T cell–based therapies have much promise in cancer treatment. This approach may be enhanced if used in combination with radiotherapy provided that tumor-specific T cells can be protected against the effects of radiotherapy. Previously, we demonstrated that administration of TLR9 ligand into mice decreased activation- and serum deprivation–induced cell death in T cells. We hypothesized that TLR9 engagement on T lymphocytes decreased apoptosis after cellular stress. We show that TLR9 engagement on murine CD4 T cells reduces γ-radiation–induced apoptosis as judged by decreased annexin-V/PI staining, caspase-3 activation, and PARP cleavage. TLR9-stimulated cells show heightened accumulation at the G2 cell-cycle phase and increased DNA repair rates. Irradiated, TLR9-engaged cells showed higher levels of phosphorylated Chk1 and Chk2. While the levels of activated ATM in response to IR did not differ between TLR9-stimulated and unstimulated cells, inhibition of ATM/ATR and Chk1/Chk2 kinases abolished the radioprotective effects in TLR9-stimulated cells. In vivo, TLR9-stimulated cells displayed higher radio resistance than TLR9-stimulated MyD88–/– T cells and responded to antigenic stimulation after total body irradiation. These findings show, for the first time, that TLR9 engagement on CD4 T cells reduces IR-induced apoptosis by influencing cell-cycle checkpoint activity, potentially allowing for combinatorial immunotherapy and radiotherapy.
Introduction
The development of T cell–based immunotherapy to treat cancer patients has advanced significantly in the last decade due to the identification of multiple tumor antigens and the understanding of the signals that stimulate antitumor T-cell responses.1 For example, vaccine-based strategies that incorporate tumor antigens (in the form of proteins or peptides) to elicit strong CD4 and CD8 T-cell responses are effective in both the prevention and the treatment of various cancers in preclinical studies.2,–4 In cancer patients, infusion of in vitro–activated and expanded tumor-specific T cells has been shown to reduce tumor burden in patients with various types of malignancies.5 Unfortunately, although T-cell responses are effective against small tumor loads, they are generally ineffective against bulky tumors.5 One promising strategy is to combine immunotherapy with current anticancer treatments to enhance the antitumor effects
Ionizing radiotherapy (RT) is an important therapy for the treatment of tumors.6 Generally, RT is administered locally to the tumor site or draining lymph nodes and kills cancer cells by damaging DNA. Radiotherapy is effective at reducing large burdens in some cancers and preventing local recurrence in the case of positive margins. However, RT is rarely curative as a single treatment modality and is therefore often combined with chemotherapy. Unfortunately, this combination results in the destruction of nonmalignant cells including immune cells, which are especially sensitive to radiation.7,8 Recent reports suggest that RT and immunotherapy might have a synergistic or at least an additive effect against tumors when given sequentially.9,,,–13 There might also be an advantage of giving the treatments at the same time, provided that tumor-specific T cells can be protected against the effects of RT.14
The use of toll-like receptor (TLR) agonists as immune adjuvants to improve antitumor T-cell responses has been a subject of intense focus in recent times. Current studies reveal that local injections of TLR agonists can be combined with RT to enhance antitumor T-cell responses; however, these mechanisms remain undefined.9,,,–13 TLRs are expressed primarily on innate immune cells and activate the immune system by recognizing a range of microbial products, including lipopolysaccharide (TLR4), peptidoglycans and lipopeptides (TLR1 and TLR2), flagellin (TLR5), RNA (TLR3, TLR7, TLR8), and unmethylated “CpG”-DNA (TLR9).15,16 Stimulation of TLRs has been shown to enhance T-cell responses through the production of proinflammatory cytokines and the increased expression of costimulatory molecules on antigen presenting cells.15 Additionally, TLR9 stimulation enhances the intensity of the immune response by prolonging cell survival through the up-regulation of antiapoptotic molecules.15,17,,–20 Consequently, it is not surprising that the stimulation of TLR9 has also been shown to repress apoptosis in innate immune cells against a variety of stimuli including ionizing radiation (IR).18,,,,,–24 Although much attention has focused on the effects of TLR stimulation on innate immune cells, TLRs are also expressed on cells of the adaptive immune system.
TLRs are expressed and functional on human and mouse T lymphocytes. For instance, in vitro, the engagement of TLR1/2, -5, -7 and -9 on CD4 T helper cells enhances cytokine production and proliferation.25,,–28 The stimulation of TLR2 and TLR8 on CD4+CD25+ regulatory T cells blocks their suppressive effects.29,30 TLR1/2 engagement on CD8 T cells increases longevity, in vitro, by augmenting expression levels of antiapoptotic proteins.17,31,,–34 However, there are no reports demonstrating the potential effects of direct TLR stimulation on T cells in vivo. Previously, we showed that injection of the TLR9 ligand into mice increased the numbers of CD4 and CD8 T cells and that T cells from these mice were more resistant against serum deprivation– and activation–induced cell death ex vivo.17 However, it was not clear whether the protective effects of the TLR9 ligand were the result of direct TLR9 stimulation on T cells or through the stimulation of innate immune cells such as dendritic cells (DCs). Furthermore, it was unknown whether T lymphocytes from TLR9 ligand–treated mice were resistant to other cytotoxic stimuli such as γ-radiation.
In this study, we tested the effects of TLR9 engagement on CD4 T lymphocytes. The data show that TLR9 stimulation decreased IR-induced apoptosis. In addition, TLR9-stimulated cells displayed a more robust activation of the G2 cell-cycle checkpoint and increased rates of DNA repair after IR. TLR9-stimulated T cells also display elevated levels of the phosphorylation of Chk1 and Chk2 in response to irradiation. The activity of these and the ataxia telangiectasia mutated (ATM)/ATM-related (ATR) kinases is required to induce the radioprotective effect activated by TLR9 engagement. In vivo, the administration of TLR9 agonist preferentially protected wild-type T cells, over TLR9 signaling–impaired T cells, after nonmyeloablative doses of total body irradiation (TBI). TLR9-stimulated, irradiated CD4 T cells retained their capacity to respond to antigenic stimulation in vivo. These findings indicate that TLR9 engagement on CD4 T cells protect against radiation and would be especially valuable in developing novel combination therapies that will enhance and preserve antitumor T-cell responses in cancer patients undergoing radiotherapy.
Methods
Animal studies conducted in this work were approved by the Louisiana State University Health Sciences Center Institutional Animal Care and Use Committee.
T-cell isolation, treatment, and irradiation
Mouse CD4 T cells were enriched by negative selection (Stemcell Technology, Vancouver, BC) followed by positive selection (Miltenyi Biotec, Auburn, CA); purity > 99.5%. T cells (106) were cultured in 24-well plates in the presence of plate-bound α-CD3 antibody (2.5 μg/mL) and α-CD28 (1.0 μg/mL) for 48 hours, removed, and cultured in the presence of the TLR9 ligand CpG-ODN-1826 (TCCATGACGTTCCTGACGTT; 10 μg/mL) or control nonstimulatory ligand for an additional 24 hours. TLR9 ligand was synthesized without a phosphorothioate backbone followed by removal of endotoxins using a Detoxi-Gel Removal kit (Pierce, Rockford, IL); Mayo Clinic, DNA Core Facility, Rochester, MN. Twenty-four hours after addition of TLR9-ligand T lymphocytes were irradiated using a Gammacell 40 Exactor; MDS Nordion (Ottawa, ON) 60Co-γ. In some experiments cells were treated with pharmacologic inhibitors for Chk1 and Chk2 proteins debromohymenialdisine (DBH; 4 μM; Calbiochem, La Jolla, CA), UCN01 (100 μM), and wortmannin (10 μM; Sigma-Aldrich, St Louis, MO).
Western Blots
Fifty micrograms cell extract was prepared from purified CD4 T cells and conducted as previously described.17 Briefly, after washing the membranes were incubated overnight at 4°C with antibodies to Bcl-xL, Bcl-2, phosphorylated p-(Ser1981)-ATM, p-(Ser345)-Chk1, p-(Thr387)-Chk2, Chk2, Poly (ADP-ribose) polymerase (PARP), caspase-3 (1:1000, all from Cell Signaling, Danvers, MA), total ATM (1:500; Santa Cruz Biotech, Santa Cruz, CA), Chk1 (2μg/mL;AbCam), and β-actin (1:5000;AbCam), stained with horseradish peroxidase-conjugated secondary Abs (1:5000), and developed with the ECL Plus (GE-Healthcare, Chalfont St Giles, United Kingdom).
Flow cytometry
Apoptosis was quantitated by flow cytometry by staining cells with FITC-labeled annexin-V (BD Pharmingen, San Jose, CA) and propidium iodide (PI; Sigma-Aldrich). In some experiments, cellular DNA content was determined by permeablizing cells in 70% ethanol for 2 hours at 4°C followed by staining with PI for 30 minutes at room temperature and analyzed on a FACScalibur (BD Biosciences, San Jose, CA). In adoptive T-cell transfer experiments, the number of CD4 T cells was determined by flow cytometry using fluorescent-labeled mAbs specific for the indicated cell populations. Briefly, 106 cells were stained with mAb for 45 minutes at 4°C in 200 μL phosphate-buffered saline (PBS) containing 0.1% sodium azide and 2% fetal calf serum (FCS). Cells were washed and analyzed for CD4, CD45.1, CD45.2 CD90.1 (BD Pharmingen) expression on a FACScalibur. In other experiments, T-cell proliferation was evaluated by labeling cells with 1 μM CarboxyFluoroscein Succinimidyl Ester (CFSE) and analyzed by flow cytometry.
Comet assay
Comet assay was used to detect IR-induced double strand breaks (DSBs) under neutral pH conditions as recommended by the manufacturer (Trevigen, Gaithersburg, MD). Briefly, cells were cast into agarose gels on microscope slides, lysed to remove DNA-associated proteins before electrophoresis. DNA damage was evaluated on an Automated Comet Assay Scoring System (Loats Associates, Westminister, MD) by analyzing 150 > cells (2 fields per time point).
Mice and treatments
We used C57BL6 mice (Charles River Laboratories, Wilmington, MA), B6.SJL-PtprcaPep3/BoyJ and B6.Pl-Thy1a/Cy (Jackson Laboratory, Bar Harbor, ME), MyD88–/– mice (a kind gift from Dr Douglas Golenbock, Boston University), and TLR9–/– splenocytes (a kind gift from Dr Jeffrey Platt, Mayo Clinic, Rochester, MN). All experiments were routinely performed in groups of 3 to 5 mice each. Mice were injected with 50 μg TLR9 ligand or control ligand via intraperitoneal injections on days 1, 3, and 5 followed by 300 cGy total body irradiation in a Gammacell 40 Exactor (MDS Nordion) 60Co-γ on day 7. Spleens and lymph nodes were obtained at the indicated time points after irradiation. The numbers of cells recovered per mouse were determined using flow cytometry (LSRII; Becton Dickinson, Franklin Lakes, NJ). The absolute count for each cell type/subset was estimated by multiplying the percentage of the corresponding cell subset by the number of splenocytes recovered per mouse.
Adaptive T-cell transfers
CD4 T cells were purified from the pooled spleens and lymph nodes of CD90.1 and CD45.1 as described. Purified T cells were mixed at a 1:1 ratio, and 4 × 106 cells were intravenously injected into mice. In some experiments purified T cells from CD45.1 and MyD88–/– or CD45.1 OT-2 T cell receptor (TCR) transgenic were intravenously injected into mice.
Results
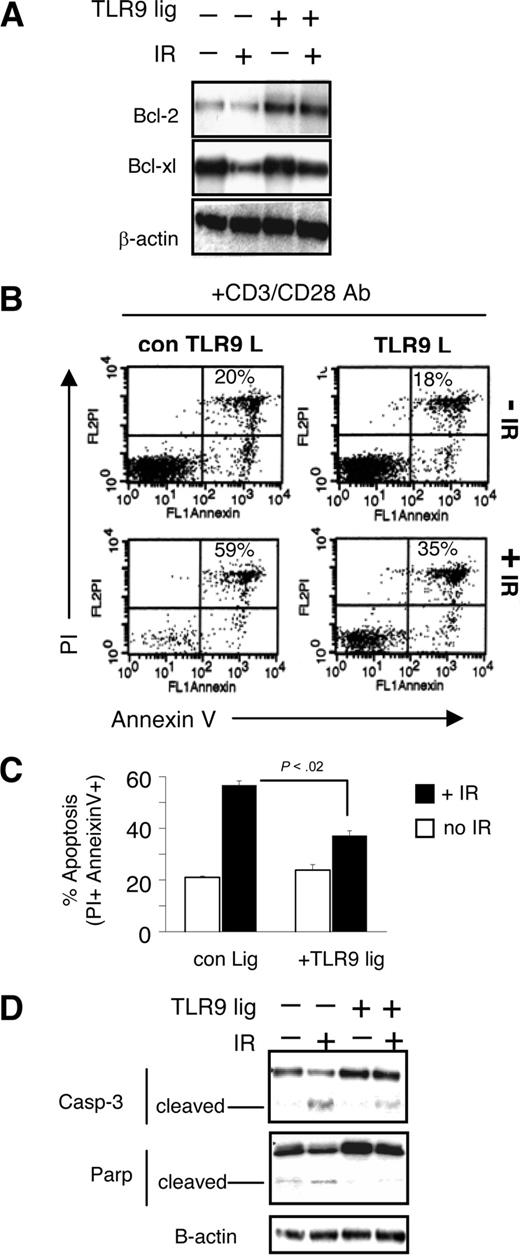
TLR9 engagement on CD4 T cells represses IR-induced apoptosis
TLR9 is expressed and functional on activated CD4 T cells34,35 ; hence, we chose this cell type as a model for study (Figure S1, available on the Blood website; see the Supplemental Materials link at the top of the online article). We hypothesized that TLR9 engagement on CD4 T cells results in the enhanced expression of proteins with antiapoptotic properties and that this imparts a radioprotective feature to T cells. We examined expression of the antiapoptotic proteins Bcl-2 and Bcl-xl in TLR9 ligand–treated cells and nontreated cells either unirradiated or exposed to γ-radiation (300 cGy). Purified CD4 T cells were first activated with plate-bound anti-CD3/28 antibodies for 48 hours and transferred to new media containing TLR9 ligand (10 μg/mL) or control TLR9 ligand. Twenty-four hours later cells were exposed to 300 cGy. We observed higher levels of Bcl-2 in CD4 T cells incubated with TLR9 ligand in both irradiated and nonirradiated cells compared with control cells (Figure 1A). We did not observe an increase from baseline in Bcl-xL expression in either irradiated TLR9 ligand–treated or untreated CD4 cells. However, in irradiated CD4 T cells not treated with TLR9 ligand, Bcl-xL expression decreased faster than in TLR9-treated irradiated cells.
TLR9-stimulation on CD4 T lymphocytes represses IR-induced apoptosis. (A) CD4 T cells were purified by negative selection and then followed by positive selection using magnetic beads. 106 cells were activated with plate-bound anti-CD3 and CD28 antibody for 48 hours. After this time, cells were cultured in fresh media in the absence or presence of TLR9 ligand (10 μg/mL CpG-ODN) for 24 hours, as described in “Methods.” After activation, cells were irradiated (300 cGy γ-radiation) and parked in culture for an additional 24 hours. Cells were then harvested and total cell lysates were used for analysis by Western blot for the expression of indicated proteins. (B,C) Alternatively, 24 hours after irradiation apoptosis was evaluated by staining cells with annexin-V plus propidium iodide and the average of several experiments is shown in panel C. The percentages indicated on the graph are the percent of double positive PI- and annexin V–stained cells (± SD, n = 3 experiments). P values were determined by use of Student t test; P < .02. (D) CD4 T cells were treated as described in panel A. Twenty-four hours after irradiation cell lysates were used to analyze the expression of the indicated proteins by Western blots.
