Abstract
One-hundred thirty-nine patients with acute lymphoblastic leukemia (ALL) and hypodiploidy (fewer than 45 chromosomes) were collected from 10 different national ALL study groups and single institutions. Patients were stratified by modal chromosome number into 4 groups: 24 to 29 (N = 46); 33 to 39 (N = 26); 40 to 43 (N = 13); and 44 (N = 54) chromosomes. Nine patients were Philadelphia chromosome (Ph) positive (4 cases: 44 chromosomes; 5 cases: 40-43 chromosomes) and were not considered further. Event-free survival (EFS) and overall survival (OS) of the remaining 130 patients were 38.5% ± 4.4% and 49.8% ± 4.2% at 8 years, respectively. There were no significant differences in outcome between patients with 24 to 29, 33 to 39, or 40 to 43 chromosomes. Compared with patients with fewer than 44 chromosomes, patients with 44 chromosomes had a significantly better EFS (P = .01; 8-year estimate, 52.2% vs 30.1%) and OS (P = .017; 69% vs 37.5%). For patients with 44 chromosomes, monosomy 7, the presence of a dicentric chromosome, or both predicted a worse EFS but similar OS. Doubling of the hypodiploid clone occurred in 32 patients (24-29 chromosomes [n = 25] and 33-39 chromosomes [n = 7]) and had no prognostic implication. Children and adolescents with ALL and hypodiploidy with fewer than 44 chromosomes have a poor outcome despite contemporary therapy.
Introduction
Ploidy is a highly significant prognostic factor in childhood acute lymphoblastic leukemia (ALL).1 A hyperdiploid karyotype with more than 50 chromosomes (particularly those with trisomies for 4, 10, 17, 18) identifies patients with a favorable outcome.2,3 By contrast, hypodiploidy (modal chromosome number fewer than 46) is associated with a poor outcome.4–9 The majority of hypodiploid patients show 45 chromosomes in their leukemic cells and have a significantly better outcome than patients with fewer than 45 chromosomes.5 It is not uncommon for leukemic cells with 23 to 29 and 33 to 39 chromosomes to undergo doubling of the hypodiploid clone such that the modal chromosome number may fall in the hyperdiploid or triploid range,10 respectively. Analysis of the specific pattern of chromosomal gains and losses or flow cytometric determination of DNA content can identify such doubled populations
Hypodiploidy with fewer than 45 chromosomes is very uncommon. In a large MRC study, excluding patients with an established chromosomal structural abnormality, 5% of patients had hypodiploidy of which only 1% had fewer than 45 chromosomes in their leukemic clone.5
To better understand the epidemiology, prognostic factors, and treatment outcome for children and adolescents with ALL and fewer than 45 chromosomes, 139 cases were collected from 10 participating cooperative groups and large single institutions in the United States and Europe for investigation.
This article represents a record review from studies that were previously approved by each institution's local IRB. Informed consent was obtained in accordance with the Declaration of Helsinki.
Patients, materials, and methods
Patients
Study groups or institutions reviewed their own records and identified ALL patients with fewer than 45 chromosomes who were registered on ALL clinical trials between 1986 and 1996. A predefined data set was collected for each patient and the data were sent to a central coordinating center for review. Of the 173 patients for whom data were submitted, 2 were ineligible because their date of diagnosis did not meet study entrance criteria, and 32 had karyotypes that were not evaluable. Thus, 139 cases were eligible. Cases were accrued from the following groups: AIEOP-3; BFM-5; CCG-33; COALL-3; DANA FARBER-4; POG-44; SJCRH-6; UK-20; NOPHO-6; and EORTC-15. Most of the patients received treatment on higher-risk regimens. Nine patients underwent bone marrow transplantation in first remission.
Statistical methods
Analyses were based on patient follow-up through December 2003. Clinical, demographic, and laboratory features of the various hypodiploid subgroups were compared using χ2 tests for homogeneity of proportions. Outcome was analyzed using life table methods and associated statistics. The primary end points examined were event-free survival (EFS) and overall survival (OS) from study entry; events included induction failure due to refractory leukemia, induction death, leukemic relapse at any site, death during remission, or second malignant neoplasm, whichever occurred first. Patients not experiencing an event were censored at the time of their last contact. The Kaplan-Meier life table estimate of EFS and its standard deviation (SD) are provided for selected time points. Life table comparisons of EFS outcome patterns for hypodiploid subgroups used the log-rank statistic. P values were based on the pattern of outcome across the entire period of patient follow-up. Values of .05 or less are referred to as significantly different. Numeric cutoff levels for the hypodiploid subgroups 24 to 29, 33 to 39, 40 to 43, and 44 were based on previous analyses of hypodiploid patients. In contrast to prior studies, we found that patients with 44 chromosomes constituted the largest subgroup of hypodiploid patients so they were included as a separate group.
Results
Karyotypes of hypodiploid patients
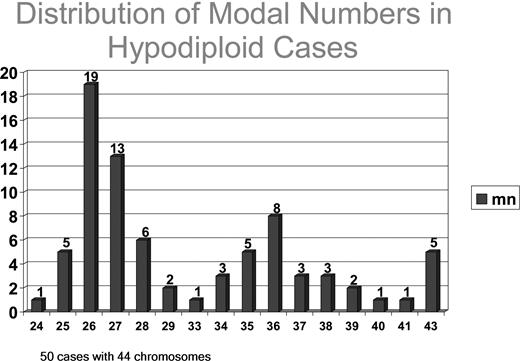
Nine of the 139 patients with hypodiploidy were Philadelphia chromosome (Ph) positive; 5 had 40 to 43 chromosomes and 4 had 44 chromosomes. These patients were not considered further, leaving 130 eligible patients who were divided into 4 groups based on modal chromosome number: 24 to 29, 33 to 39, 40 to 43, and 44 chromosomes (Table 1). For one patient in the 40 to 43 chromosome group and another in the 33 to 39 group, a modal chromosome range was provided but the actual chromosome number could not be accurately assessed. Thus, Figure 1 and the following analysis of cytogenetic features are based on 128 patients. Patients with 24 to 29 chromosomes and those with 44 chromosomes accounted for 72.3% of patients. The distribution of modal chromosome number for patients with 44 or fewer chromosomes is shown in Figure 1. No patient had a modal chromosome number of 30, 31, 32, or 42. The most common modal chromosome numbers for patients with 44 or fewer chromosomes were 44 (n = 50), 26 (n = 19), and 27 (n = 13).
Modal chromosome number for non-Ph+ ALL patients with fewer than 45 chromosomes
| Modal chromosome no. . | No. of cases . |
|---|---|
| 24 to 29 chromosomes | 46 |
| 33 to 39 chromosomes | 26 |
| 40 to 43 chromosomes | 8 |
| 44 chromosomes | 50 |
| Modal chromosome no. . | No. of cases . |
|---|---|
| 24 to 29 chromosomes | 46 |
| 33 to 39 chromosomes | 26 |
| 40 to 43 chromosomes | 8 |
| 44 chromosomes | 50 |
Distribution of modal chromosome numbers in hypodiploid cases with fewer than 44 chromosomes. There are no patients with 30, 31, 32, or 42 chromosomes. For 2 patients, modal chromosome number could not be accurately determined.
Distribution of modal chromosome numbers in hypodiploid cases with fewer than 44 chromosomes. There are no patients with 30, 31, 32, or 42 chromosomes. For 2 patients, modal chromosome number could not be accurately determined.
Cytogenetic features of hypodiploid subgroups
Forty-four chromosomes (n = 50).
Forty-nine of 50 patients had structural as well as numeric chromosome abnormalities. The most frequent monosomic chromosomes were 7, 9, 13, and X/Y. Ten patients had a dicentric chromosome. The most common structural abnormalities included loss of the short arm of chromosome 9 (9p) and an abnormal 12p. No doubling of the hypodiploid clone was seen in this group.
Forty to 43 chromosomes (n = 7).
All patients had disomies for chromosomes 2, 6, 10, 11, 20, and 22. Structural abnormalities occurred in 6 patients. No doubling of the hypodiploid clone was seen.
Thirty-three to 39 chromosomes (n = 25).
Nine patients had structural abnormalities; in 8 of these, the modal chromosome number was fewer than 36. Disomies for chromosomes 3, 7, 16, and 17 were rare. In 7 patients, doubling of the hypodiploid clone was present.
Twenty-four to 29 chromosomes (n = 46).
Thirty-three patients had only numeric abnormalities. All patients were disomic for chromosome 21. Disomies for chromosome X/Y (n = 30) and 14 and 18 (n = 24 each) were also common. Twenty-five patients had doubling of the near-haploid clone.
