Abstract
Introduction Autologous stem cell transplantation (ASCT) is the standard care for refractory and relapsed Hodgkin and aggressive non Hodgkin lymphoma, but patients (pts) with high tumor burden before transplantation present a very poor outcome. Furthermore, pts with advanced age or co-morbidities could not be eligible to the procedure. We tested efficacy and feasibility of reinforced mini-BEAM followed by hematopoietic stem cell infusion (mini-ASCT) either as extreme debulking attempt in pts with disappointing response to previous salvage therapy or in pts unsuitable for standard transplantation.
Patients and methods Ten Hodgkin’s lymphoma (HL), 10 aggressive B-cell non Hodgkin’s lymphoma (B-NHL) and 3 aggressive T-cell non Hodgkin’s lymphoma (T-NHL) pts received mini-BEAM therapy (BCNU 100 mg/m2 on d-6, VP-16 75 mg/m2/d and Ara-C 200 mg/m2/d from d-5 to d-2, Melphalan 100 mg/m2 on -d1) followed by peripheral blood stem cell infusion (PBSC). Median age was 44 years (range 23–67). Fifteen pts (65%) were primary refractory to first line therapy, while 5 pts and 3 pts had early and late relapse, respectively (22% and 13%); all 23 pts had received at least three previous therapies. Disease status before mini-BEAM was partial remission (PR) in 2 pts, stable disease (SD) in 7 pts and progressive disease (PD) in 14 pts.
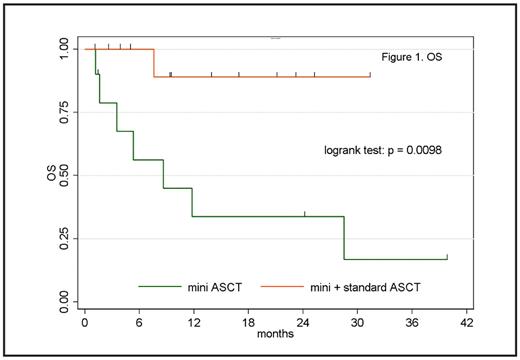
Results Median number of CD34+ cells infused was 5.77×106/kg (range: 1.4–20.0). Median time to neutrophils and platelets engraftment was 9 days (range 7–11) and 10 days (range 8–15), respectively. Nine pts (39%) had fever with a median duration of three days (range 1–5); only in 2/9 cases an infection was documented. Four pts (17%) experienced mucositis, requiring systemic opioid therapy in a single case. Median hospitalization was 25 days (range 21–37). Overall response rate (ORR) was 34.8% (CR 8.7%, PR 26.1%); 8 pts (34.8%) presented SD and 7 pts (30.4%) PD. Standard ASCT was performed in 12 pts; 11 pts were excluded because of co-morbidities (6 pts) or progressive disease (5 pts). Eleven pts are evaluable for response to ASCT: 5 pts reached CR (41.7%) and 6 PR (50%). Considering all the 23 pts, median overall survival (OS) was 28.5 months with a median follow-up of 9.4 months (range 1.1–39.8), while median event-free survival (EFS) was 13 months with a median follow-up of 5.2 months (range 1.0–39.8). Analysing pts undergone mini plus standard ASCT (cohort 1) apart from pts treated with mini ASCT alone (cohort 2), median OS was not reached in cohort 1 and 8.6 months in cohort 2, with a median follow-up of 11.7 months (range: 2.6–31.4) and 5.3 months (range: 1.1–39.8), respectively (Figure 1); median EFS was not reached in cohort 1 and 3.3 months in cohort 2, with a median follow-up of 13.1 months (range: 3.5–31.4) and 2.8 months (range: 1.0–39.8), respectively (Figure 2). Both differences in OS and EFS are statistically significant (logrank test: p = 0.0098 and p = 0.0187). At univariate analysis, a significant association was detected between standard ASCT and OS (p = 0.009), while both histology (p = 0.831) and response to mini-BEAM (p = 0.364) did not exert any valuable impact on OS.
Conclusion ASCT with reduced BEAM as conditioning regimen proved to be a feasible and safe strategy for pts with refractory lymphoma which failed multiple salvage therapies. In this unfavourable setting of pts, ORR was better than expected. Survival data show an advantage for pts subsequently treated with standard ASCT, which must be performed whenever possible. Mini-ASCT can play a role for disease reduction in a tandem-fashion before standard ASCT in younger and to some extent chemosensitive pts. Finally, mini-ASCT can be considered as a valid option for pts uneligible to standard transplantation.
Disclosures: No relevant conflicts of interest to declare.
Author notes
Corresponding author


This feature is available to Subscribers Only
Sign In or Create an Account Close Modal