TLR9-stimulation on CD4 T lymphocytes represses IR-induced apoptosis. (A) CD4 T cells were purified by negative selection and then followed by positive selection using magnetic beads. 106 cells were activated with plate-bound anti-CD3 and CD28 antibody for 48 hours. After this time, cells were cultured in fresh media in the absence or presence of TLR9 ligand (10 μg/mL CpG-ODN) for 24 hours, as described in “Methods.” After activation, cells were irradiated (300 cGy γ-radiation) and parked in culture for an additional 24 hours. Cells were then harvested and total cell lysates were used for analysis by Western blot for the expression of indicated proteins. (B,C) Alternatively, 24 hours after irradiation apoptosis was evaluated by staining cells with annexin-V plus propidium iodide and the average of several experiments is shown in panel C. The percentages indicated on the graph are the percent of double positive PI- and annexin V–stained cells (± SD, n = 3 experiments). P values were determined by use of Student t test; P < .02. (D) CD4 T cells were treated as described in panel A. Twenty-four hours after irradiation cell lysates were used to analyze the expression of the indicated proteins by Western blots.
We next examined apoptosis in TLR9-stimulated and nonstimulated CD4 T cells in response to IR by evaluating the percentage of propidium iodide and annexin-V–stained cells. Twenty-four hours after IR, we observed a significant increase (from 20% to 59%) in apoptotic CD4 T cells compared with unirradiated controls (Figure 1B representative dot plot). In TLR9-stimulated CD4 T cells, we also observed apoptotic cells (from 18% to 35%) in response to IR, but the percentages were significantly lower than cells treated with control ligand (P < .02, n = 3; Figure 1C; data from several experiments).
We conducted Western blot analysis using antibodies specific for caspase-3 and PARP as an independent biochemical assay to confirm that cells are triggering apoptosis. Active caspase-3, which normally exists as an inactive 32-kD zymogenic form, is cleaved to yield catalytically active subunits,36 was observed in both TLR9-stimulated and unstimulated cells in response to irradiation (Figure 1D); however, we observed significantly lower levels of active caspase-3 in TLR9-stimulated cells. We also observed enhanced accumulation of cleaved PARP, which is targeted for caspase-dependent proteolysis,37 in non–TLR9-stimulated CD4 T cells, after IR (Figure 1D). In contrast, notably less IR-induced PARP cleavage was observed in TLR9-stimulated CD4 T cells. These results are consistent with the reduced level of apoptosis in these cells as measured by annexin/PI staining. When taken together, these findings indicate that TLR9 engagement result in a reduction of apoptosis in response to IR.
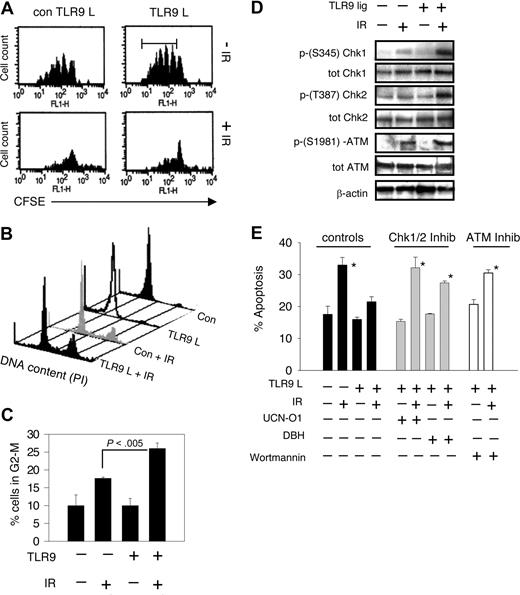
TLR9-stimulated T cells show enhanced cell-cycle checkpoint activation after IR
Cells exposed to irradiation activate cell-cycle checkpoint, resulting in a halt of cell proliferation. To fully characterize irradiation response in TLR9-engaged CD4 T cells, we evaluated T-cell proliferation, with or without TLR9 stimulation, in irradiated and nonirradiated cells. CD4 T cells were labeled with CFSE, and activated as described. Unirradiated, CFSE-labeled CD4 T cells showed marked proliferation (Figure 2A). Additionally, consistent with the finding of others,34 we did not observe an effect of TLR9 stimulation on cell proliferation. In response to irradiation, however, we observed that both untreated and TLR9-engaged cells showed a clear decrease in proliferation, indicating that T cells were undergoing cell-cycle arrest.
TLR9 engagement plus γ-radiation enhances cell-cycle checkpoint activation. (A) CD4 T cells were labeled with CFSE (1 μM), activated with plate-bound anti-CD3 and CD28 antibodies for 48 hours. Cells were removed and placed in fresh media containing TLR9 or control ligand (10 μg/mL) for 24 hours followed by IR (300 cGy γ-radiation). Cells were maintained in the presence of IL-2 (50 U/mL) for an additional 3 days. Seventy-two hours after IR, T-cell division was evaluated by flow cytometry. Each CFSE peak, after the first peak, represents one cycle of cell division. (B) CD4 T cells were activated with plate-bound anti-CD3 and CD28 antibodies for 48 hours. Cells were removed and placed in fresh media containing TLR9 or control ligand (10 μg/mL) for 24 hours followed by IR (300 cGy γ-radiation). Twenty-four hours after IR, cells were harvested, stained with propidium iodide, and analyzed by flow cytometry. The data in the histogram in panel B show the DNA content of cells from different groups. The percentage of cells in the G-2M phase, compiled from several experiments (± SD) is shown in panel C. P values were determined by use of Student t test; P < .005. (D) CD4 T lymphocytes were treated as described in panel C except that protein was collected from TLR-stimulated or nonstimulated cells plus or minus IR 20 minutes after IR. Western blot was used to analyze the indicated proteins. (E) CD4 T lymphocytes were treated as described in Figure 1. Before IR exposure, UCN-01 or DBH, which inhibit Chk1 and Chk2 activation, or wortmannin, which inactivates PI3K activity, were added to cell cultures. The levels of apoptotic cells as determined by annexin V and propidium iodide staining were evaluated 24 hours after IR and were measured by flow cytometry. The data shown is representative of at least 2 experiments (± SD), each showing identical results. The Student t test was used to determine P values between the indicated groups and irradiated, TLR9-treated cells; *P < .05.
TLR9 engagement plus γ-radiation enhances cell-cycle checkpoint activation. (A) CD4 T cells were labeled with CFSE (1 μM), activated with plate-bound anti-CD3 and CD28 antibodies for 48 hours. Cells were removed and placed in fresh media containing TLR9 or control ligand (10 μg/mL) for 24 hours followed by IR (300 cGy γ-radiation). Cells were maintained in the presence of IL-2 (50 U/mL) for an additional 3 days. Seventy-two hours after IR, T-cell division was evaluated by flow cytometry. Each CFSE peak, after the first peak, represents one cycle of cell division. (B) CD4 T cells were activated with plate-bound anti-CD3 and CD28 antibodies for 48 hours. Cells were removed and placed in fresh media containing TLR9 or control ligand (10 μg/mL) for 24 hours followed by IR (300 cGy γ-radiation). Twenty-four hours after IR, cells were harvested, stained with propidium iodide, and analyzed by flow cytometry. The data in the histogram in panel B show the DNA content of cells from different groups. The percentage of cells in the G-2M phase, compiled from several experiments (± SD) is shown in panel C. P values were determined by use of Student t test; P < .005. (D) CD4 T lymphocytes were treated as described in panel C except that protein was collected from TLR-stimulated or nonstimulated cells plus or minus IR 20 minutes after IR. Western blot was used to analyze the indicated proteins. (E) CD4 T lymphocytes were treated as described in Figure 1. Before IR exposure, UCN-01 or DBH, which inhibit Chk1 and Chk2 activation, or wortmannin, which inactivates PI3K activity, were added to cell cultures. The levels of apoptotic cells as determined by annexin V and propidium iodide staining were evaluated 24 hours after IR and were measured by flow cytometry. The data shown is representative of at least 2 experiments (± SD), each showing identical results. The Student t test was used to determine P values between the indicated groups and irradiated, TLR9-treated cells; *P < .05.
We next analyzed DNA content in TLR9-treated CD4 T cells by flow cytometry. Consistent with activation of the G2/M checkpoint in response to IR, we observed a clear increase in cells with 4N DNA content 24 hours after irradiation compared with unirradiated controls (Figure 2B). Moreover, the percentage of cells containing a 4N DNA content after irradiation show a statistically significant increase in response to TLR9 stimulation compared with irradiated non–TLR9-stimulated cells (P < .005, n = 3; Figure 2C). This analysis indicates that TLR9 engagement enhances the G2/M checkpoint response after IR.
To further understand the enhanced cell-cycle checkpoint response mediated by TLR9 engagement in CD4 T cells, we examined several biochemical events linked to activation of the G2/M checkpoint in TLR9-stimulated and nonstimulated T cells. Specifically, we looked at the activation of kinases Chk1, Chk2, and ATM as these molecules are connected to this response.38 While the overall level of Chk1 was uneffected by TLR9 engagement or irradiation, we observed that phosphorylation of the Ser345 residue, a posttranslational modification linked to the catalytic activation of Chk1, was enhanced in irradiated T cells stimulated with TLR9 ligand as compared with irradiated T cells treated with control ligand (Figure 2D). Similarly, we found no difference in total Chk2 expression in response to TLR9 stimulation, but observed an increase in Thr387 phosphorylation,39 indicative of the catalytic activation of this kinase, in irradiated TLR9 ligand–treated cells compared with controls.
Chk1 and Chk2 are phosphorylated (activated) by the kinases ATR and ATM, respectively, in response to DNA damage.40,41 We tested for phosphorylated ATM (Ser1981-phosphorylated)42 in extracts of irradiated TLR9 ligand–treated and control ligand–treated CD4 T cells by Western blot analysis. This experiment showed, as predicted, that the phosphorylated form of ATM was detectable in extracts from irradiated cells (Figure 2D); however, similar signal intensities were observed in extracts from TLR9 ligand– and control ligand–treated cells. This result suggests that the increase in Chk2 phosphorylation observed in TLR9-treated cells is not attributable to increased ATM activity.
We next used 2 pharmacologic inhibitors of Chk1 and Chk2 catalytic activity, DBH43,44 and 7-hydroxystaurosporine (UCN-01),45,46 to examine the role that these kinases play during IR response in CD4 T cells. Specifically, these drugs were used to measure the effect that Chk1/2 inhibition has on irradiation-induced apoptosis. As we previously observed, IR activates apoptosis in CD4 T cells and this response is suppressed with the addition of TLR9 ligand (Figure 2E). This decreased apoptotic response was abrogated when TLR9-stimulated CD4 T cells were treated with DBH or UCN-01 (Figure 2E). This finding indicates that inhibition of Chk1 and Chk2 overrides the radioprotective effect of TLR9 engagement in CD4 T cells. Several studies have determined that the radiosensitizing agent wortmannin inhibits ATM/ATR and related protein kinases.47,48 The antiapoptotic effects of TLR9-engagement were also lost after wortmannin treatment. Thus, although we did not observe an increase in the levels of activated ATM, these data are consistent with ATM/ATR activation playing a critical role in TLR9-mediated radioprotection. In addition, the enhanced levels of apoptosis in CD4 T cells treated with DBH, UCN-01, or wortmannin correlated with the decreased expression levels of the antiapoptotic protein bcl-2 in TLR9-stimulated cells (Figure S2).
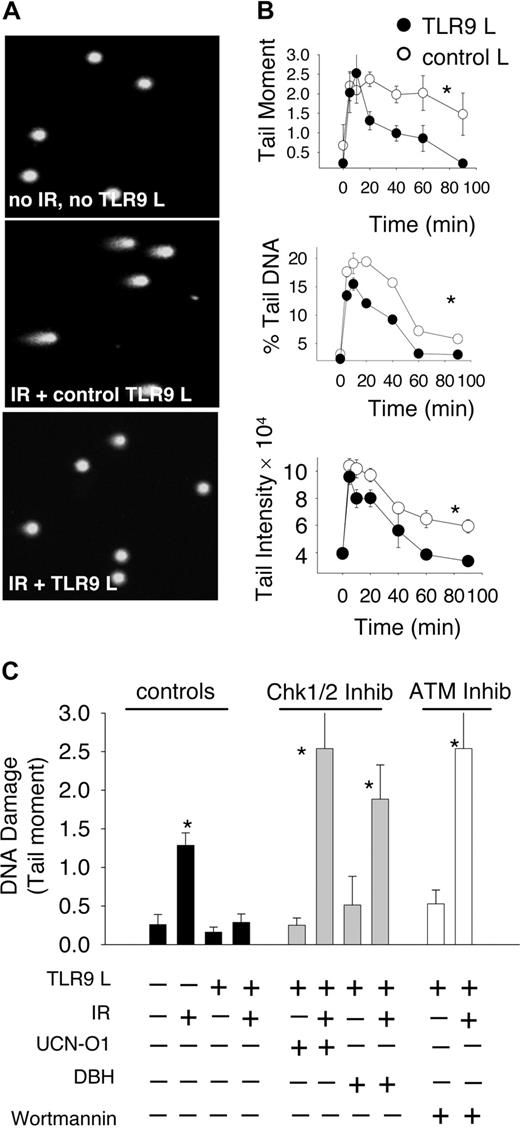
TLR9-stimulated CD4 T cells enhance DNA DSB repair activity
Ionizing radiation induces a wide range of damage into DNA including base and phosphodiester backbone oxidation often resulting in single and DSBs. Because efficient repair of DSBs is necessary to overcome the lethal effects of this type of genotoxic stress, we compared the levels of DNA damage after exposure to IR in TLR9-stimulated and nonstimulated CD4 T cells using a neutral pH comet assay that specifically detects DSB.49 Representative images of nonirradiated cells and TLR9-stimulated and unstimulated cells 30 minutes after IR are shown in Figure 3A. This analysis clearly demonstrated the presence of characteristic comet tails indicative of DSBs in irradiated CD4 T cells. The extent of DNA damage in TLR9-stimulated and nonstimulated cells was quantified as the percent tail DNA, tail moment, and tail intensity during the indicated time course after IR (Figure 3B). TLR9-stimulated and control T cells were equally susceptible to IR-induced DNA damage immediately after IR; however, the levels of damage were significantly decreased in TLR9-stimulated cells within 20 minutes after IR (P < .005 for all 3 parameters pertinent for DNA damage; Figure 3B). Additionally, the enhanced rate of DSB disappearance continued over the evaluated time course. In contrast, control ligand–treated cells showed a much slower rate of DNA repair, and cells with higher levels of DNA damage were observed at the end of this time course experiment (after 90 minutes; Figure 3B). These findings suggest that TLR9 engagement on CD4 T cells significantly enhances their capacity to repair IR-induced DSB.
