Abstract
We have reported that outcome of transplant-eligible patients (pts) with relapsed and primary refractory HL is determined by three pre-second-line chemotherapy (ST) risk factors (RF): remission duration of <1 yr., extranodal disease and B symptoms. In addition, normalization of FDG-PET prior to ASCT is the most important factor predicting favorable EFS. We now report the preliminary results of an ongoing phase II risk-adapted study where HL pts receive the following: Favorable risk (0–1 RF) - one cycle of standard dose ifosfamide, carboplatin and etoposide (ICE) ST followed by one cycle of augmented ICE; unfavorable risk (2-RF)- 2 cycles of augmented ICE. All pts then underwent a restaging FDG-PET and the results determined the next treatment. Pts with a negative FDG-PET went directly to HDT/ASCT; however if the FDG-PET was still positive, pts received an additional four biweekly cycles of gemcitabine (1000 mg/m2), vinorelbine (20 mg/m2) and liposomal doxorubicin (15 mg/m2) (GVD) followed by repeat FDG-PET scan; pts without evidence of progression then received HDT/ASCT. Preceding high-dose chemotherapy and ASCT, patients that were radiation therapy-naive received involved field radiotherapy (IFRT) followed by total lymphoid irradiation. Selected previously irradiated patients received only IFRT.
Sixty-two pts are evaluable; median follow-up of surviving pts is 30 months; median age was 35. Forty-eight pts had a remission duration of < 1 yr. of those, 28 had primary refractory disease; 28 had extranodal disease and 11 had B symptoms. All patients had previously failed doxorubicin-based chemotherapy; 18 had received prior radiation; of those, 13 failed in the radiation field.
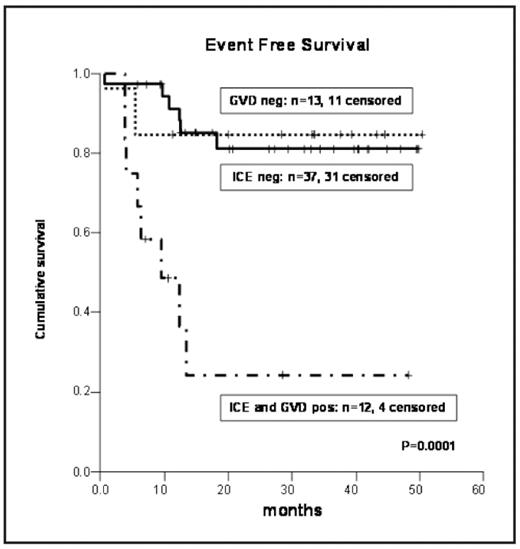
Following first ST chemotherapy with ICE, 3 pts progressed, while 37 pts normalized their FDG-PET scan and currently 31 of these pts are event-free. Twenty-five pts with an improving CT scan after ICE still had a persistently positive FDG-PET; they received the second ST with GVD. Of these, 13 pts normalized their FDG-PET scan and 11 are eventfree; the remaining 12 pts had persistently abnormal FDG-PET scan or progressed; only 4 of them are event-free. There was no difference in outcome between the pts who had normal FDG-PET after ICE (pre-ASCT) and those who achieved a negative FDG-PET scan because of the additional ST with GVD. Both of these cohorts had a statistically significant improvement in EFS compared to pts with a persistently positive FDG-PET. In total 46/62 (65%) pts on this program are currently event-free. One pt died from sepsis. Conclusion: For pts with relapsed and primary refractory HL our evolving strategy is to administer ST until normalization of FDG-PET is achieved prior to HDT/ASCT.
Disclosures: No relevant conflicts of interest to declare.
Author notes
Corresponding author

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal