ABL–expressing leukemia cells and spleen weights during therapy (Figure 3B-C, P < .001). Once again, inhibition of Hsp90 by IPI-504 is more effective against tumor cells bearing T315 than BCR-ABL-WT.
Hsp90 is a therapeutic target for B-ALL induced by BCR-ABL-T315I. (A) Treatment with the Hsp90 inhibitor IPI-504 prolonged survival of mice with B-ALL induced by BCR-ABL-T315I (right panel) but not by BCR-ABL-WT (left panel). B-ALL mice treated with a placebo (n = 9 for BCR-ABL-WT; n = 8 for BCR-ABL-T315I), imatinib (n = 8 for BCR-ABL-WT; n = 10 for BCR-ABL-T315I), IPI-504 (n = 13 for BCR-ABL-WT; n = 8 for BCR-ABL-T315I), and combination of imatinib and IPI-504 (n = 10 for BCR-ABL-WT; n = 8 for BCR-ABL-T315I). (B) Flow cytometric evaluation of the leukemic process in IPI-504– or imatinib-treated mice with B-ALL induced by BCR-ABL-WT (left panel) or BCR-ABL-T315I (right panel). The number of circulating leukemic cells (calculated as percentage of B220+ GFP+ cells × white blood cell count) in B-ALL mice treated with placebo, imatinib, IPI-504, or the combination of imatinib and IPI-504 was determined on days 11, 14, and 17 after transplantation. (C) Spleen weights of B-ALL mice treated with placebo, imatinib, IPI-504, and combination of imatinib and IPI-504. (Left panel) BCR-ABL-WT. (Right panel) BCR-ABL-T315I.
Hsp90 is a therapeutic target for B-ALL induced by BCR-ABL-T315I. (A) Treatment with the Hsp90 inhibitor IPI-504 prolonged survival of mice with B-ALL induced by BCR-ABL-T315I (right panel) but not by BCR-ABL-WT (left panel). B-ALL mice treated with a placebo (n = 9 for BCR-ABL-WT; n = 8 for BCR-ABL-T315I), imatinib (n = 8 for BCR-ABL-WT; n = 10 for BCR-ABL-T315I), IPI-504 (n = 13 for BCR-ABL-WT; n = 8 for BCR-ABL-T315I), and combination of imatinib and IPI-504 (n = 10 for BCR-ABL-WT; n = 8 for BCR-ABL-T315I). (B) Flow cytometric evaluation of the leukemic process in IPI-504– or imatinib-treated mice with B-ALL induced by BCR-ABL-WT (left panel) or BCR-ABL-T315I (right panel). The number of circulating leukemic cells (calculated as percentage of B220+ GFP+ cells × white blood cell count) in B-ALL mice treated with placebo, imatinib, IPI-504, or the combination of imatinib and IPI-504 was determined on days 11, 14, and 17 after transplantation. (C) Spleen weights of B-ALL mice treated with placebo, imatinib, IPI-504, and combination of imatinib and IPI-504. (Left panel) BCR-ABL-WT. (Right panel) BCR-ABL-T315I.
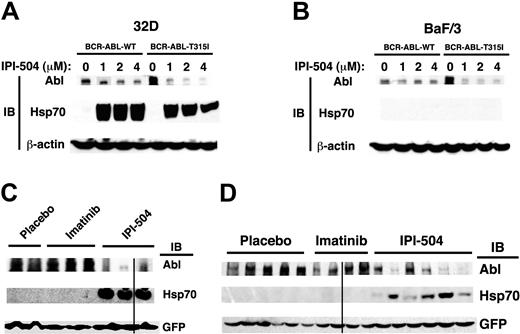
Hsp90 inhibition has differential effects on BCR-ABL degradation and Hsp70 induction in myeloid and lymphoid cells in vitro
To investigate why inhibition of Hsp90 is more effective in treating CML than B-ALL (Figures 2–3), we compared the effects of treatment with IPI-504 on BCR-ABL-WT or BCR-ABL-T315I at protein level in a mouse myeloid cell line (32D) and a mouse lymphoid cell line (BaF/3) (Figure 4). BCR-ABL–expressing 32D and BaF/3 cells were treated with different concentrations of IPI-504. After treatment, levels of BCR-ABL-WT protein were dramatically decreased in 32D cells (Figure 4A), but only slightly in BaF/3 cells (Figure 4B). Compared with BCR-ABL-WT, BCR-ABL-T315I was more sensitive to IPI-504–induced degradation in both 32D and BaF/3 cells, but levels of BCR-ABL protein were decreased much more markedly in 32D cells than in BaF/3 cells (Figure 4A-B). These results indicate that inhibition of Hsp90 by IPI-504 affects BCR-ABL stability more strongly in myeloid cells than in lymphoid cells. It has been shown that the Hsp90 antagonists geldanamycin and 17-AAG alter chaperone association of Hsp90 with BCR-ABL and facilitate binding of BCR-ABL to heat shock protein 70 (hsp70), resulting in degradation of BCR-ABL by the proteasome.19,34-36 Recent studies have shown that Hsp70 plays a positive role in BCR-ABL–mediated resistance to apoptosis.37,38 If Hsp70 plays a role in decreased sensitivity of B-ALL than CML to IPI-504 treatment, we expect that after IPI-504 treatment, Hsp70 would be induced to a much higher level in BCR-ABL–expressing lymphoid cells than in myeloid cells. However, an increase in intracellular Hsp70 levels was observed in IPI-504–treated BCR-ABL–expressing 32D but not Ba/F3 cells (Figure 4A-B). This observation is consistent with our in vivo observation in cells from CML and B-ALL mice, which showed that the level of Hsp70 in leukemic cells from IPI-504–treated CML mice is higher than that in leukemic cells from B-ALL mice (Figure 4C-D). Thus, Hsp70 is not an explanation for the decreased sensitivity of B-ALL compared with CML upon IPI-504 treatment (Figures 2–3).
Hsp90 inhibition has differential effects on BCR-ABL degradation and Hsp70 induction in myeloid and lymphoid cells in vitro and in vivo. (A) In 32D cells, IPI-504–induced degradation of BCR-ABL-T315I was greater than that of BCR-ABL-WT. BCR-ABL-WT– or BCR-ABL-T315I–expressing 32D cells were treated with different concentrations of IPI-504 for 12 hours. Protein lysates were analyzed by Western blotting using antibodies indicated. (B) In Ba/F3 cells, IPI-504 induced significant degradation of BCR-ABL-T315I but not BCR-ABL-WT. BCR-ABL-WT– or BCR-ABL-T315I–expressing 32D cells were treated with different concentrations of IPI-504 for 12 hours. Protein lysates were analyzed by Western blotting using antibodies indicated. (C) Mice with BCR-ABL-T315I–induced CML were treated with placebo, imatinib (100 mg/kg, twice a day by gavage), and IPI-504 (50 mg/kg, once every 2 days by gavage), respectively, for 8 days, beginning at day 8 after transplantation. At 6 hours after the last dose, protein lysates of leukemic cells from the spleen of the treated CML mice were analyzed by Western blotting using antibodies indicated. The black line indicates that the lanes that were not adjacent on the same original Western blotting gel were brought together to generate this figure. (D) Mice with BCR-ABL-T315I–induced B-ALL were treated with placebo, imatinib, and IPI-504, respectively, for 8 days, beginning at day 8 after transplantation. At 6 hours after the last dose, protein lysates of leukemic cells from the spleen of the treated mice were analyzed by Western blotting using antibodies indicated. The black line indicates that the lanes that were not adjacent on the same original Western blotting gel were brought together to generate this figure.
Hsp90 inhibition has differential effects on BCR-ABL degradation and Hsp70 induction in myeloid and lymphoid cells in vitro and in vivo. (A) In 32D cells, IPI-504–induced degradation of BCR-ABL-T315I was greater than that of BCR-ABL-WT. BCR-ABL-WT– or BCR-ABL-T315I–expressing 32D cells were treated with different concentrations of IPI-504 for 12 hours. Protein lysates were analyzed by Western blotting using antibodies indicated. (B) In Ba/F3 cells, IPI-504 induced significant degradation of BCR-ABL-T315I but not BCR-ABL-WT. BCR-ABL-WT– or BCR-ABL-T315I–expressing 32D cells were treated with different concentrations of IPI-504 for 12 hours. Protein lysates were analyzed by Western blotting using antibodies indicated. (C) Mice with BCR-ABL-T315I–induced CML were treated with placebo, imatinib (100 mg/kg, twice a day by gavage), and IPI-504 (50 mg/kg, once every 2 days by gavage), respectively, for 8 days, beginning at day 8 after transplantation. At 6 hours after the last dose, protein lysates of leukemic cells from the spleen of the treated CML mice were analyzed by Western blotting using antibodies indicated. The black line indicates that the lanes that were not adjacent on the same original Western blotting gel were brought together to generate this figure. (D) Mice with BCR-ABL-T315I–induced B-ALL were treated with placebo, imatinib, and IPI-504, respectively, for 8 days, beginning at day 8 after transplantation. At 6 hours after the last dose, protein lysates of leukemic cells from the spleen of the treated mice were analyzed by Western blotting using antibodies indicated. The black line indicates that the lanes that were not adjacent on the same original Western blotting gel were brought together to generate this figure.