TLR9-engaged CD4 T cells show increased DNA repair activity. (A) CD4 T lymphocytes were treated as described in Figure 1. Briefly, after activation and TLR9 ligand treatment CD4 T cells were irradiated or not. Comet analysis was conducted 30 minutes after irradiation. Representative images of DNA comet formation 30 minutes after irradiation are shown. (B) The levels of IR-induced DSB DNA damage (using neutral pH conditions that specifically detect DSB), at the indicated time points after IR are shown as tail moment, percent tail DNA, and tail intensity. Data are the means (± SD, n > 150 cells per condition). (C) Thirty minutes after IR the levels of DSBs were measured using the comet assay in cells treated with Chk1 and Chk2 inhibitors, UCN-01, DBH, or inhibitors of ATM, ATR and related protein kinases, wortmannin. The data shown are representative of at least 2 experiments, each showing identical results. P values for all 3 graphs in panel B were determined by use of 2-way analysis of variance using data acquired between 20 and 90 minutes after IR; *P < .05. Groups with asterisks represent groups that reached statistical differences as compared with irradiated, TLR9-stimulated cells.
TLR9-engaged CD4 T cells show increased DNA repair activity. (A) CD4 T lymphocytes were treated as described in Figure 1. Briefly, after activation and TLR9 ligand treatment CD4 T cells were irradiated or not. Comet analysis was conducted 30 minutes after irradiation. Representative images of DNA comet formation 30 minutes after irradiation are shown. (B) The levels of IR-induced DSB DNA damage (using neutral pH conditions that specifically detect DSB), at the indicated time points after IR are shown as tail moment, percent tail DNA, and tail intensity. Data are the means (± SD, n > 150 cells per condition). (C) Thirty minutes after IR the levels of DSBs were measured using the comet assay in cells treated with Chk1 and Chk2 inhibitors, UCN-01, DBH, or inhibitors of ATM, ATR and related protein kinases, wortmannin. The data shown are representative of at least 2 experiments, each showing identical results. P values for all 3 graphs in panel B were determined by use of 2-way analysis of variance using data acquired between 20 and 90 minutes after IR; *P < .05. Groups with asterisks represent groups that reached statistical differences as compared with irradiated, TLR9-stimulated cells.
We next examined a potential role for the Chk1/2 and ATM/ATR kinases in augmenting the rate of DSB repair in irradiated, TLR9-stimulated CD4 T cells. We observed that TLR9 engagement led to a reduction in DSBs as measured by tail moment (Figure 3C). Treatment of irradiated CD4 T cells with TLR9 ligand and either DBH or UCN-01 abrogated the enhanced rates of DSB repair in these cells (Figure 3C). We also observed that the ATM/ATR inhibitor wortmannin similarly blocked the enhanced DSB repair shown by TLR9-engaged cells. Taken together, these findings suggest that Chk1/2 and ATM/ATR are critical in facilitating the enhanced rates of DNA repair exhibited by TLR9-stimulated CD4 T cells.
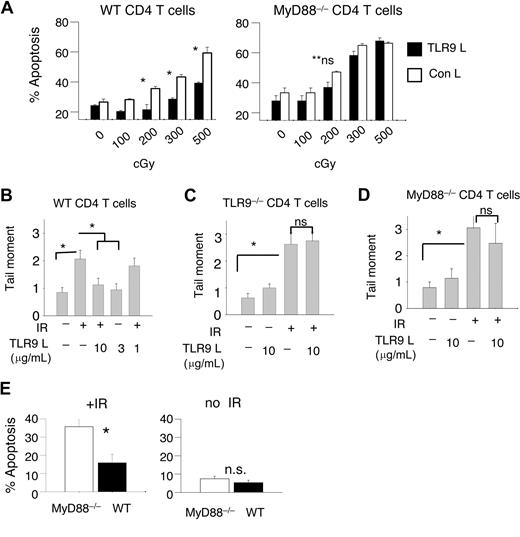
TLR9 stimulation lowers sensitivity to IR-induced apoptosis via the TLR9-MyD88 signaling transduction pathway
We next confirmed that the decreased apoptosis and enhanced DNA repair activity induced by TLR9 stimulation occurred via the TLR9-MyD88 signaling pathway and not as the result of nonspecific affects by the TLR9 ligand. MyD88–/– and wild type (WT) CD4 T cells were activated and treated or not with the TLR9 ligand followed by IR. The survival of TLR9-stimulated and nonstimulated WT and MyD88–/– CD4 T cells was compared after exposure to varying IR doses. The engagement of TLR9 on WT CD4 T cells significantly decreased the levels of IR-induced apoptosis compared with irradiated cells without TLR9 stimulation (P < .05, n = 3; Figure 4A). This effect was observed up to 500 cGy but was not observed after a dose of 800 cGy (data not shown). In contrast, TLR9 stimulation had no protective effect on IR-induced apoptosis in MyD88–/– CD4 T cells.
TLR9 engagement decreases sensitivity to IR-induced apoptosis via the TLR9-MyD88–signaling transduction pathway. (A) CD4 T cells from WT or MyD88–/– mice were activated and treated with TLR9 ligand or control ligand as described in Figure 1. Twenty-four hours after TLR9 treatment, T cells were irradiated using various doses of γ-radiation, and apoptosis was determined by flow cytometry. (B-D) CD4 T lymphocytes from WT, TLR9–/–, or MyD88–/– BL/6 mice were activated with plate-bound anti-CD3/CD28 Ab and treated or not with the indicated concentrations of TLR9 ligand before exposure to IR (300 cGy). Irradiated T cells were allowed 30 minutes to repair DNA before damage was measured using comet assay. Data shown are representative of several experiments, each showing similar trends; data are the means (± SD, n > 150 cells per condition). (E) CD4 T cells from CD45.1 mice were mixed at a 1:1 ratio with MyD88–/– CD4 T lymphocytes (which express CD45.2) and activated with plate-bound CD3/CD28 Ab and treated with TLR9 ligand as described. Twenty-four hours after TLR9 treatment, T cells were or were not irradiated (300 cGy) and the levels of apoptosis from each group were measured by flow cytometry 24 hours after irradiation. The Student t test was used to determine P values between the indicated groups; *P < .05; ns indicates not significant; data are the means (± SD).
TLR9 engagement decreases sensitivity to IR-induced apoptosis via the TLR9-MyD88–signaling transduction pathway. (A) CD4 T cells from WT or MyD88–/– mice were activated and treated with TLR9 ligand or control ligand as described in Figure 1. Twenty-four hours after TLR9 treatment, T cells were irradiated using various doses of γ-radiation, and apoptosis was determined by flow cytometry. (B-D) CD4 T lymphocytes from WT, TLR9–/–, or MyD88–/– BL/6 mice were activated with plate-bound anti-CD3/CD28 Ab and treated or not with the indicated concentrations of TLR9 ligand before exposure to IR (300 cGy). Irradiated T cells were allowed 30 minutes to repair DNA before damage was measured using comet assay. Data shown are representative of several experiments, each showing similar trends; data are the means (± SD, n > 150 cells per condition). (E) CD4 T cells from CD45.1 mice were mixed at a 1:1 ratio with MyD88–/– CD4 T lymphocytes (which express CD45.2) and activated with plate-bound CD3/CD28 Ab and treated with TLR9 ligand as described. Twenty-four hours after TLR9 treatment, T cells were or were not irradiated (300 cGy) and the levels of apoptosis from each group were measured by flow cytometry 24 hours after irradiation. The Student t test was used to determine P values between the indicated groups; *P < .05; ns indicates not significant; data are the means (± SD).
The levels of DNA damage and rates of repair in TLR9-stimulated, irradiated WT, MyD88–/–, and TLR9–/– CD4 T cells were evaluated. Consistent with our previous observation, TLR9-treated (10 μg/mL), irradiated WT T cells showed a reduced level of DNA damage 30 minutes after IR. Similarly, cells treated with 3 μg/mL TLR9 ligand showed reduced amounts of DNA damage at this time point; however, cells treated with 1 μg/mL per mL TLR9 ligand showed no enhanced rate of DNA repair compared with controls (Figure 4B).
When similar experiments were conducted in TLR9–/– (Figure 4C) and MyD88–/– CD4 T cells (Figure 4D) the addition of TLR9 ligand showed no clear enhancement of DNA repair 30 minutes after IR. These data clearly indicate that an intact TLR9-MyD88 signaling transduction pathway is required to confer cells the radioprotective effect in response to TLR9 ligand.
