Abstract
The ability of platelets to provide a highly reactive surface for the recruitment of other platelets and leukocytes to sites of vascular injury is critical for hemostasis, atherothrombosis, and a variety of inflammatory diseases. The mechanisms coordinating platelet-platelet and platelet-leukocyte interactions have been well defined and, in general, it is assumed that increased platelet activation correlates with enhanced reactivity toward other platelets and neutrophils. In the current study, we demonstrate a differential role for platelets in supporting platelet and neutrophil adhesive interactions under flow. We demonstrate that the conversion of spread platelets to microvesiculated procoagulant (annexin A5–positive [annexin A5+ve]) forms reduces platelet-platelet adhesion and leads to a paradoxical increase in neutrophil-platelet interaction. This enhancement in neutrophil adhesion and spreading is partially mediated by the proinflammatory lipid, platelet-activating factor (PAF). PAF production, unlike other neutrophil chemokines (IL-8, GRO-α, NAP-2, IL-1β) is specifically and markedly up-regulated in annexin A5+ve cells. Physiologically, this spatially controlled production of PAF plays an important role in localizing neutrophils on the surface of thrombi. These studies define for the first time a specific proinflammatory function for annexin A5+ve platelets. Moreover, they demonstrate an important role for platelet-derived PAF in spatially regulating neutrophil adhesion under flow.
Introduction
Platelet-platelet and platelet-leukocyte interactions have a well-defined role in a broad range of physiological functions, including hemostasis, vascular repair, host defense, inflammation, and allergic responses. Dysregulation of these adhesive interactions is also relevant to a range of human diseases, including atherosclerosis, acute myocardial infarction, ischemic stroke, acute respiratory distress syndrome, and allergic airways disease.1–3 Platelet adhesion to sites of vascular injury is initiated by subendothelial matrix proteins, including collagen and von Willebrand factor (VWF), which engage specific receptors on the platelet surface, including glycoprotein Ib (GPIb/V/IX)/GPVI, integrins αIIbβ3 and α2β1.4,5 Firm adhesion of platelets is associated with extensive cytoskeletal remodeling, resulting in spreading over the site of vascular injury. Spread platelets provide a highly reactive surface for the recruitment of other circulating blood cells, including platelets and leukocytes, due to the surface expression of various adhesive ligands (VWF, fibrinogen, fibronectin), receptors (activated integrin αIIbβ3, P-selectin),4,6,7 and prothrombotic (eg, ADP7 ) and proinflammatory (eg, IL-1β, RANTES, soluble CD40 ligand [sCD40L], NAP-2, ENA-78, LTB4, PAF8–12 ) factors.
Insight into the mechanisms regulating leukocyte adhesion to platelets has been derived principally from perfusion studies on spread platelet monolayers.13–16 Neutrophil tethering is mediated by platelet P-selectin binding to PSGL-1 on the neutrophil surface, whereas stable adhesion is dependent on leukocyte β2 integrin activation, through a process partially dependent on the generation of platelet-activating factor (PAF), followed by integrin ligation with adhesion molecules such as fibrinogen and ICAM-2.17 The mechanisms regulating neutrophil adhesion onto the surface of thrombi have been less clearly defined, although likely to be important given that the majority of leukocyte-platelet interactions in vivo occur on the surface of thrombi rather than on spread primary adherent platelets.18 In vitro perfusion studies and in vivo thrombosis models have demonstrated that forming thrombi are typically more reactive to platelets than leukocytes, at least during the early phases of thrombus development.18–20 Part of this differential reactivity may reflect the kinetics of surface expression of adhesive ligands, such as VWF, fibrinogen, and P-selectin. It is also possible that specific activating signals are generated during distinct phases of thrombus development; however to date there is limited information on the role of specific platelet chemokines in regulating the spatial and temporal aspects of leukocyte adhesion and spreading during thrombus development.
One of the most striking examples of altered platelet surface reactivity involves the calcium-dependent change in platelets from a proaggregatory to a procoagulant state.21 For example, on a potent thrombogenic matrix such as fibrillar type I collagen, primary adherent platelets initially provide a highly reactive surface for the recruitment of other platelets; however, over time, these platelets become less adhesive toward other platelets due to calcium-dependent down-regulation of integrin αIIbβ3 adhesive function. This reduction in platelet adhesiveness is associated with an up-regulation in platelet procoagulant activity, due in part to the surface expression of phosphatidylserine (recognized as annexin A5–positive [annexin A5+ve] platelets).21,22 Conversion of platelets from a proaggregatory to a procoagulant phenotype is associated with marked morphologic changes, resulting in membrane contraction, fragmentation, and the formation of phosphatidylserine-rich microvesicles. These platelets have been variously described as balloon-shaped cells with membrane blebs,22 SCIPs (sustained calcium-induced platelet morphology), COAT (collagen and thrombin activated platelets),23,24 and more recently COATED platelets,25 to reflect their surface “coating” by procoagulant protein complexes. Given their inability to support platelet-platelet adhesion under flow, we hypothesized that activated platelets that had converted to a SCIP phenotype would exhibit altered reactivity toward neutrophils.
We demonstrate here that these annexin 5A+ve platelets (referred to as SCIPs in this report) exhibit a paradoxical increase in surface reactivity toward neutrophils, leading to enhanced neutrophil adhesion and spreading. This increase in reactivity is partially dependent on the production of the proinflammatory phospholipid PAF. PAF production, in contrast to other platelet cytokines/chemokines, such as IL-8, GRO-α, NAP-2, and IL-1β, is selective to SCIPs. Our studies demonstrate that SCIP conversion represents a novel mechanism of spatially controlling leukocyte adhesion on the surface of thrombi. Moreover, they suggest that SCIP formation represents an important mechanism of coordinating the phenotypic conversion of platelets from a proaggregatory to a proinflammatory adhesive surface.
Materials and methods
Materials
Histopaque-1077, Histopaque-1119, and ionophore A23187 were from Sigma Chemical (St Louis, MO). FITC-conjugated annexin 5A was from Becton Dickinson (Franklin Lakes, NJ), and DiIC18 (1,1′-dioctadecyl-3,3,3′,3′-tetramethylindocarbocyanine perchlorate) was from Molecular Probes (Eugene, OR). The CXCR-1 and CXCR-2 blocking antibodies were from R&D Systems (Minneapolis, MN). The PAF quantitative radioimmunoassay was from Amersham BioSciences (Buckinghamshire, United Kingdom) while the enzyme-linked immunosorbent assays (ELISAs) for the quantitation of IL-8, IL-1β, GRO-α, and NAP-2 were from R&D Systems. The PAF-receptor antagonists, PCA424826 and CV3988,27 were from Biomol International (Plymouth Meeting, MA), while WEB2086 was kindly donated by Boehringer-Ingelheim (Mannheim, Germany). The LTB4 receptor antagonist, LY255283,28 was from Biomol International. All other reagents were obtained from sources described previously.21
Whole blood and blood cell preparation
All procedures were approved by the Institutional Research Board at the Australian Center for Blood Disease, Monash Medical School at Alfred Medical Research and Education Precinct. Blood was drawn from healthy consenting individuals who had not ingested any antiplatelet or anti-inflammatory medication in the 2 weeks prior to venesection into either citrate or acid-citrate-dextrose containing theophylline. Platelets were isolated from whole blood as previously described29 and finally resuspended in modified Tyrode buffer (10 mM Hepes, 12 mM NaHCO3, pH 7.4, 137 mM NaCl, 2.7 mM KCl, 5 mM glucose) that was unsupplemented or supplemented with 1 mM CaCl2/MgCl2 where indicated. Neutrophils were prepared from citrated blood using Histopaque-1077 and Histopaque-1119 as per the manufacturer's instructions. Isolated neutrophils were washed twice in Hanks balanced salt solution (HBSS; 137 mM NaCl, 5.4 mM KCl, 0.7 mM Na2HPO4, 1.2 mM NaHCO3, 27.5 mM Tris, pH 7.4, 12.2 mM dextrose). The isolated neutrophil fraction contained between 92% and 99% neutrophils that were more than 95% viable (assessed by trypan blue exclusion) with minimal red blood cell and platelet contamination as assessed by an automated cell counter. Cells were stored at room temperature for a maximum of 2 hours and resuspended in Tyrode buffer supplemented with 1 mM CaCl2/MgCl2 (1 × 106/mL) prior to experimentation.
Perfusion studies
All perfusion studies in this report used glass microcapillaries that were acid-cleaned, extensively washed, and dried thoroughly before use.30
Platelet monolayer studies.
Washed platelets (2.5 × 108/mL) in unsupplemented Tyrode buffer were allowed to form monolayers in microcapillary tubes for 30 minutes at 37°C followed by blocking with 3% human serum albumin (HSA) for 15 minutes. Unbound albumin was removed by gentle flushing of the microcapillaries with unsupplemented Tyrode buffer. To induce SCIP conversion, spread platelet monolayers were exposed to Tyrode buffer containing 1 μM ionophore A23187 and 1 mM CaCl2/MgCl2 for 10 minutes prior to ionophore removal21 and blocking with 3% HSA.
Isolated neutrophils (1 × 106/mL) in Tyrode buffer supplemented with 1 mM CaCl2/MgCl2 were perfused over spread or SCIP monolayers at 150 s−1 for 5 minutes at 37°C. In some studies, neutrophils were pretreated with isotype control or anti–CXCR-1 or anti–CXCR-2 blocking antibodies (20 μg/mL) for 30 minutes prior to perfusion. In experiments examining the effect of PAF receptor antagonism on neutrophil-platelet adhesion dynamics, isolated neutrophils were pretreated with either vehicle (Me2SO) or WEB2086 (30 μM) for 5 minutes prior to perfusion over spread or SCIP monolayers. Neutrophil-platelet interactions were visualized using phase video microscopy (10× lens, Leica DMIRB; Leica, Heidelberg, Germany) and recorded at various times throughout perfusion for off-line analysis. Alternatively, after some perfusion experiments, samples were fixed and prepared for scanning electron microscopy as described.21
Platelet thrombi studies.
Citrated whole blood was perfused through VWF (100 μg/mL) or type I collagen–coated (2 mg/mL) microcapillary tubes for 5 minutes at 1800 s−1, and nonadherent cells were removed by perfusion of cell-free Tyrode buffer in the absence or presence of extracellular CaCl2 (1 mM) for a further 5 minutes. Isolated neutrophils (1 × 106/mL) in Tyrode buffer supplemented with 1 mM CaCl2/MgCl2 were then perfused over the preformed thrombi and leukocyte-platelet interactions visualized by real-time video microscopy and recorded for off-line analysis. In some experiments, whole blood was perfused in the presence of 5 μg/mL FITC–annexin 5A and neutrophils were prestained with DiIC18 (1 μM) for 10 minutes prior to flow. These cells were then visualized by multichannel confocal microscopy (20× lens, Zeiss Meta 510; Zeiss, Heidelberg, Germany) and images overlaid using Zeiss imaging software. PAF receptor blockade in thrombi studies was carried out using the following concentrations of antagonists: WEB2086 (30 μM), PCA-4248 (5 μM), CV-3988 (5 μM), or LY255283 (20 μM).
Quantitation of platelet chemokines
Quantitation of soluble chemokines released from activated platelets.
Commercially available DuoSet ELISA kits from R&D Systems were used to quantitate the levels of released NAP-2, GRO-α, IL-8, and IL-1β. These molecules are classically soluble factors released from cells upon appropriate stimulation. To obtain platelet releasates, isolated platelets were resuspended in Tyrode buffer containing either 1 mM CaCl2 or 1 mM EGTA and 2 mM MgCl2. Platelets were left unstimulated or stimulated with thrombin (1 U/mL) or ionophore A23187 (1 μM) for 15 minutes. Platelets were then pelleted at 2000g in the presence of 10 mM theophylline, and the resulting supernatant (releasate) was aspirated and frozen until use.
Quantitation of PAF in activated platelets.
A commercial PAF assay kit was used to measure PAF generation in adherent platelets following the manufacturer-provided protocol. PAF is typically localized to cell membranes, and thus PAF generation in our experiments was measured under conditions optimized for platelet membrane harvest. Briefly, platelets resuspended in Tyrode buffer (2.5 × 108/mL) were allowed to adhere and spread onto collagen type I–coated 10-cm glass dishes in the absence or presence of extracellular calcium for 60 minutes at 37°C. In some studies, SCIP formation was induced in 100% of adherent cells by the addition of ionophore A23187 (1 μM) and 1 mM CaCl2 for 10 minutes following the 60-minute adhesion period. Following removal of nonadherent platelets, membrane lipids were then extracted from adherent platelets (2 × 108/dish) using the method of Bligh and Dyer.31 The organic phases were then dried under a stream of N2 and subjected to thin layer chromatography (TLC), alongside 1 μg authentic PAF, using a methanol-chloroform-water (65:35:6) development solution for 70 minutes. Authentic PAF on the TLC plate was visualized using iodine vapor, and the areas (1.5 cm2) of the TLC plate containing sample lipids corresponding to the PAF standard were scraped and extracted into pure chloroform, dried under N2, and reconstituted in assay buffer for quantitation by the commercial radioimmunoassay (RIA) kit. Results are presented as picogram of PAF produced per 108 platelets. In control experiments, we confirmed that other cellular lipids related to PAF (such as oleayl acetyl glycerol) did not comigrate with PAF by TLC (Figure S2, available on the Blood website; see the Supplemental Materials link at the top of the online article). Furthermore, using sensitive, quantitative liquid chromatography/mass spectrometry (LC/MS) techniques, we confirmed that platelet-derived PAF (PAF C:18) was indeed the major lipid from the area scraped from the TLC plate prior to RIA, which increased upon conversion of platelets to SCIPs (Figure S1).