Inhibition of Hsp90 suppresses CML stem cells
In the BMT CML model, imatinib prolongs survival of mice with BCR-ABL–induced CML,33,39 but does not stop progression of the disease,33 partially due to the inability of imatinib to completely eradicate leukemia stem cells.40 Hematopoietic stem cells (HSCs) have been identified in the CML model by showing that the Lin−c-Kit+Sca-1+ population is sufficient to confer leukemia in recipient mice.40 To investigate whether inhibition of Hsp90 has an inhibitory effect on leukemia stem cells in CML, we first isolated bone marrow cells from mice with T315I-induced CML and cultured the cells in conditions that support survival and growth of HSCs.28,29 During culture, the cells were treated with IPI-504 or imatinib (Figure 5). Six days after the treatment, we analyzed survival of GFP+Lin−c-Kit+Sca-1+ cells, representing leukemia stem cells remaining in the culture. FACS analysis showed that compared with the untreated group, imatinib treatment did not lower the percentage and the number of leukemia stem cells, whereas IPI-504 treatment had a dramatic inhibitory effect on the stem cells (Figure 5A, P < .001). We next tested whether IPI-504 inhibits leukemia stem cells in CML mice. Mice with BCR-ABL-T315I–induced CML were treated with a placebo, imatinib, or IPI-504 for 6 days, and bone marrow cells were analyzed by FACS for GFP+Lin−c-Kit+Sca-1+ cells. Consistent with the in vitro results, imatinib treatment did not lower the percentage and number of leukemia stem cells, compared with the untreated group, whereas IPI-504 treatment had a dramatic inhibitory effect on the stem cells (Figure 5B). To determine whether IPI-504 had an effect on normal HSCs in mice, WT mice were treated with IPI-504 or placebo for 2 weeks. Analysis of bone marrow from these mice showed that there was no change in levels of Lin−c-Kit+Sca-1+ cells from any treatment group (Figure 5C), indicating that IPI-504 treatment did not inhibit survival of normal HSCs.
Targeting Hsp90 by IPI-504 inhibits survival of leukemia stem cells. (A) Bone marrow cells isolated from C57BL/6 (B6) mice with BCR-ABL-T315I–induced CML were cultured in vitro (5 × 106 cells/6 cm tissue culture plate) under the stem cell condition (“Materials and methods”) in the presence or absence of IPI-504 (0.1 μM) or imatinib (2 μM) for 6 days (changing the stem cell medium containing placebo or IPI-504 at day 3) followed by FACS analysis of leukemia stem cells (GFP+Lin−c-Kit+Sca-1+). (B) Mice with BCR-ABL-T315I–induced CML were treated with a placebo (n = 5), imatinib (100 mg/kg, twice a day by gavage) (n = 5), and IPI-504 (50 mg/kg, once every 2 days by gavage) (n = 5), respectively, for 6 days beginning at day 8 after transplantation. Bone marrow cells were isolated from the treated CML mice, and leukemia stem cells were analyzed by FACS. The numbers of cells represent total leukemia stem cells in average from femur and tibia of each treated CML mouse. (C) IPI-504 had no inhibitory effect on survival of normal HSCs in mice. B6 mice were treated with a placebo (n = 5), imatinib (100 mg/kg, twice a day by gavage) (n = 5), and IPI-504 (50 mg/kg, once every 2 days by gavage) (n = 5), respectively, for 2 weeks. Bone marrow cells were isolated from the treated mice, and were analyzed by FACS.