Next, to determine whether TLR9 stimulation induced the production of soluble factors (such as cytokines) that might confer radioresistance, CD45.1 WT and CD45.2 MyD88–/– CD4 T cells were cultured together at a 1:1 ratio, incubated with TLR9 ligand, and subsequently irradiated. (The CD45.1 and CD45.2 are congenic markers used to differentiate between the 2 different cell groups using flow cytometry.) We observed that the percentage of apoptotic WT CD4 T cells was significantly lower than MyD88–/– T cells (P < .05), demonstrating that TLR9-stimulation on WT T cells preferentially protected them over TLR9-signaling impaired cells (Figure 4E). In the absence of IR, the percentages of apoptotic CD4 MyD88–/– and WT cells remained similar (Figure 4E). These findings demonstrate that neither cytokines nor other factors produced in response to TLR stimulation play a major role in conferring radioresistance. However, these findings do not rule out the possibility that TLR-stimulated T cells increase the expression of certain receptors and thus might become more responsive to cytokine stimulation.
TLR9-stimulated CD4 T cells show preferential survival after irradiation
We next tested whether the in vivo administration of TLR9 ligand in mice protected T cells after total body irradiation (TBI). As depicted in Figure 5A, CD4 T cells were purified from TLR9 ligand–treated CD45.1 mice or control ligand–treated Thy1.1 (CD90.1) mice. (The CD90.1 and CD45.1 are congenic markers used to differentiate between the 2 different cell groups using flow cytometry.) T cells were mixed at a 1:1 ratio and intravenously injected into BL6 mice (CD90.2 CD45.2). Twenty-four hours after adoptive T-cell transfer, mice were injected with TLR9 ligand on days 1, 3, and 5. On day 6, mice were irradiated (300 cGy). After TBI, the numbers of CD90.1 T cells were nearly 6-fold lower than the number of CD90.1 T cells recovered from unirradiated mice (Figure 5B). In contrast, the number of CD45.1 T cells (+ TLR9 injections) in IR mice was 2-fold lower than that obtained from unirradiated mice (Figure 5B); indicating that T cells from TLR9-treated mice were more resistant to IR than control cells. To exclude the indirect effects of TLR9-stimulated antigen-presenting cell (APCs), CD4 T cells were stimulated with TLR9 ligand and anti-CD3/28 antibodies in vitro and then adoptively transferred to a WT host. TLR9-stimulated CD4 T cells show greater resistance to IR-induced apoptosis than non–TLR9-stimulated cells (Figure S3). Together, these results indicate that TLR9 engagement confers a radioprotective phenotype that protects T cells against the toxic effects IR in vivo.
CD4 T cells from TLR9 ligand–treated mice show a lower sensitivity to IR-induced apoptosis. (A) A schematic representation of the protocol used for the experiments described here. CD4 T cells were purified from CD45.1 BL/6 mice that were injected with TLR9 ligand (3 intraperitoneal injections of 50 μg/mL on days 1, 3, and 5) or from Thy1.1 (CD90.1) BL/6 mice injected with control ligand. T cells (4 × 106) were mixed at a 1:1 ratio and intravenously injected into congenic CD90.2 CD45.2 BL/6 mice (n = 3). Twenty-four hours after adaptive transfer, mice underwent TBI (300 cGy) or not. (B) Ten days after TBI, the numbers of CD45.1 and CD90.1 cells were determined by flow cytometry by staining spleen cell suspensions with antibodies to CD4, CD45.1, or CD90.1. Data shown are the means (± SD); P values were determined by use of the Student t test; *P < .05; There was not a significant difference in T-cell numbers in non-IR hosts (P > .1).
CD4 T cells from TLR9 ligand–treated mice show a lower sensitivity to IR-induced apoptosis. (A) A schematic representation of the protocol used for the experiments described here. CD4 T cells were purified from CD45.1 BL/6 mice that were injected with TLR9 ligand (3 intraperitoneal injections of 50 μg/mL on days 1, 3, and 5) or from Thy1.1 (CD90.1) BL/6 mice injected with control ligand. T cells (4 × 106) were mixed at a 1:1 ratio and intravenously injected into congenic CD90.2 CD45.2 BL/6 mice (n = 3). Twenty-four hours after adaptive transfer, mice underwent TBI (300 cGy) or not. (B) Ten days after TBI, the numbers of CD45.1 and CD90.1 cells were determined by flow cytometry by staining spleen cell suspensions with antibodies to CD4, CD45.1, or CD90.1. Data shown are the means (± SD); P values were determined by use of the Student t test; *P < .05; There was not a significant difference in T-cell numbers in non-IR hosts (P > .1).
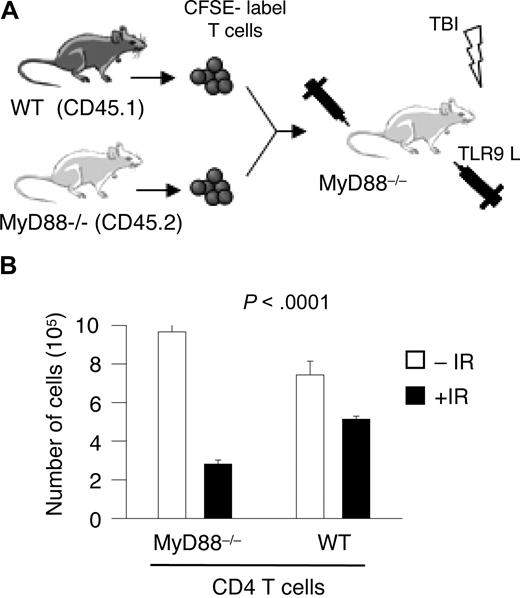
One possible interpretation of the results of these in vivo experiments is that the radioprotective effect of TLR9 ligand could stem from direct TLR9 stimulation on T cells. Alternatively, the radioprotective effect could be mediated through other TLR9-expressing cells such as DCs. To verify the preferential survival of TLR9-stimulated T cells over nonstimulated cells after TBI, T cells were purified from CD45.1 WT mice and CD45.2 MyD88–/– mice and activated with plate-bound anti-CD3/28 antibodies (Figure 6A). Forty-eight hours after in vitro activation, cells were mixed at a 1:1 ratio, labeled with CFSE, and intravenously injected into MyD88–/– mice. MyD88–/– mice were injected with TLR9 ligand (50 μg/injection) and irradiated. The CD45.1 marker and CFSE labeling were used to identify transferred T cells. In this model system only transferred WT T lymphoyctes and not MyD88–/– lymphocytes respond to TLR9 stimulation. In Figure 6B, the data show that the numbers of WT CD4 T cells, recovered from irradiated mice, were significantly higher than MyD88–/– CD4 T cells. In non-IR mice, the numbers of transferred WT and MyD88–/– cells remain similar (Figure 6B). These data indicate that TLR9 stimulation of CD4 T cells does occur in vivo and that stimulation TLR9 protects CD4 T cells against the toxic effects of radiation.
TLR9 engagement on CD4 T lymphocytes in vivo show greater radioresistance than non-TLR–stimulated CD4 T lymphoyctes. (A) A schematic representation of the protocol used for the experiments described here. CD4 T cells were purified from WT CD45.1 and MyD88–/– CD45.2 BL/6 mice. Cells were activated with anti-CD3/CD28 Ab for 48 hours, pooled at a 1:1 ratio, labeled with CFSE, and intravenously injected into MyD88–/– mice (n = 5) followed by 3 intraperitoneal injections of TLR9 ligand (50 μg/injection) on days 1, 3, and 5. Mice were irradiated on day 6 (300 cGy). (B) The number of WT and MyD88–/– CD4 T lymphocytes recovered from the spleen and lymph nodes of IR and non-IR animals was determined using flow cytomety. The expression of the congenic markers CD45.1 and CD45.2 were used to identify transferred cells. The endogenous population of MyD88–/– T cells was distinguished from transferred MyD88–/– T cells based on their labeling with CFSE. The Student t test was used to determine P values between the indicated groups; *P < .05; ns indicates not significant.