Image analysis
The following parameters were used to identify various subsets of neutrophil adhesive behavior under flow. A cell was deemed as tethered if it maintained its first adhesive contact with immobilized platelets for at least 40 ms. Cells maintaining a single adhesive contact for at least 10 seconds were scored as stationary adherent cells. Neutrophils were scored as spread once lamellipodial membrane extension from the entire membrane periphery was observed, and under phase microscopy, neutrophils lost their phase bright appearance and adopted a phase dark morphology (typically associated with close cell apposition to an immobile surface and spreading).
Image acquisition information
Differential interference contrast (DIC) image acquisition for Figure 2 was taken using a Leica DMIRB (Leica, Heidelberg, Germany) with a 40×/0.6 NA lens coupled to a DAGE-MTI RC300 CCD camera (Dage-MTI, Michigan City, IN) and digitalized using Image Pro Plus version 6.2 (MediaCybernetics, Silver Spring, MD). For Figure 3C, images were taken using a Zeiss Meta 510 confocal microscopy (Zeiss, Melbourne, Australia) with a 20×/0.45 NA lens and images overlaid using Zeiss imaging software (Axiovision LE version 4.5; Zeiss). Neutrophils were prestained before perfusion with DiIC18 as described in “Materials and methods, Perfusion studies” (Invitrogen, Carlsbad, CA). Scanning electron microscopy (SEM) images (Figure 4A,B) were acquired using a Hitachi S570 system (Hitachi, Tokyo, Japan).
Results
Effect of matrix reactivity on neutrophil adhesion to the surface of platelet thrombi
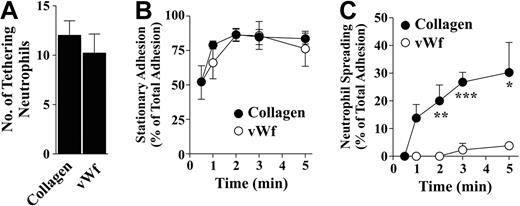
Platelet adhesion to distinct thrombogenic surfaces induces variable levels of platelet activation and thrombus growth, with the level of activation in primary adherent platelets having a major impact on subsequent platelet recruitment.32 Whether differences in the level of platelet activation have a significant influence on neutrophil recruitment has not been established. To investigate this, we performed neutrophil perfusion studies on thrombi formed on a type I fibrillar collagen substrate or a purified VWF matrix. We chose VWF and type I fibrillar collagen for these studies as they represent the 2 extremes of matrix reactivity, with the former inducing weak platelet activation and limited thrombus growth, whereas the latter induces the rapid formation of large platelet thrombi.32 As demonstrated in Figure 1A, platelet thrombi on either thrombogenic surface were equally effective at promoting initial neutrophil tethering (collagen: 10.2 ± 1.3 × 102/mm2; VWF: 8.7 ± 1.6 × 102/mm2) and firm adhesion (Figure 1B). However, thrombi formed on a collagen substrate were more effective at promoting neutrophil spreading with 30.3% (± 10.8%; n = 4) of adherent neutrophils spread on collagen-formed thrombi compared with only 2.8% (± 1.2%; n = 4) on VWF thrombi (Figure 1C). Although neutrophils did not spread on VWF thrombi, more than 90% of neutrophils changed shape and extended transient polarized lamellae (Video S1). In addition to being more effective at inducing neutrophil spreading, collagen-formed thrombi induced a distinct spatial pattern of neutrophil spreading. Specifically, we found that the highest proportion of spread neutrophils occurred on the outer margins of thrombi with very few spread neutrophils on the apical surface (Figure 2). These studies demonstrate that platelets can induce heterogeneous neutrophil spreading responses that are partly dependent on the nature of thrombogenic substrate and also by the spatial distribution of platelets within a thrombus. In control studies, we confirmed that neutrophil tethering to spread platelets and formed thrombi was P-selectin dependent under all experimental conditions studied, as it was completely eliminated by a P-selectin blocking antibody (data not shown), whereas firm adhesion was blocked by functional blocking anti-β2 integrin antibody (data not shown).
Differential abilities of collagen- and VWF-bound thrombi to induce neutrophil spreading under flow. Citrated whole blood was perfused over either VWF (100 μg/mL) or collagen (2 mg/mL) matrices for 5 minutes at 1800 s−1 to obtain platelet thrombi. Nonadherent platelets were removed by a further 5-minute perfusion with cell-free unsupplemented Tyrode buffer at 1800 s−1 followed by perfusion of isolated neutrophils (1 × 106/mL) in Tyrode buffer supplemented with 1 mM CaCl2/MgCl2 for 5 minutes at 150 s−1. Neutrophil-platelet interactions were visualized by phase-contrast microscopy and the number of neutrophils tethering in the first 30 seconds of perfusion (A), the proportion of tethering neutrophils forming stationary adhesion contacts (B), and the proportion of tethered neutrophils exhibiting spreading (C) were quantitated. Results are presented as means (± SEM; n = 4). *P < .05, **P < .01, ***P < .001.
Differential abilities of collagen- and VWF-bound thrombi to induce neutrophil spreading under flow. Citrated whole blood was perfused over either VWF (100 μg/mL) or collagen (2 mg/mL) matrices for 5 minutes at 1800 s−1 to obtain platelet thrombi. Nonadherent platelets were removed by a further 5-minute perfusion with cell-free unsupplemented Tyrode buffer at 1800 s−1 followed by perfusion of isolated neutrophils (1 × 106/mL) in Tyrode buffer supplemented with 1 mM CaCl2/MgCl2 for 5 minutes at 150 s−1. Neutrophil-platelet interactions were visualized by phase-contrast microscopy and the number of neutrophils tethering in the first 30 seconds of perfusion (A), the proportion of tethering neutrophils forming stationary adhesion contacts (B), and the proportion of tethered neutrophils exhibiting spreading (C) were quantitated. Results are presented as means (± SEM; n = 4). *P < .05, **P < .01, ***P < .001.
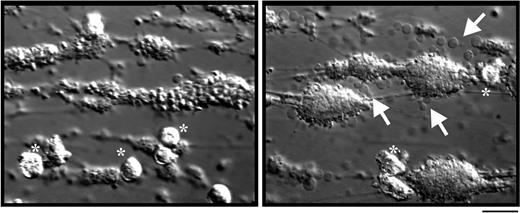
Neutrophil spreading occurs on spatially distinct areas of collagen thrombi. Citrated whole blood was perfused over a collagen (2 mg/mL) matrix for 5 minutes at 1800 s−1 to obtain platelet thrombi. Nonadherent platelets were removed by a further 5-minute perfusion with cell-free unsupplemented Tyrode buffer at 1800 s−1 followed by perfusion of isolated neutrophils (1 × 106/mL) in Tyrode buffer supplemented with 1 mM CaCl2/MgCl2 for 5 minutes at 150 s−1. Neutrophil-thrombus interactions were visualized by differential interference contrast (DIC) microscopy at a high (at the apex of thrombi; image on left) or low (to image the sides of thrombi; image on right) focal plane. These images are from 1 experiment representative of more than 10 independent experiments. Neutrophils in images are identified by asterisks. Arrows indicate the presence of SCIP, particularly prominent around the side of the thrombi. Bar represents 30 μm.
Neutrophil spreading occurs on spatially distinct areas of collagen thrombi. Citrated whole blood was perfused over a collagen (2 mg/mL) matrix for 5 minutes at 1800 s−1 to obtain platelet thrombi. Nonadherent platelets were removed by a further 5-minute perfusion with cell-free unsupplemented Tyrode buffer at 1800 s−1 followed by perfusion of isolated neutrophils (1 × 106/mL) in Tyrode buffer supplemented with 1 mM CaCl2/MgCl2 for 5 minutes at 150 s−1. Neutrophil-thrombus interactions were visualized by differential interference contrast (DIC) microscopy at a high (at the apex of thrombi; image on left) or low (to image the sides of thrombi; image on right) focal plane. These images are from 1 experiment representative of more than 10 independent experiments. Neutrophils in images are identified by asterisks. Arrows indicate the presence of SCIP, particularly prominent around the side of the thrombi. Bar represents 30 μm.
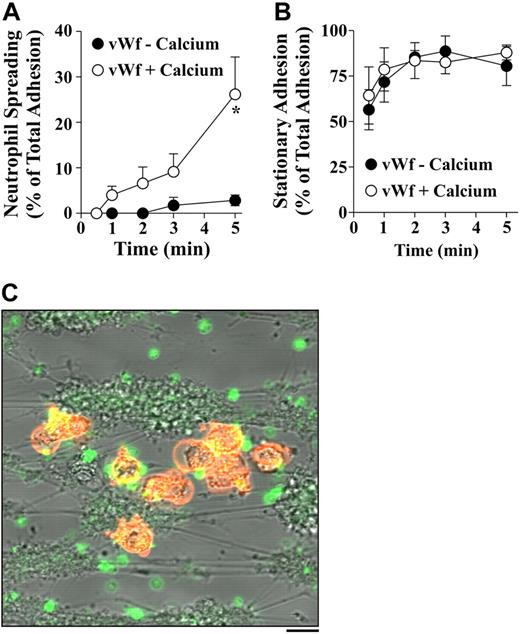
Platelet exposure to extracellular calcium facilitates neutrophil spreading.
The only experimental condition in which VWF thrombi induced a marked increase in neutrophil spreading was when thrombi underwent exposure to calcium-containing buffers (“Materials and methods, Perfusion studies, Platelet thrombi studies”) prior to neutrophil perfusion (note: all neutrophil perfusions occurred in the presence of calcium) (Figure 3A). Under these conditions, there was an approximately 10-fold increase in the proportion of spread neutrophils on VWF thrombi. Similarly, prior exposure of collagen-formed thrombi to extracellular calcium induced a significant increase in neutrophil spreading (from 30.2% ± 10.8% to 69% ± 4.2% by 5 minutes of perfusion [n = 4]). This calcium effect was specific to spreading as there was no difference in neutrophil tethering (data not shown) or stationary adhesion (Figure 3B). Furthermore, the effects of calcium were likely to be principally on platelets rather than on neutrophils, as all calcium-dependent changes were related to the time of platelet exposure to extracellular calcium (data not shown).
Exposure of VWF thrombi to extracellular calcium induces spreading in tethering neutrophils. (A,B) Citrated whole blood was perfused over a VWF (100 μg/mL) matrix for 5 minutes at 1800 s−1 to obtain platelet thrombi. Nonadherent platelets were removed by a further 5-minute perfusion with cell-free unsupplemented Tyrode buffer (VWF − calcium) or buffer supplemented with at 1800 s−1 with 1 mM CaCl2/MgCl2 (VWF + calcium) for 5 minutes prior to perfusion of isolated neutrophils (1 × 106/mL) resuspended in 1 mM CaCl2/MgCl2-containing Tyrode buffer for 5 minutes at 150 s−1. Neutrophil-platelet interactions were visualized by phase contrast microscopy and the number of neutrophils exhibiting spreading (A) and stationary adhesion (B) quantitated. Results are presented as means (± SEM; n = 4). *P < .05. (C) Citrated whole blood was perfused over collagen (2 mg/mL) in the presence of FITC–annexin 5A (5 μg/mL) (green) and neutrophils were stained with DiIC18 (1 μM) (orange) prior to perfusion as described in “Materials and methods, Perfusion studies, Platelet thrombi studies.” Platelets and neutrophils were simultaneously visualized using filters for DIC, and green and red fluorescence, by confocal microscopy. Image overlay is from 1 experiment representative of 4 independent experiments. Bar represents 30 μm.
Exposure of VWF thrombi to extracellular calcium induces spreading in tethering neutrophils. (A,B) Citrated whole blood was perfused over a VWF (100 μg/mL) matrix for 5 minutes at 1800 s−1 to obtain platelet thrombi. Nonadherent platelets were removed by a further 5-minute perfusion with cell-free unsupplemented Tyrode buffer (VWF − calcium) or buffer supplemented with at 1800 s−1 with 1 mM CaCl2/MgCl2 (VWF + calcium) for 5 minutes prior to perfusion of isolated neutrophils (1 × 106/mL) resuspended in 1 mM CaCl2/MgCl2-containing Tyrode buffer for 5 minutes at 150 s−1. Neutrophil-platelet interactions were visualized by phase contrast microscopy and the number of neutrophils exhibiting spreading (A) and stationary adhesion (B) quantitated. Results are presented as means (± SEM; n = 4). *P < .05. (C) Citrated whole blood was perfused over collagen (2 mg/mL) in the presence of FITC–annexin 5A (5 μg/mL) (green) and neutrophils were stained with DiIC18 (1 μM) (orange) prior to perfusion as described in “Materials and methods, Perfusion studies, Platelet thrombi studies.” Platelets and neutrophils were simultaneously visualized using filters for DIC, and green and red fluorescence, by confocal microscopy. Image overlay is from 1 experiment representative of 4 independent experiments. Bar represents 30 μm.