Targeting Hsp90 by IPI-504 inhibits survival of leukemia stem cells. (A) Bone marrow cells isolated from C57BL/6 (B6) mice with BCR-ABL-T315I–induced CML were cultured in vitro (5 × 106 cells/6 cm tissue culture plate) under the stem cell condition (“Materials and methods”) in the presence or absence of IPI-504 (0.1 μM) or imatinib (2 μM) for 6 days (changing the stem cell medium containing placebo or IPI-504 at day 3) followed by FACS analysis of leukemia stem cells (GFP+Lin−c-Kit+Sca-1+). (B) Mice with BCR-ABL-T315I–induced CML were treated with a placebo (n = 5), imatinib (100 mg/kg, twice a day by gavage) (n = 5), and IPI-504 (50 mg/kg, once every 2 days by gavage) (n = 5), respectively, for 6 days beginning at day 8 after transplantation. Bone marrow cells were isolated from the treated CML mice, and leukemia stem cells were analyzed by FACS. The numbers of cells represent total leukemia stem cells in average from femur and tibia of each treated CML mouse. (C) IPI-504 had no inhibitory effect on survival of normal HSCs in mice. B6 mice were treated with a placebo (n = 5), imatinib (100 mg/kg, twice a day by gavage) (n = 5), and IPI-504 (50 mg/kg, once every 2 days by gavage) (n = 5), respectively, for 2 weeks. Bone marrow cells were isolated from the treated mice, and were analyzed by FACS.
Inhibition of Hsp90 prevents emergence of the T315I-expressing clones over the WT clones
The effectiveness of IPI-504 in prolonging survival of mice with CML and B-ALL induced by the T315I mutant (Figures 2–3) suggests that inhibition of Hsp90 would preferentially prevent emergence of the T315I-expressing clones over the WT clones. To test this hypothesis, studies were performed in mice bearing both populations of leukemic cells. In the first study, bone marrow cells (BMCs) from Ly 5.1 and Ly5.2 C57BL/6 mice were transduced with BCR-ABL-T315I and BCR-ABL-WT, respectively. Equal numbers of donor BMCs were mixed and transplanted into recipient mice. Mice were treated with a placebo, imatinib, or IPI-504. During the treatment, FACS analysis was performed to assess the percentages of GFP+Gr-1+Ly5.1+ (representing T315I-expressing cells) and GFP+Gr-1+Ly5.1− (representing WT-expressing cells) cells in peripheral blood of the CML mice (Figure 6A). In placebo-treated mice, the ratio between T315I- and WT-expressing cells remained unchanged, and in imatinib-treated mice, T315I-expressing cells became dominant. In contrast, with continuous treatment of IPI-504, T315I-expressing cells gradually decreased to a low level (Figure 6A). Mice treated with IPI-504 lived significantly longer than those treated with imatinib (Figure 6A). Consistent with previous data, these results indicate that inhibition of Hsp90 preferentially suppresses T315I-expressing leukemic clones over the WT-expressing clones. In the second study, BMCs from BALB/c mice were transduced with BCR-ABL-T315I and BCR-ABL-WT, respectively, and equal numbers of the transduced cells were mixed and transplanted into recipient mice. Mice were treated with a placebo, imatinib, IPI-504, or both agents (Figure 6B). Mice treated with the combination of IPI-504 and imatinib survived significantly longer than those treated with IPI-504 or imatinib alone. Results from these studies suggest that the combined use of IPI-504 and imatinib would be a viable strategy for preventing emergence of imatinib-resistant clones in the clinic.
Inhibition of Hsp90 by IPI-504 preferentially reduces growth of myeloid leukemic cells harboring the BCR-ABL-T315I mutant. (A) Bone marrow cells from C57BL/6-Ly5.2 mice were transduced by BCR-ABL-WT, and bone marrow cells from C57BL/6-Ly5.1 mice were transduced by BCR-ABL-T315I. The transduced cells were 1:1 mixed, and 0.5 × 106 mixed cells were injected into each recipient mouse (C57BL/6-Ly5.2). The mice were treated with a placebo (n = 10), imatinib (100 mg/kg, twice a day) (n = 10), and IPI-504 (50 mg/kg, once every 2 days) (n = 10), respectively, beginning at 8 days after BMT. At days 12 and 15 after BMT, GFP+ cells viable cells in peripheral blood of the mice were analyzed for Gr-1+Ly5.1+ cells that represented BCR-ABL-T315I–expressing myeloid cells. Gr-1+Ly5.1− cells represented BCR-ABL-WT–expressing myeloid cells. Percentages of BCR-ABL-T315I–expressing myeloid cells in peripheral blood of IPI-504–treated CML mice were further analyzed at days 21 and 28 after BMT. The FACS results for one representative mouse from each treatment group were shown. IPI-504 but not imatinib significantly prolonged survival of the CML mice. (B) Simultaneous inhibition of Hsp90 and BCR-ABL kinase activity with IPI-504 and imatinib significantly prolongs survival of CML mice carrying both T315-expressing and WT-BCR-ABL leukemia cells. BALB/c mice were used to induce CML, and each treatment group had 10 mice.