TLR9 engagement on CD4 T lymphocytes in vivo show greater radioresistance than non-TLR–stimulated CD4 T lymphoyctes. (A) A schematic representation of the protocol used for the experiments described here. CD4 T cells were purified from WT CD45.1 and MyD88–/– CD45.2 BL/6 mice. Cells were activated with anti-CD3/CD28 Ab for 48 hours, pooled at a 1:1 ratio, labeled with CFSE, and intravenously injected into MyD88–/– mice (n = 5) followed by 3 intraperitoneal injections of TLR9 ligand (50 μg/injection) on days 1, 3, and 5. Mice were irradiated on day 6 (300 cGy). (B) The number of WT and MyD88–/– CD4 T lymphocytes recovered from the spleen and lymph nodes of IR and non-IR animals was determined using flow cytomety. The expression of the congenic markers CD45.1 and CD45.2 were used to identify transferred cells. The endogenous population of MyD88–/– T cells was distinguished from transferred MyD88–/– T cells based on their labeling with CFSE. The Student t test was used to determine P values between the indicated groups; *P < .05; ns indicates not significant.
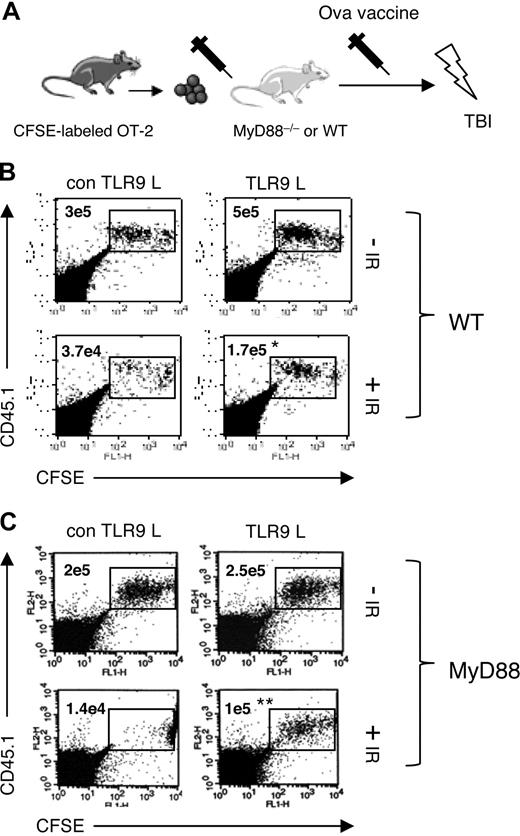
TLR9-stimulated, irradiated CD4 T cells respond to antigenic stimulation after total body irradiation
We evaluated whether TLR9-stimulated CD4 T cells maintained their ability to respond to antigenic stimulation after irradiation. As shown in Figure 7A, purified CD4 T cells from TCR transgenic OT-2 mice, which recognize an epitope derived from chicken ovalbumin protein, were labeled with CFSE and intravenously injected into WT or MyD88–/– CD45.2 mice. Twenty-four hours after adoptive transfer, mice were vaccinated with α-CD40 antibody, ovalbumin protein, and TLR9 or control ligand. Twenty-four hours after vaccination, mice were or were not irradiated. In TLR9-treated WT mice, the percentages and overall numbers of OT-2 T cells were higher than in non-TLR9 ligand–treated mice (Figure 7B dot plots). In contrast, the number of OT-2 T cells in irradiated, non-TLR ligand–treated mice, was significantly fewer as compared with TLR9 ligand–treated, irradiated mice (P = .013). Additionally, a greater frequency of the surviving OT-2 T cells in TLR9-treated, irradiated mice underwent proliferation. These data indicate that the administration of TLR9 ligand in WT mice contributes to OT-2 T-cell survival and expansion in spite of irradiation.
TLR9-stimulated OT-2 CD4 T lymphocytes respond to antigenic stimulation after total body irradiation. (A) A schematic representation of the protocol used for the experiments described here. Purified OT-2 CD4 T cells (106) were labeled with CFSE and intravenously injected into MyD88–/– mice or WT mice (n = 3). Twenty-four hours after adoptive T-cell transfer mice were vaccinated via intraperitoneal injection with ovalbumin protein (500 μg), α-CD40 antibody (50 μg) plus or minus TLR9 ligand (50 μg). One day after vaccination, mice were irradiated (TBI; 300 cGy) or not. OT-2 T-cell proliferation was evaluated in WT (B) and MyD88–/– (C) mice using flow cytometry 10 days after vaccination. Each CFSE peak, after the first peak, represents one cycle of cell division. The average number of OT-2 T cells recovered from the spleens of MyD88 or WT mice is shown on the dot plot. The Student t test was used to determine P values between the numbers of OT-2 cells in irradiated, TLR9 ligand–treated and irradiated, non-TLR9 ligand–treated mice; *P < .05, **P < .005.
TLR9-stimulated OT-2 CD4 T lymphocytes respond to antigenic stimulation after total body irradiation. (A) A schematic representation of the protocol used for the experiments described here. Purified OT-2 CD4 T cells (106) were labeled with CFSE and intravenously injected into MyD88–/– mice or WT mice (n = 3). Twenty-four hours after adoptive T-cell transfer mice were vaccinated via intraperitoneal injection with ovalbumin protein (500 μg), α-CD40 antibody (50 μg) plus or minus TLR9 ligand (50 μg). One day after vaccination, mice were irradiated (TBI; 300 cGy) or not. OT-2 T-cell proliferation was evaluated in WT (B) and MyD88–/– (C) mice using flow cytometry 10 days after vaccination. Each CFSE peak, after the first peak, represents one cycle of cell division. The average number of OT-2 T cells recovered from the spleens of MyD88 or WT mice is shown on the dot plot. The Student t test was used to determine P values between the numbers of OT-2 cells in irradiated, TLR9 ligand–treated and irradiated, non-TLR9 ligand–treated mice; *P < .05, **P < .005.
The radioprotective effects of TLR9 ligand observed in WT mice could have been through the stimulation of TLR9-responsive APCs such as DCs. Therefore, to determine the radioprotective effects of TLR9 stimulation on CD4 T cells in vivo, similar experiments to those described above were conducted using MyD88–/– mice as recipients. In TLR9 ligand–treated and untreated mice, similar percentages of OT-2 T cells (1.7% + 0.2% and 1.1% + 0.5%, respectively) were observed (Figure 7C). Moreover, OT-2 T cells from both these groups of mice underwent similar cycles of cell division. In control-treated, irradiated mice, OT-2 T cells comprised 0.1% + 0.05% of the total splenocyte population and proliferating cells were scarcely detectable; however, in TLR9-treated, irradiated mice, the percentage (0.7% + 0.2%) and overall number of OT-2 cells was higher (Figure 7C dot plot; P > .02). In addition, OT-2 T cells from TLR9-treated, irradiated mice proliferated in response to antigenic challenge. Together, these data indicate that TLR9-stimulated CD4 T cells, in vivo, are protected against the effects of total body irradiation and maintain their ability to divide in response to antigenic stimulation.
Discussion
We demonstrate that TLR9 engagement imparts a radioprotective effect on activated CD4 T cells. This radioprotective effect is manifested in vitro by decreased apoptosis, increased cell-cycle arrest, and an increased rate of DNA DSB repair, in TLR9-stimulated CD4 T cells. In vivo, the injection of TLR9 ligand rescued WT CD4 T cells but not MyD88–/– CD4 T cells after TBI. At the molecular level, the radioprotective effects of TLR9-stimulation required the participation of TLR9 and MyD88. Additionally, TLR9 was responsible for the increased activation of checkpoint kinases Chk1 and Chk2. Taken together, these findings identify a receptor (or family of receptors) that trigger a signaling cascade that preserves cellular longevity after exposure to IR.