High magnification imaging of thrombi formed on a VWF matrix revealed that prolonged exposure to calcium buffers induced microvesiculation and fragmentation in a subset of primary adherent platelets. Similarly, on thrombi formed on a collagen matrix, a high proportion of the platelets on the side of thrombi (the precise regions where neutrophils had spread) had microvesiculated and fragmented (Figure 2 arrows). This calcium-dependent change in platelet morphology has been well defined and is associated with phosphatidylserine expression on the cell surface (annexin 5A+ve cells).21,22 We have recently termed this platelet morphology as SCIP, referring to sustained calcium-induced change in platelet morphology21 and demonstrated that they have a selective defect in their ability to support stable platelet adhesive interactions under flow. Prolonged exposure of formed thrombi to calcium-containing buffers resulted in a marked increase in FITC–annexin 5A+ve platelets, from 3.64 (+ 2.1; n = 3) up to 38.81 (+ 5.1; n = 3) platelets per field on a VWF matrix. Furthermore, spread neutrophils colocalized with FITC–annexin 5A+ve platelets on the margins of thrombi, as well as on the surface of individual primary adherent platelets (Figure 3C). Collectively, these studies suggest a potentially important role for SCIPs in promoting neutrophil spreading under flow.
SCIP monolayers induce neutrophil spreading under flow
To investigate the functional relationship between SCIPs and neutrophil adhesion in further detail, we examined the ability of purified neutrophils to adhere and spread onto monolayers composed entirely of intact spread platelets or SCIPs (Figure 4A,B micrographs). The formation and characterization of these monolayers is presented in “Perfusion studies” and has been described in detail elsewhere.21 There was little difference in the ability of either spread or SCIP monolayers to support the initial tethering or adhesion of neutrophils under flow (data not shown). However we observed that monolayers composed entirely of SCIPs were more efficient at inducing firm neutrophil adhesion during the early stages of neutrophil perfusion and unlike spread platelets were able to induce spreading in adherent neutrophils (Figure 4C). Real-time analysis of neutrophil adhesion to spread platelets revealed that neutrophils converted from round to polarized forms and were able to extend short “fanlike” membrane extensions from a single region of the cell membrane within 1 to 3 minutes of cell arrest. However, these extensions were typically transient in nature, resulting in less than 2% of neutrophils adopting a fully spread morphology (Video S2). In contrast, upon firm adhesion to SCIPs, neutrophils underwent a rapid change in shape, sometimes within 30 seconds of adhesion, extending lamellar membranes from the entire cell periphery, eventually adopting a fully spread morphology (Video S3). These studies confirm an important role for SCIPs in promoting neutrophil spreading under flow.
SCIPs, but not spread platelets, induce neutrophil spreading under flow. Washed platelets (2.5 × 108/mL) in unsupplemented Tyrode buffer were allowed to form monolayers in glass microcapillary tubes for 30 minutes at 37°C followed by blocking with 3% HSA for 15 minutes. Monolayers were left untreated (Spread) or pretreated with 1 μM ionophore A23187 for 10 minutes followed by ionophore removal with cell-free buffer to convert spread platelets to SCIPs (SCIP). Isolated neutrophils (106/mL) were then perfused over the monolayers at 150 s−1 for 5 minutes. (A) Scanning electron microscopy images of spread platelet and SCIP monolayers prior to neutrophil perfusion. (B) Scanning electron microscopy images of neutrophils that have interacted with Spread platelet or SCIP monolayers. (C) Neutrophil-platelet interactions were visualized by phase-contrast microscopy and the proportion of adherent neutrophils exhibiting stationary (i) or spread (ii) morphology quantitated. Images in panels A and B are representative of more than 10 individual experiments. Bar is 5 μm. Results in C are expressed as mean (±SEM; n = 4). *P < .05, **P < .01, ***P < .001.
SCIPs, but not spread platelets, induce neutrophil spreading under flow. Washed platelets (2.5 × 108/mL) in unsupplemented Tyrode buffer were allowed to form monolayers in glass microcapillary tubes for 30 minutes at 37°C followed by blocking with 3% HSA for 15 minutes. Monolayers were left untreated (Spread) or pretreated with 1 μM ionophore A23187 for 10 minutes followed by ionophore removal with cell-free buffer to convert spread platelets to SCIPs (SCIP). Isolated neutrophils (106/mL) were then perfused over the monolayers at 150 s−1 for 5 minutes. (A) Scanning electron microscopy images of spread platelet and SCIP monolayers prior to neutrophil perfusion. (B) Scanning electron microscopy images of neutrophils that have interacted with Spread platelet or SCIP monolayers. (C) Neutrophil-platelet interactions were visualized by phase-contrast microscopy and the proportion of adherent neutrophils exhibiting stationary (i) or spread (ii) morphology quantitated. Images in panels A and B are representative of more than 10 individual experiments. Bar is 5 μm. Results in C are expressed as mean (±SEM; n = 4). *P < .05, **P < .01, ***P < .001.
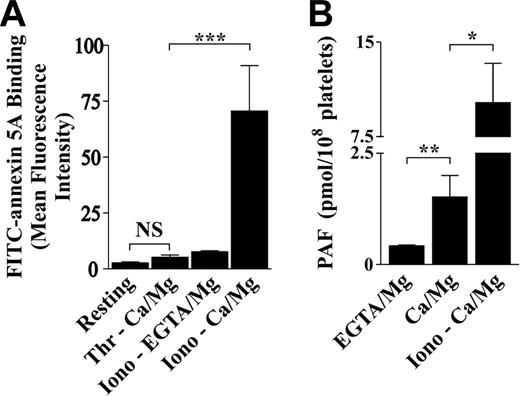
PAF promotes neutrophil spreading on SCIP monolayers
It is well known that platelets generate a number of proinflammatory molecules that act as potent activators of leukocytes, including IL-8, IL-1β, NAP-2, GRO-α, and PAF.12 Many of these factors are known to be released from activated platelets, acting as soluble costimuli enhancing the activation status of adherent leukocytes. To investigate whether SCIP conversion was specifically associated with the production of these chemokines, quantitative analysis of IL-8, GRO-α, IL-1β, or NAP-2 levels was performed on resting, thrombin- or ionophore A23187–stimulated platelets (in the presence of CaCl2/MgCl2 [annexin 5A+ve] or EGTA/MgCl2 [annexin 5A−ve]) (Figure 5A). As demonstrated in Table 1, there was an increase in the levels of soluble NAP-2 following platelet activation by thrombin or ionophore A23187; however, this increase was unrelated to SCIPs, as chelators of extracellular calcium had no inhibitory effect on NAP-2 levels. Notably, under the experimental conditions used here, we did not observe an increase in IL-8, IL-1β, or GRO-α levels in the releasates of platelets stimulated with either thrombin or ionophore A23187 (Table 1). Further evidence suggesting that a soluble chemokine was unlikely to be principally responsible for neutrophil spreading was the demonstration that the releasate from thrombin-stimulated platelets was unable to induce neutrophil spreading on spread platelet monolayers under flow (data not shown).