Inhibition of Hsp90 by IPI-504 preferentially reduces growth of myeloid leukemic cells harboring the BCR-ABL-T315I mutant. (A) Bone marrow cells from C57BL/6-Ly5.2 mice were transduced by BCR-ABL-WT, and bone marrow cells from C57BL/6-Ly5.1 mice were transduced by BCR-ABL-T315I. The transduced cells were 1:1 mixed, and 0.5 × 106 mixed cells were injected into each recipient mouse (C57BL/6-Ly5.2). The mice were treated with a placebo (n = 10), imatinib (100 mg/kg, twice a day) (n = 10), and IPI-504 (50 mg/kg, once every 2 days) (n = 10), respectively, beginning at 8 days after BMT. At days 12 and 15 after BMT, GFP+ cells viable cells in peripheral blood of the mice were analyzed for Gr-1+Ly5.1+ cells that represented BCR-ABL-T315I–expressing myeloid cells. Gr-1+Ly5.1− cells represented BCR-ABL-WT–expressing myeloid cells. Percentages of BCR-ABL-T315I–expressing myeloid cells in peripheral blood of IPI-504–treated CML mice were further analyzed at days 21 and 28 after BMT. The FACS results for one representative mouse from each treatment group were shown. IPI-504 but not imatinib significantly prolonged survival of the CML mice. (B) Simultaneous inhibition of Hsp90 and BCR-ABL kinase activity with IPI-504 and imatinib significantly prolongs survival of CML mice carrying both T315-expressing and WT-BCR-ABL leukemia cells. BALB/c mice were used to induce CML, and each treatment group had 10 mice.
Other imatinib-resistant BCR-ABL mutants are also sensitive to Hsp90 inhibition
Other resistance-conferring BCR-ABL kinase domain mutations have been observed in imatinib refractory CML patients, including E225K, M351T, and Y253F.5,9 Consistent with the increased dependency of BCR-ABL-T315I on Hsp90, IPI-504 also prolonged survival of mice with CML induced by these mutants (Figure 7).
Other imatinib-resistant BCR-ABL mutants are also sensitive to Hsp90 inhibition. IPI-504 treatment prolonged survival of mice with CML induced by imatinib-resistant BCR-ABL-E225K (n = 10), -M351T (n = 10), or -Y253F (n = 10).
Other imatinib-resistant BCR-ABL mutants are also sensitive to Hsp90 inhibition. IPI-504 treatment prolonged survival of mice with CML induced by imatinib-resistant BCR-ABL-E225K (n = 10), -M351T (n = 10), or -Y253F (n = 10).
Discussion
While the mechanism of primary resistance to imatinib and dasatinib therapy in CML patients is poorly understood, the mechanisms of secondary resistance have been very well characterized. Kinase domain mutations represent the predominant form of secondary resistance accounting for up to 90% of cases. Currently, no drugs have been effective in treating patients with CML and B-ALL harboring the BCR-ABL-T315I mutation. Recent clinical trials with dasatinib revealed that patients known to have the BCR-ABL-T315I mutation prior to therapy had no objective response to treatment.16 Thus, as newer tyrosine kinase inhibitors (TKIs) that effectively block other resistant mutations become clinically available, the T315I mutation may become the predominant acquired resistance mutation. The challenge for development of an effective Ph+ leukemia therapy is therefore to develop an alternative treatment strategy that does not rely solely on kinase domain inhibition but rather results in degradation of the offending BCR-ABL protein regardless of its mutational status. Herein, we demonstrate that direct inhibition of Hsp90 function with IPI-504 represents an alternative treatment strategy that results in degradation of the offending BCR-ABL protein regardless of its mutational status. Our findings suggest that inhibition of other targets that impact Hsp90 function might also be effective in murine models of Ph+ leukemia. For example, histone deacetylatase (HDAC) inhibitors that induce acetylation and inhibition of Hsp90 might also be active.41-44
While imatinib induces complete hematologic and cytogenetic remission in the majority of newly diagnosed chronic-phase CML patients,45 molecular remission is difficult to achieve in these patients. One study designed to look at newly diagnosed chronic-phase patients using the standard-dose imatinib (400 mg daily), with a 18-month follow-up showed that only 39% of patients obtained a major molecular response (greater than or equal to 3-log reduction of BCR-ABL mRNA), whereas even fewer patients, 4%, obtained a complete molecular response rate (negativity by reverse-transcription–polymerase chain reaction [RT-PCR]).46 One prediction as to why the patients do not obtain a complete molecular response is perhaps due to imatinib not targeting the BCR-ABL–positive stem cells. This suggests that therapy with imatinib does not completely eradicate leukemic cells. It is likely that a small number of leukemic cells remain in imatinib-treated CML patients, and these cells may function as leukemia stem cells responsible for disease relapse. The inhibitory effects of IPI-504 on leukemia stem cells, while appearing to spare the normal hematopoietic stem cells, merits further investigation. Sole inhibition of BCR-ABL by imatinib has limited inhibitory effects on leukemic stem cells in mice.40 Thus, a pathway distinct from BCR-ABL is likely involved in suppression of survival of leukemic stem cells by IPI-504. A plausible explanation is that BCR-ABL cooperates with a non–BCR-ABL signaling pathway that is driven by an unknown Hsp90 client protein to maintain survival of leukemic stem cells. IPI-504 is able to inhibit both pathways, as would be necessary to suppress leukemic stem cells. The putative pathway that is Hsp90 dependent might be less critical for normal hematopoietic stem cells. The putative non–BCR-ABL pathway in leukemic stem cells requires further study.