These results, showing that TLR9 stimulation is important for T-cell survival, are consistent with those obtained in other cell types where this pathway influences cell life.19,20,23,24,34,50,,–53 In DCs, TLR9 stimulation has been shown to induce activation of phosphatidylinositol 3-kinase family (PI3K), and inhibition of this pathway reduces cell survival, suggesting that PI3K activation might be an important pathway for TLR9-mediated survival in T cells. The activation of DNA-PK, a member of the phosphatidylinositol 3-kinase like-kinase family (PIKK), has been shown to improve cell survival after TLR9 stimulation.54,55 Our data showing that wortmannin, which inhibits PI3K and PIKK activity, abolished the radioprotective effects of TLR9 stimulation, support the notion that TLR9 engagement on T cells triggers the activation of these families of kinases, which in turn up-regulates the antiapoptotic pathways. While some studies show that the survival of TLR9-stimulated macrophages depends on the activation of the MEK-ERK and PI3K-Akt signaling pathways other studies indicate that the PI3K-Akt pathway but not the DNA-PK or MEK-ERK pathways are required.20,54,–56 These findings clearly implicate PI3K and PIKK family members in TLR9-mediated survival, but also highlight the need for further investigation of the mechanisms responsible for the protective effect of TLR9 stimulation in different cell types.
Consistent with previous reports,34 we have shown that in response to TLR9 stimulation, CD4 T cells display increased expression of the antiapoptotic molecules. We postulate that increased Bcl-2 expression, for instance, is, in part, responsible for the reduced levels of programmed cell death after irradiation in these cells. Additionally, data obtained by various groups indicate that cell-cycle control is also linked to the expression of Bcl-2 or other antiapoptotic family members.33,57,,–60 For example, Linette et al demonstrated that lymphocytes from Bcl-2–deficient mice showed distinct differences in cell-cycle profile with increasing levels of Bcl-2 retarding the G0 to S-phase transition.61 Although we observed higher levels of Bcl-2 expression after TLR stimulation, we did not observe that TLR9 engagement of CD4 T cells resulted in a reduction in their rate of proliferation in the absence of IR; however, it is possible that the increased Bcl-2 expression resulting from TLR9 engagement and irradiation, in addition to inhibiting the activation of apoptosis, served to block cell proliferation in response to irradiation.
Ionizing radiation–induced DNA damage activates a host of cellular responses, including the triggering of cell-cycle checkpoints at the G1/S and G2/M transitions and a slowing of S-phase traversal.41 Here we show that TLR9-stimulated irradiated CD4 T cells undergo a significant reduction in proliferation and increased accumulation at G2/M checkpoint. While not directly assayed, the G1/S and S-phase checkpoints are likely activated as well. Principal participants in the activation of these checkpoints are the protein kinases ATM and ATR.62 In response to irradiation, ATM phosphorylates and activates the protein kinase Chk2 which, in turn, phosphorylates the protein kinase Cdc25C.63 Phosphorylated Cdc25C is subsequently sequestered to the cytoplasm,64 promoting accumulation of inactive Cdc2-cyclin B complex, thus blocking transit from G2 to M-phase. In a parallel pathway, the kinase ATR phosphorylates Chk1, which also inhibits Cdc25C activity.65,66 In our studies, irradiation combined with TLR9 engagement significantly increased the levels of phosphorylated Chk1 and Chk2 but did not have a measurable effect on the levels of phosphorylated/activated ATM. Conversely, in the absence of IR, TLR9 stimulation did not influence the phosphorylation status of Chk1 or Chk2, indicating that TLR9 stimulation produces a synergistic effect when combined with damage-induced signaling. Moreover, inhibition of these 2 kinases abrogated both the reduced entry into apoptosis and the increased rate of DNA DSB repair documented in irradiated CD4 T cells. These results strongly suggest that Chk1 and Chk2 are important components in the radioprotective effect imparted by TLR9 engagement.
At present, we do not understand the molecular nature of how TLR9 positively impacts Chk1 and Chk2 phosphorylation/activation or the rate of DNA DSB repair. One possibility is that TLR9 promotes the formation of complexes and/or localization of both Chk1 and Chk2 that makes these molecules more accessible to their respective activators. In support of this notion, it has been observed that Chk1, Chk2, and other key damage responsive molecules are components in various molecular complexes.67,,–70 Alternatively, it is plausible that TLR9 engagement down-regulates the mechanisms that dephosphorylate and inactivate Chk1 and Chk2. While the phosphatase(s) that negatively regulate Chk1 and/or Chk2 in mammalian cells have not been definitively identified, recent findings in yeast indicate that the phosphatase Dis2 is responsible for dephosphorylation of Chk1 after DNA damage, and mice null for the phosphatase PPM1D display increased phosphorylation of both Chk1 and Chk2.71,72 Of note, deficiency in DNA-PK, a kinase related to both ATM and ATR, also lead to heightened Chk1 and Chk2 activation in response to irradiation, although it remains undetermined if this observation is mechanistically linked to TLR9 engagement. Clearly, additional work is required to determine the mechanistic involvement of TLR9 stimulation on Chk1 and Chk2 activation.73
Our study provides the first proof that TLR9 stimulation of CD4 lymphocytes reduces their radiosensitivity. This has potential benefits for the combination of radiotherapy with immunotherapy to treat cancer patients. In support of this notion, others have noted that combining radiotherapy and immunotherapy is a useful approach for the better control of tumor growth.74 For example, intratumoral or local injection of TLR9 ligand synergizes with local radiotherapy in controlling tumor growth.9,10,12 Other studies demonstrated that TLR9 ligand can potentiate antitumor effects of radiotherapy against malignant glioma and rhabdomyosarcoma.11,13 While the function of radiotherapy, as an immune-enhancer, remains under investigation, the current view is that radiation facilitates the uptake and cross-presentation of tumor antigens to tumor-specific T lymphocytes by professional antigen presenting cells. There is the added advantage that radiotherapy can increase the expression of death receptors on some tumor cells and alter the extracellular matrix, facilitating the infiltration of T lymphocytes.75 Based on the data presented here, we propose that the administration of TLR9 ligands may also be used as a strategy to temporarily protect tumor-specific T lymphoyctes from the toxic effects of radiation, thus boosting T-cell responses. On the other hand, several groups have shown that tumor-reactive T cells from patients can be expanded in vitro and infused into the patient. Therefore, another strategy may be stimulate TLR9 on T cells during the expansion phase. We demonstrate that TLR9-stimulated CD4 T cells, irradiated in vivo, maintain their ability to respond to antigenic stimulation, indicating not only increased longevity but functional competence of these cells in mounting an immune response. These early studies support the hypothesis that TLR9 stimulation can enhance and/or maintain antitumor T-cell activity in vivo and could function to eliminate the small tumor burden remaining after radiotherapy.
The online version of this article contains a data supplement.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 USC section 1734.
Acknowledgments
The authors thank Dr Augusto Ochoa for critical review of this manuscript.
This work was supported by a National Institutes of Health (NIH) Center for Biomedical Research Excellence Grant (1P20 RR021970) and the Louisiana Cancer Research Consortium. K.D.B. was supported in part by a grant from NIH (R01-CA102289).
National Institutes of Health
Authorship
Contribution: L.Z., N.A., A.H.K., and P.R. performed research; K.D.B. designed research; and E.D. designed research and wrote the manuscript.
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Correspondence: Eduardo Davila, Department of Pediatrics, CSRB Rm 454, Louisiana State University Health Sciences Center, 533 Bolivar Street, New Orleans, LA 70112; e-mail: edavil@lsuhsc.edu.


This feature is available to Subscribers Only
Sign In or Create an Account Close Modal