PAF formation specifically correlates with SCIP formation. (A) Washed platelets (5 × 107/mL) were resuspended in Tyrode buffer containing either 1 mM CaCl2/MgCl2 (Ca/Mg) or 1 mM EGTA and 2 mM MgCl2 (EGTA/Mg). Platelets were left unstimulated (Resting) or stimulated with 1 U/mL thrombin (Thr) or 1 μM ionophore A23187 (Iono) for 15 minutes at 37°C in the presence of 5 μg/mL FITC–annexin 5A. Platelets were then subjected to fluorescence-activated cell sorting (FACS) and the geometric mean of the fluorescence intensity per sample was calculated. Results are presented as means (± SEM; n = 4). NS indicates no significant difference; ***P < .001. (B) Washed platelets (2.5 × 108/mL) were resuspended in Tyrode buffer containing either 1 mM CaCl2/MgCl2 (Ca/Mg) or 1 mM EGTA and 2 mM MgCl2 (EGTA/Mg). Platelets were allowed to adhere to collagen-coated (2 mg/mL) 10-cm glass dishes to form monolayers for 30 minutes at 37°C. To obtain monolayers comprising 100% SCIPs, collagen-adherent platelets were exposed to 1 μM ionophore A23817 in the presence of calcium for 10 minutes (Iono − Ca/Mg). Nonadherent platelets were removed and the membrane lipids from the adherent platelets extracted and the level of PAF quantitatively assessed as described in “Materials and methods, Quantitation of platelet chemokines.” Results are expressed as means (± SEM; n = 3). *P < .05, **P < .01.
PAF formation specifically correlates with SCIP formation. (A) Washed platelets (5 × 107/mL) were resuspended in Tyrode buffer containing either 1 mM CaCl2/MgCl2 (Ca/Mg) or 1 mM EGTA and 2 mM MgCl2 (EGTA/Mg). Platelets were left unstimulated (Resting) or stimulated with 1 U/mL thrombin (Thr) or 1 μM ionophore A23187 (Iono) for 15 minutes at 37°C in the presence of 5 μg/mL FITC–annexin 5A. Platelets were then subjected to fluorescence-activated cell sorting (FACS) and the geometric mean of the fluorescence intensity per sample was calculated. Results are presented as means (± SEM; n = 4). NS indicates no significant difference; ***P < .001. (B) Washed platelets (2.5 × 108/mL) were resuspended in Tyrode buffer containing either 1 mM CaCl2/MgCl2 (Ca/Mg) or 1 mM EGTA and 2 mM MgCl2 (EGTA/Mg). Platelets were allowed to adhere to collagen-coated (2 mg/mL) 10-cm glass dishes to form monolayers for 30 minutes at 37°C. To obtain monolayers comprising 100% SCIPs, collagen-adherent platelets were exposed to 1 μM ionophore A23817 in the presence of calcium for 10 minutes (Iono − Ca/Mg). Nonadherent platelets were removed and the membrane lipids from the adherent platelets extracted and the level of PAF quantitatively assessed as described in “Materials and methods, Quantitation of platelet chemokines.” Results are expressed as means (± SEM; n = 3). *P < .05, **P < .01.
Platelet chemokine production in response to agonist stimulation
| . | NAP-2 . |
|---|---|
| Resting | 0.12 ± 0.06 |
| Iono + EGTA/Mg | 1.17 ± 0.76* |
| Thr + Ca/Mg | 1.09 ± 0.36* |
| Iono + Ca/Mg | 1.11 ± 0.85* |
| . | NAP-2 . |
|---|---|
| Resting | 0.12 ± 0.06 |
| Iono + EGTA/Mg | 1.17 ± 0.76* |
| Thr + Ca/Mg | 1.09 ± 0.36* |
| Iono + Ca/Mg | 1.11 ± 0.85* |
GRO-α, IL-1β, and IL-8 were not detectable. All units of measure are ng/108 platelets.
P < .05 (cf with resting).
In contrast to soluble chemokines, the levels of the membrane-bound proinflammatory lipid, PAF, correlated with SCIP formation. For example, there was minimal increase in PAF levels following platelet adhesion to collagen in the presence of EGTA/MgCl2, a condition that induces potent platelet activation but not SCIP formation.21 However, ionophore A23187 stimulation of collagen-adherent platelets, in the presence of extracellular calcium, resulted in a marked increase in PAF production (Figure 5B). When platelets were allowed to adhere to collagen in the presence of extracellular calcium for 30 minutes, which leads to about 40% to 45% SCIP conversion,21 an intermediate level of PAF production was observed. These studies indicate that PAF production correlates closely with SCIP conversion of platelets.
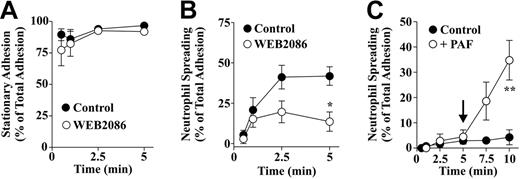
To examine the functional importance of PAF in promoting neutrophil spreading on SCIP monolayers, the effects of the PAF receptor antagonist, WEB2086, were examined. Blockade of the PAF receptor did not affect the ability of neutrophils to tether (12.2 ± 12 × 102/mm2 vs 12.3 ± 10.9 × 102/mm2, n = 4 on intact spread platelets; 10.4 ± 13.9 × 102/mm2 vs 10.1 ± 1.9 × 102/mm2, n = 4 on SCIP monolayers) or adhere to the surface of spread platelet or SCIP monolayers (Figure 6A). However, WEB2086 significantly inhibited subsequent neutrophil spreading (Figure 6B). Furthermore, perfusion of soluble PAF over neutrophils adherent to spread monolayers induced spreading in the majority of adherent neutrophils (Figure 6C). In control studies, we demonstrated that antagonism of CXCR1 and CXCR2 (neutrophil receptors for NAP-2 and IL-812,33 ) using function blocking antibodies had no effect on neutrophil adhesion on SCIP monolayers (data not shown). These studies define a major role for PAF in promoting neutrophil spreading on the surface of SCIP monolayers.
PAF receptor inhibition with WEB2086 specifically inhibits neutrophil spreading on SCIP monolayers. (A,B) Isolated neutrophils (1 × 106/mL) in Tyrode buffer containing 1 mM CaCl2/MgCl2 were pretreated with Me2SO (Control) or 30 μM of the PAF receptor antagonist, WEB2086, for 5 minutes prior to perfusion over SCIP monolayers at 150 s−1 for 5 minutes. Neutrophil-platelet monolayer interactions were visualized by phase-contrast microscopy and the proportion of adherent neutrophils forming stationary adhesion contacts or spreading was quantitated. Results are presented as means (± SEM; n = 4). *P < .05. (C) Isolated neutrophils were perfused over spread platelet monolayers at 150 s−1 for 5 minutes. At the end of the 5-minute cell perfusion, Tyrode buffer supplemented with vehicle (Control) or exogenous PAF (+ PAF) (700 nM) was perfused over adherent neutrophils for 5 minutes. The proportion of neutrophils exhibiting spreading was quantitated over the 10-minute perfusion period. Results are presented as means (± SEM; n = 4). **P < .01.