Clinical and biologic characteristics of patients with 44 or fewer chromosomes
Approximately 90% of patients showed a B-precursor immunophenotype; almost all were CD10+ and 8 had CNS involvement at diagnosis. Of the 8 T-cell patients, 7 had 44 chromosomes. Table 2 shows the age, white count, and sex distribution for the 130 patients.
Demographic features by modal chromosome number
| . | Modal chromosome no. . | ||||
|---|---|---|---|---|---|
| Fewer than 30 . | 33 to 39 . | 40 to 43 . | 44 . | Total . | |
| Age, y | |||||
| Younger than 1 | — | — | 1 | 2 | 3 |
| 1 to 9 | 32 | 5 | 6 | 39 | 82 |
| Older than 10 | 14 | 21 | 1 | 9 | 45 |
| WBC, × 109/L | |||||
| Less than 20 | 18 | 19 | 4 | 21 | 62 |
| 20 to less than 50 | 19 | 5 | 2 | 16 | 42 |
| 50 or more | 9 | 2 | 2 | 13 | 26 |
| Sex | |||||
| Male | 23 | 18 | 6 | 25 | 72 |
| Female | 23 | 8 | 2 | 25 | 58 |
| . | Modal chromosome no. . | ||||
|---|---|---|---|---|---|
| Fewer than 30 . | 33 to 39 . | 40 to 43 . | 44 . | Total . | |
| Age, y | |||||
| Younger than 1 | — | — | 1 | 2 | 3 |
| 1 to 9 | 32 | 5 | 6 | 39 | 82 |
| Older than 10 | 14 | 21 | 1 | 9 | 45 |
| WBC, × 109/L | |||||
| Less than 20 | 18 | 19 | 4 | 21 | 62 |
| 20 to less than 50 | 19 | 5 | 2 | 16 | 42 |
| 50 or more | 9 | 2 | 2 | 13 | 26 |
| Sex | |||||
| Male | 23 | 18 | 6 | 25 | 72 |
| Female | 23 | 8 | 2 | 25 | 58 |
— indicates not applicable.
Patients with 33 to 39 chromosomes were a unique group; 21 of 26 patients in this subgroup compared with 24 of 104 patients in the other groups were older than 10 years at diagnosis (P ≤ .001).
Only 2 of 26 patients with 33 to 39 chromosomes compared with 23 of 104 patients in the other hypodiploid subgroups had a white blood cell (WBC) count greater than 50 × 109/L (P = NS). There was also a male predominance in the patients with 33 to 39 chromosomes and in the small subgroup of patients with 40 to 43 chromosomes; patients in the fewer than 30 and 44 chromosome groups had a male to female ratio of one.
Treatment outcome and prognostic features
All 130 patients achieved a complete remission but 78 patients had a postremission event, including marrow relapse in 56 patients (51 isolated; 5 combined), CNS relapse in 10 patients, testicular relapse in 2 patients, death in initial remission in 6 patients, and second malignant neoplasm in 1 patient. The type of adverse event was unknown in 3 patients.
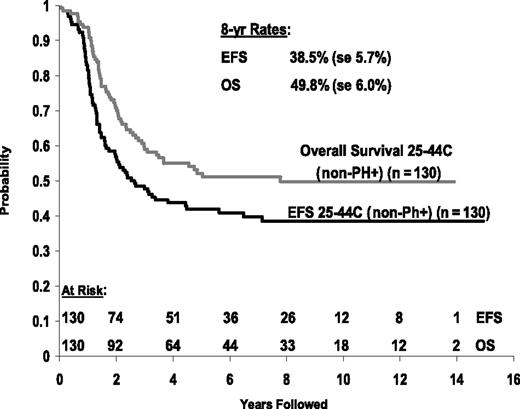
The 8-year EFS and OS for the whole group of 130 patients were 38.5% ± 5.7% and 49.8% ± 6.0%, respectively (Figure 2). Nine patients underwent bone marrow transplantation in first remission at a median of 3 months (range, 2 to 8 months) from diagnosis, and 5 of them had an adverse event after transplantation. With this relatively small number of patients, EFS and OS did not differ significantly between patients who did or did not undergo transplantation.