The inhibitory effects of IPI-504 on BCR-ABL-T315I–expressing cells indicate that Hsp90 may serve as an effective target for treating imatinib- and dasatinib-resistant CML patients, as well as patients with blast crisis or with Ph+ ALL. The simultaneous use of IPI-504 and imatinib in chronic-phase CML patients might prevent the development of imatinib-resistant clones and inhibit growth of highly proliferative leukemic cells through inhibition of BCR-ABL kinase activity, thereby providing a rationale for combination strategy. Likewise, early use of IPI-504 to suppress initial B-ALL clones may help prevent the transition of CML to advanced B-ALL caused by the BCR-ABL-T315I mutation. While IPI-504 was active in BCR-ABL–induced B-ALL, the activity was not as pronounced as in CML. Studies to evaluate the mechanism for this difference showed that Hsp70 was more strongly induced in myeloid cells compared with lymphoid cells. Hsp70 is reported to exert antiapoptotic effects in a variety of settings and cell types, including leukemia cells that are exposed to Hsp90 inhibitors.37,38 In separate studies, inhibition of Hsp90 was shown to result in increased binding of BCR-ABL to Hsp70, thereby favoring proteasome-mediated degradation of BCR-ABL.19,34-36 Thus, on one hand, Hsp70 induction could counter the effects of Hsp90 inhibition, while other studies suggest that Hsp70 could have a positive influence on the ability of Hsp90 inhibition to result in degradation of BCR-ABL. Elucidation of the mechanism of differential sensitivity to Hsp90 inhibition between myeloid and lymphoid leukemia will require more extensive studies, as variation in Hsp70 induction is not likely the cause.
In summary, IPI-504 represents a novel therapeutic approach whereby inhibition of Hsp90 in CML patients and Ph+ ALL may significantly advance efforts to develop a cure for these diseases. The rationale underlying the use of IPI-504 for kinase inhibitor–resistant CML has implications for other cancers that display oncogene addiction to kinases that are Hsp90 client proteins. While resistant conferring kinase-domain mutations were originally described in CML, analogous mutations have been observed in lung cancer, gastrointestinal stromal tumor, and the hypereosinophilic syndrome with resistance to kinase inhibitor therapy.47 IPI-504 is currently in clinical trials to evaluate its potential for treating cancer that has become resistant to therapy with tyrosine kinase inhibitors such as imatinib.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 USC section 1734.
Acknowledgments
This work was supported by grants from the Department of Defense, and the National Cancer Institute (R01-CA114199) to S.L.
We thank Stephen B. Sampson for critical reading of the paper, Patricia Cherry for secretarial assistance, and Richard A. Van Etten for the BCR-ABL mutant constructs E225K, M351T, and Y253F.
National Institutes of Health
Authorship
Contribution: C.P. performed experiments and analyzed the data; J.B. provided reagents and helped with the paper; Y.H., L.K., and A.G. helped with the experiments; D.G. provided reagents and helped with the paper; M.R. provided reagents and helped with the paper; R.P. provided reagents; S.L. designed and performed experiments, analyzed the data, and wrote the paper.
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Correspondence: Shaoguang Li, The Jackson Laboratory, 600 Main St, Bar Harbor, ME 04609; e-mail: shaoguang.li@jax.org.






This feature is available to Subscribers Only
Sign In or Create an Account Close Modal