PAF receptor inhibition with WEB2086 specifically inhibits neutrophil spreading on SCIP monolayers. (A,B) Isolated neutrophils (1 × 106/mL) in Tyrode buffer containing 1 mM CaCl2/MgCl2 were pretreated with Me2SO (Control) or 30 μM of the PAF receptor antagonist, WEB2086, for 5 minutes prior to perfusion over SCIP monolayers at 150 s−1 for 5 minutes. Neutrophil-platelet monolayer interactions were visualized by phase-contrast microscopy and the proportion of adherent neutrophils forming stationary adhesion contacts or spreading was quantitated. Results are presented as means (± SEM; n = 4). *P < .05. (C) Isolated neutrophils were perfused over spread platelet monolayers at 150 s−1 for 5 minutes. At the end of the 5-minute cell perfusion, Tyrode buffer supplemented with vehicle (Control) or exogenous PAF (+ PAF) (700 nM) was perfused over adherent neutrophils for 5 minutes. The proportion of neutrophils exhibiting spreading was quantitated over the 10-minute perfusion period. Results are presented as means (± SEM; n = 4). **P < .01.
Importance of PAF for neutrophil spreading on the surface of thrombi
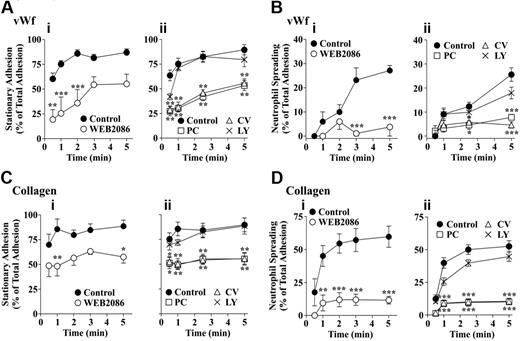
To investigate the significance of SCIP-derived PAF in promoting neutrophil adhesion and spreading on the surface of preformed thrombi, WEB2086-treated neutrophils were perfused over collagen- or VWF-formed thrombi. (Note: In these experiments all preformed thrombi were exposed to calcium-containing buffers prior to the perfusion of neutrophils.) Inhibiting the PAF receptor with WEB2086 had minimal effects on the total number of neutrophils adhering to the surface of thrombi formed on VWF or collagen (eg, at 5 minutes 7.12 ± 1.2 × 102/mm2 vehicle-treated or 7.7 ± 0.8 × 102/mm2 [n = 4] WEB2086-treated neutrophils adhered to collagen thrombi). However, in contrast to the platelet monolayers, we found that PAFR antagonism had a significant effect on the ability of tethering neutrophils to form firm adhesion contacts with the thrombus surface (Figure 7Ai,Ci). Notably, this effect was more obvious on VWF thrombi than collagen thrombi even though the level of stationary adhesion was similar on both matrices. Similar to the findings on platelet monolayers, inhibiting the PAF receptor markedly reduced the proportion of spread neutrophils on the surface of either VWF- or collagen-formed thrombi (Figure 7Bi,Di). To eliminate the possibility that the PAFR antagonists were nonspecifically blocking other bioactive lipid pathways, such as the LTB4 receptor, we also performed studies using LY255283 at concentrations known to effectively inhibit LTB4 receptor activity28 and found no effects on neutrophil adhesive or spreading behavior on VWF or collagen thrombi (Figure 7Aii,Bii,Cii,Dii). Furthermore, 2 additional structurally unrelated PAF receptor antagonists (PCA-4248 or CV-3988) had similar inhibitory effects on neutrophil adhesion and spreading as WEB2086 (Figure 7Aii,Bii,Cii,Dii). Collectively, our data supports an important role for PAF in promoting neutrophil spreading.
PAF plays a major role in supporting neutrophil adhesive behavior on the surface of thrombi. Citrated whole blood was perfused over a (A,B) VWF (100 μg/mL) or (C,D) collagen type I (2 mg/mL) for 5 minutes at 1800 s−1 to form thrombi followed by perfusion of cell-free Tyrode buffer supplemented with 1 mM CaCl2/MgCl2 for 5 minutes. Isolated neutrophils (1 × 106/mL) resuspended in supplemented Tyrode buffer were pretreated with Me2SO (Control) or PAF receptor antagonists WEB2086 (30 μM), PC-4248 (PC; 5 μM), CV-3988 (CV; 5 μM), or the LTB4 receptor antagonist, LY255283 (LY; 20 μM), for 5 minutes prior to perfusion over VWF or collagen thrombi. Neutrophil-thrombus interactions were visualized by phase contrast microscopy and the proportion of adherent neutrophils forming firm adhesion contacts (A,C) and spreading (B,D) was quantitated. Results are presented as means (± SEM; n = 2-4). *P < .05, **P < .01, ***P < .001.
PAF plays a major role in supporting neutrophil adhesive behavior on the surface of thrombi. Citrated whole blood was perfused over a (A,B) VWF (100 μg/mL) or (C,D) collagen type I (2 mg/mL) for 5 minutes at 1800 s−1 to form thrombi followed by perfusion of cell-free Tyrode buffer supplemented with 1 mM CaCl2/MgCl2 for 5 minutes. Isolated neutrophils (1 × 106/mL) resuspended in supplemented Tyrode buffer were pretreated with Me2SO (Control) or PAF receptor antagonists WEB2086 (30 μM), PC-4248 (PC; 5 μM), CV-3988 (CV; 5 μM), or the LTB4 receptor antagonist, LY255283 (LY; 20 μM), for 5 minutes prior to perfusion over VWF or collagen thrombi. Neutrophil-thrombus interactions were visualized by phase contrast microscopy and the proportion of adherent neutrophils forming firm adhesion contacts (A,C) and spreading (B,D) was quantitated. Results are presented as means (± SEM; n = 2-4). *P < .05, **P < .01, ***P < .001.
Discussion
The studies reported here define a novel functional role for annexin 5A+ve platelets in regulating neutrophil adhesion and spreading. More specifically, we have demonstrated that the calcium-dependent conversion of spread platelets to microvesiculated forms (SCIPs) is important for enabling neutrophil spreading under flow. This change in platelet surface reactivity is partially dependent on the generation of PAF, a well-defined proinflammatory lipid that promotes neutrophil adhesion. Moreover, we have demonstrated that SCIP-dependent PAF formation is important for spatially controlling neutrophil adhesive behavior on the surface of thrombi. These findings extend the functional role of annexin 5A+ve platelets and suggest that the transition of intact spread platelets to SCIPs represents a potentially important mechanism of converting platelets from a proaggregatory to a proinflammatory state.