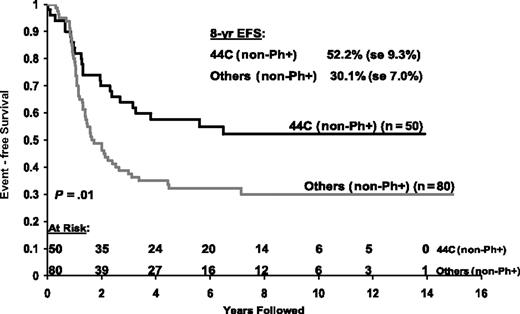
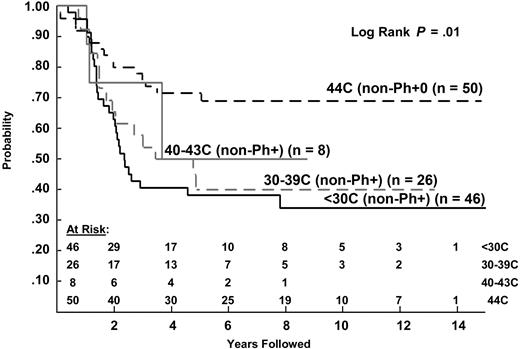
Patients with 44 chromosomes fared significantly better than those with fewer than 44 chromosomes in terms of EFS (P = .01) and OS (P = .002). The 8-year EFS was 52.2% versus 30.1%, and 8-year OS was 69% versus 37.5%, respectively (Figures 3, 4). There were no significant differences in outcome between patients with fewer than 30 chromosomes, 33 to 39 chromosomes, or 40 to 43 chromosomes (Figure 5[EFS] and Figure 6 [OS]; Table 3).
Comparison of EFS for non-Ph+ hypodiploid patients with 44 chromosomes or fewer than 44 chromosomes.
Comparison of EFS for non-Ph+ hypodiploid patients with 44 chromosomes or fewer than 44 chromosomes.
Comparison of survival for non-Ph+ hypodiploid patients with 44 chromosomes or fewer than 44 chromosomes.
Comparison of survival for non-Ph+ hypodiploid patients with 44 chromosomes or fewer than 44 chromosomes.
EFS for 130 evaluable, non-Ph+ patients by modal chromosome number: 44 chromosomes, 40 to 43 chromosomes, 30 to 39 chromosomes, and 24 to 29 chromosomes.
EFS for 130 evaluable, non-Ph+ patients by modal chromosome number: 44 chromosomes, 40 to 43 chromosomes, 30 to 39 chromosomes, and 24 to 29 chromosomes.
OS for 130 evaluable, non-Ph+ patients by modal chromosome number: 44 chromosomes, 40 to 43 chromosomes, 30 to 39 chromosomes, and 24 to 29 chromosomes.
OS for 130 evaluable, non-Ph+ patients by modal chromosome number: 44 chromosomes, 40 to 43 chromosomes, 30 to 39 chromosomes, and 24 to 29 chromosomes.
Outcome by modal chromosome number
| . | Modal chromosome no. . | |||
|---|---|---|---|---|
| Fewer than 30 . | 33 to 39 . | 40 to 43 . | 44 . | |
| No. of patients | 46 | 26 | 8 | 50 |
| Events | 33 | 16 | 6 | 23 |
| 8-year EFS, % | 28.3 ± 6.6 | 36.9 ± 9.8 | 18.7 ± 15.8 | 52.2 ± 7.4 |
| 8-year survival, % | 33.9 ± 7.6 | 40 ± 10.1 | 50 ± 17.7 | 69 ± 6.7 |
| . | Modal chromosome no. . | |||
|---|---|---|---|---|
| Fewer than 30 . | 33 to 39 . | 40 to 43 . | 44 . | |
| No. of patients | 46 | 26 | 8 | 50 |
| Events | 33 | 16 | 6 | 23 |
| 8-year EFS, % | 28.3 ± 6.6 | 36.9 ± 9.8 | 18.7 ± 15.8 | 52.2 ± 7.4 |
| 8-year survival, % | 33.9 ± 7.6 | 40 ± 10.1 | 50 ± 17.7 | 69 ± 6.7 |
For the 50 patients with 44 chromosomes, 16 had either monosomy 7, a dicentric chromosome, or both. The 8-year EFS for patients with either or both of these abnormalities was 31.2% ± 11.6% versus 68.5% ± 8.3% for those with neither abnormality (P = .025). However, the survival was 68% for both groups. There was no difference in outcome for patients with doubling of their hypodiploid clone versus those in whom a doubled clone was not observed (data not shown).
Discussion
In previous studies of ALL, outcome for patients with fewer than 46 chromosomes in their leukemic clone has been poor, ranging from 25% to 40%.4–9 In an MRC study, the 3-year EFS for the 20 children with 25 to 39 chromosomes was 29% compared with 66% for the 121 patients with 42 to 45 chromosomes.5 Only 7 children in that series had 42 to 44 chromosomes. Of these, 3 with T-cell ALL relapsed and died while 3 of the 4 patients with B-lineage ALL remained alive in continuous remission. The Children's Cancer Group reported on 23 patients with fewer than 45 chromosomes.8 The EFS for patients with 24 to 28 chromosomes and 33 to 44 chromosomes was 25% and 40%, respectively.
In this study, we collected data on patients with fewer than 45 chromosomes. This is a retrospective study with potential selection bias, and the findings reported herein need to be confirmed in prospective trials. In contrast to the MRC data, patients with 44 chromosomes (N = 50) represented the largest subgroup in our series. There were only 8 patients in the 40 to 43 chromosome group, and no patients had 30 to 32 chromosomes. We confirmed the poor outcome for patients with hypodiploidy of fewer than 45 chromosomes. The 8-year EFS and OS for the whole group of 130 hypodiploid non-Ph+ patients were only 38.5% and 49.8%, respectively (Figure 2). For patients with 24 to 43 chromosomes, 8-year EFS and OS were 30.1% and 37.5%, respectively. In contrast to previous studies suggesting that near-haploid cases with 24 to 29 chromosomes have particularly poor outcome, we found no difference in outcome between patients with 24 to 29, 33 to 39, or 40 to 43 chromosomes. A relatively favorable prognosis was observed for patients with 44 chromosomes who had an 8-year EFS of 52.2% and an 8-year OS of 69%, a finding that was not previously recognized. Moreover, within the 44 chromosome group, patients with neither a monosomy 7 nor a dicentric chromosome had significantly better EFS; albeit, there was no difference in survival compared with those with either or both abnormalities.
Doubling of a hypodiploid clone occurs frequently in patients with 24 to 29 chromosomes and less frequently in patients with 33 to 39 chromosomes. The original hypodiploid clone could be identified in all cases in which doubling occurred. Patients with doubling of a hypodiploid clone had a similar outcome to those without evidence of the doubled population, although this has not been the case in all studies (MRC and French series). Even though doubling of a hypodiploid clone has no prognostic significance among these cases, recognition of this finding is important to distinguish these patients from hyperdiploid cases who have a superior outcome and require less intensive therapy.1–8
Clearly, new treatment approaches need to be developed for the small subgroup of ALL patients with fewer than 44 chromosomes. There were no induction failures in these patients, in contrast to a high induction failure rate in other high risk subgroups such as Ph-positive patients. Whether hypodiploid cases have a high level of minimal residual disease after remission induction therapy requires further investigation. Patients with hypodiploid ALL tend to fail early in treatment (within 2 years). The efficacy of transplantation in these patients cannot be adequately addressed in this study because only 9 patients underwent this procedure. In the current Children's Oncology Group protocols, patients with hypodiploid ALL are switched to a very high-risk protocol at the end of induction featuring blocks of intensive myelosuppressive therapy (cytoxan, high-dose cytosine arabinoside, VP-16, high-dose methotrexate). Patients with a matched sibling donor are eligible to receive a bone marrow transplantation in first remission.
Acknowledgments
This work was supported in part by Cancer Center Support Grant CA21765, the American Lebanese Syrian Associated Charities, the American Cancer Society–FM Kirby Clinical Research Professorship, the Regional Grant AIRC, the Foundation Città della Speranza, PRIN, National Institutes of Health (NIH) PO1 grant CA68484, the MACC Fund, the Ponte di Legno collaboration, representing the Nordic Society of Pediatric Hematology and Oncology (NOPHO), the Swedish Children's Cancer Foundation, Leukaemia Research, United Kingdom, and NIH U10 CA 98543. A complete listing of grant support for research conducted by the Children's Cancer Group and the Pediatric Oncology Group before initiation of the Children's Oncology Group grant in 2003 is available online at http://www.childrensoncologygroup.org/admin/grantinfo.htm.
National Institutes of Health
Authorship
Contribution: All authors contributed to all aspects of preparing this paper.
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Correspondence: James Nachman, The University of Chicago Comer Children's Hospital, 5841 S Maryland Ave C-429, Chicago, IL 60637; e-mail: jnachman@peds.bsd.uchicago.edu.



This feature is available to Subscribers Only
Sign In or Create an Account Close Modal