A major finding in the current study is the demonstration that the level of neutrophil adhesion and spreading under flow is indirectly influenced by nature of the thrombogenic substrate. Specifically, our studies have demonstrated that the localized adhesion and spreading of neutrophils on the surface of thrombi is tightly linked to increased matrix reactivity, through a process dependent on the conversion of spread platelets to annexin 5A–positive forms. It is noteworthy that others14,34 have also noted a poor spreading response of neutrophils on spread platelet monolayers under flow, a phenomenon that was thought to be due to the flow-based clearance of soluble chemokines. Based on the studies presented here, a more likely explanation is that these monolayers contained a small number of annexin 5A–positive platelets and as a result produced low levels of PAF. In this context, PAF and other lipid mediators can partition within the lipid membranes of platelets and endothelial cells, and this surface localization is considered a major component of the juxtacrine signaling mechanism, enabling efficient localized leukocyte adhesion in a shear field.14,35 Such a process is consistent with the ability of SCIPs to spatially regulate neutrophil adhesive behavior within a developing thrombus, and furthermore, by limiting adhesion to a subset of neutrophils may prevent excessive platelet-dependent neutrophil accumulation at sites of tissue injury.
The demonstration that SCIPs have enhanced adhesive function toward neutrophils was somewhat unexpected given their inability to support stable platelet-platelet adhesion.21 Moreover, given that SCIPs have a well-defined procoagulant function,21,22,36 our studies suggest that SCIP conversion represents a fundamental switch in platelet biology. We have previously suggested that SCIP conversion may serve partly to limit excessive platelet accumulation on potent thrombogenic matrices, particularly type I and III fibrillar collagens.21 However, given the potential importance of SCIPs in promoting thrombin generation, fibrin formation, and neutrophil adhesion and spreading, it is possible that these platelet subtypes also play an important role in host defense and vascular repair mechanisms. Notably, platelets with an ultrastructure consistent with SCIPs have previously been demonstrated at sites of vascular injury in close proximity to exposed collagen fibers in vivo.37–43 Given that collagens are located deep within the damaged arterial wall and are enriched in advanced atherosclerotic lesions, SCIP formation may represent a potentially important mechanism of enhancing leukocyte recruitment to sites of vascular injury. Moreover, there is increasing evidence that platelet-neutrophil interactions are important for the pathogenesis of deleterious conditions such as ischemia/reperfusion injury,44 respiratory distress syndrome,45 and septic shock.46,47 It thus will also be important to examine a role for conversion of platelets to SCIPs in pathological sequelae involving the neutrophil inflammatory response.
PAF has a well-defined role in promoting the P-selectin–dependent adhesion of neutrophils onto the surface of spread platelet monolayers.14,15 A similar role for PAF in promoting firm adhesion of neutrophils onto the surface of endothelial cells has also been well established,35,48 and a wealth of in vivo evidence has suggested a critical role for the PAF signaling system as a key regulator of neutrophil and platelet activation in a variety of inflammatory and thrombotic syndromes.1,2,49 In this context, it was surprising that PAF was not required for firm adhesion of neutrophils on platelet monolayers and had only a partial role in promoting neutrophil arrest on the surface of collagen- and VWF-formed thrombi. The differences between platelet monolayers and formed thrombi are likely to reflect specific differences in the extent of platelet activation rather than an inherent difference between primary adherent platelets and aggregated platelets. For example, under experimental conditions favoring maximal platelet stimulation, that is, prolonged exposure of collagen-formed thrombi to extracellular calcium or stimulation of spread monolayers with ionophore A23187, the PAF receptor antagonist had a less marked effect on firm neutrophil adhesion on either surface. However, under less potent activating conditions, such as those leading to 20% to 30% SCIP conversion on a VWF matrix, PAF appears to play a more prominent role in promoting neutrophil arrest. Presumably the platelet monolayers prepared in previous studies had a similar surface reactivity to those formed here on a VWF or collagen matrix, with a predominance of intact spread platelets over SCIPs.14,15 However, it is difficult to accurately predict the level of SCIP conversion in these previous studies, as many factors can influence the efficiency of this process (unpublished observations, S.K., March 2005). Nonetheless, our studies indicate that the relative importance of platelet PAF in regulating leukocyte adhesion is influenced by the overall surface reactivity of immobilized platelets. Furthermore, they suggest that the relative proportion of spread platelet to SCIPs may be important in determining the absolute requirement for certain chemokines, such as PAF, in regulating leukocyte adhesive function.
The demonstration of PAF-dependent and -independent pathways regulating firm neutrophil adhesion to platelets has previously been established14,15 although the identity of other chemokines contributing to this process remains unclear. Some of these chemokines are likely to be produced from spreading platelets as spread platelets can support efficient neutrophil arrest independent of SCIP formation and generated PAF. Thus far, of the platelet chemokines demonstrated to promote neutrophil adhesion, only NAP-2 has been shown to significantly increase following platelet stimulation with physiological agonists; however as demonstrated here, blockade of NAP-2 receptors on neutrophils appears to have minimal effects on neutrophil adhesion or spreading under flow. It remains possible that other unrecognized platelet chemokines play an important role in promoting neutrophil arrest, or alternatively, that a combination of chemokines is involved in this process with the inhibition of any one chemokine having only a minor impact on the ability of neutrophils to adhere and spread. Future studies will be required to address these issues.
The online version of this article contains a data supplement.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 USC section 1734.
Acknowledgments
This work was supported by grants from the National Health and Medical Research Council, The National Heart Foundation, and BBSRC. S.T. was a British Heart Foundation Travelling Fellow visiting the ACBD during the generation of this work.
We would like to thank Dr Varuni Kanagasundaram, Dr Warwick Nesbitt, Prof Hatem Salem, Dr Len Stephens, and Dr Phill Hawkins for helpful discussions and advice. We also thank Dr Nick Ktistakis and Maria Manifava for their help with lipid extraction and TLC experiments and Judith Webster for her help with the LCMS work.
Authorship
Contribution: S.K. designed and performed research, collected and analyzed data, and wrote the paper; K.J.W. designed and performed research, and collected and analyzed data; S.T. performed research, and collected and analyzed data; D.O. performed research; and S.P.J. designed research and wrote the paper.
S.K. and K.J.W. contributed equally to this work.
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Correspondence: Shaun P. Jackson, Australian Centre for Blood Diseases, Monash University, The Alfred Medical Research & Education Precinct, 6th Floor Burnet Tower, 23-87 Commercial Road, Prahran, Victoria–3181, Australia; e-mail: shaun.jackson@med.monash.edu.au.


This feature is available to Subscribers Only
Sign In or Create an Account Close Modal