Abstract
Fanconi anemia (FA) is an inherited recessive DNA repair disorder mainly characterized by bone marrow failure and cancer predisposition. Studies in mosaic FA patients have shown that reversion of one inherited germ-line mutation resulting in a functional allele in one or a few hematopoietic stem cells (HSCs) can lead to the proliferation advantage of corrected cells, thus over time normalizing the hematologic status of the patient. In contrast to these observations, it is still unclear whether ex vivo genetic correction of FA HSCs also provides a similar proliferation advantage to FA HSCs. Using an FA mouse model with a marked hematopoietic phenotype, the FA-D1 (Brca2Δ27/Δ27) mice, we demonstrate that the lentivirus-mediated gene therapy of FA HSCs results in the progressive expansion of genetically corrected clones in mild-conditioned FA-D1 recipients. Consistent with these data, hematopoietic progenitors from FA recipients progressively became mitomycin C resistant and their chromosomal instability was reverted. No evidence of myelodysplasia, leukemias, or abnormal clonal repopulation was observed at multiple time points in primary or secondary recipients. Our results demonstrate that ectopic expression of BRCA2 confers a beneficial in vivo proliferation advantage to FA-D1 HSCs that enables the full hematopoietic repopulation of FA recipients with genetically corrected cells.
Introduction
Fanconi anemia (FA) is a rare inherited disease characterized by congenital abnormalities, progressive bone marrow failure, and cancer susceptibility.1 So far, 13 complementation groups, associated with mutations in the corresponding FA genes, have been described.2
The demonstration of somatic mosaicism in FA patients evidenced the natural proliferation advantage of hematopoietic stem cells (HSCs) that have reverted a pathogenic mutation in one of the affected alleles.3-5 Somatic mosaicism in FA, acting as a natural gene therapy (GT), constitutes the principal basis suggesting that the transplantation of a limited number of genetically corrected HSCs in either unconditioned or moderately conditioned recipients will progressively repopulate and thus normalize the hematopoiesis of FA patients.
Although the GT of CD34+ bone marrow (BM) cells in severe combined immunodeficiency (SCID) patients with defects in the interleukin-2 (IL-2) receptor common γ-chain (X1) or in the adenosine deaminase gene led to a strong proliferation advantage of genetically corrected T cells,6-8 a similar response has not been observed in FA patients undergoing analogous GT clinical trials.9-11 In addition, whereas the transduction of mouse FA-HSCs with therapeutic vectors enhances the repopulating ability of these cells in vivo,12,13 an external selective pressure was required to promote a proliferation advantage of genetically corrected FA-HSCs in transplanted recipients.14-16 Although this may be the result of the relatively mild phenotype of FA mouse models used in these studies (FA-A and FA-C), the question as to whether HSCs subjected to ex vivo GT actually acquire a proliferation advantage, similar to what has been observed in mosaic patients,3-5 remains unanswered.
In contrast to previous studies showing that cytotoxic treatments were required to facilitate the engraftment and/or selection of wild-type (WT) HSCs in FA-A, FA-C, and FA-G recipients,17-19 we have recently shown the natural proliferation advantage of WT HSCs transplanted in unconditioned FA-D1 recipients (with a hypomorphic mutation in the Brca2 gene; Brca2Δ27Δ27 mice).20 Interestingly, long-term analyses in these mice revealed an almost complete repopulation of their hematopoiesis by WT cells, provided that sufficient numbers of WT BM cells were transplanted.20
The marked hematopoietic defects of FA-D1 mice,20 together with the increased propensity of these animals to develop cancer,21 demonstrate the more severe phenotype of these animals compared with other FA mouse models.22-27 Based on these observations, we aimed to investigate whether the gene therapy of FA-D1 HSCs was sufficient to confer proliferation advantage after transplantation in FA-D1 recipients. To achieve this goal, a self-inactivating lentiviral vector (LV) expressing the human BRCA2 cDNA gene was generated and used to genetically modify BM grafts from FA-D1 mice. In addition to the improved safety properties of these vectors,28 recent studies have shown that LVs enable the rapid transduction of Fanca−/− HSCs, preserving the engraftment potential of these cells.29 Data presented in this study demonstrate, for the first time, that ex vivo GT confers a proliferation advantage of transduced FA HSCs versus untransduced donor and host FA HSCs in a submyeloablative-conditioning FA mouse model.
Methods
Animals
BALB/c mice with a homozygous deletion in exon 27 of the Fancd1/Brca2 gene (FA-D1 or Brca2Δ27Δ27 mice) were used throughout.21 As controls, WT littermates were used in all the experiments. All experimental procedures were carried out according to Spanish and European regulations (Spanish RD 223/88 and OM 13-10-89 of the Ministry of Agriculture, Food and Fisheries; and European convention ETS-123, for the use and protection of vertebrate mammals used in experimentation and other scientific purposes).
LV production
LVs carrying either the hBRCA2 or the EGFP genes, under the control of the spleen focus-forming virus (SFFV) promoter, were generated as shown in Figure 1A. 293T and HT1080 cells (CRL-12103; ATCC, Manassas, VA) used to produce and titrate the LVs grown in Dulbecco modified medium (DMEM; Invitrogen, Carlsbad, CA) supplemented with 10% fetal bovine serum (FBS; Sigma-Aldrich, St Louis, MO), 2 mM L-glutamine (Cell Culture Systems; Invitrogen), 50 U/mL penicillin-streptomycin (Invitrogen). For the production of LVs, 293T cells were transfected with 5 μg of pCDNL-BH, 3 μg of vesicular stomatitis virus G, and 20 μg of SFFV-hBRCA2 or SFFV-enhanced green fluorescence protein (EGFP) as previously described.30,31 Supernatants were harvested 48 hours after transfection, filtered through a 0.45-μm filter, and concentrated by ultracentrifugation. Functional titers of infective LVs were determined in HT1080 cells, plated at 3.5 × 104 cells per well in 24-well plates, and infected overnight with different dilutions of either LV. Cells were washed and incubated for 5 days with fresh medium. Cells were recovered using lysis buffer from QIAGEN (Valencia, CA) and analyzed by quantitative polymerase chain reaction (qPCR) for the presence of the LV provirus in cellular DNA. Because of the large size of the BRCA2 cDNA, low titers of BRCA2-LVs were routinely obtained (105-106 transduction units/mL, after concentration). Titers corresponding to EGFP-LVs were, however, approximately 109 transduction units/mL. To avoid differences in the efficiency of gene transfer, transductions with both vectors were always conducted at equivalent multiplicities of infection.
Restored formation of nuclear Rad51 foci in FA-D1 mouse fibroblasts transduced with LVs expressing hBRCA2. (A) Description of the LVs harboring the hBRCA2 (BRCA2-LV) and EGFP cDNA (EGFP-LV) used throughout. (B) Percentages of mouse FA-D1 fibroblasts with Rad51 foci after 20 hours of incubation in the presence or absence of 30 nM MMC. Data are mean plus or minus SEM of 3 independent experiments. A total of 200 cells were scored in each condition. (C) Representative immunofluorescence pictures corresponding to analysis shown in panel B. *Significant difference (P < .05). N.S. indicates not significant.
Restored formation of nuclear Rad51 foci in FA-D1 mouse fibroblasts transduced with LVs expressing hBRCA2. (A) Description of the LVs harboring the hBRCA2 (BRCA2-LV) and EGFP cDNA (EGFP-LV) used throughout. (B) Percentages of mouse FA-D1 fibroblasts with Rad51 foci after 20 hours of incubation in the presence or absence of 30 nM MMC. Data are mean plus or minus SEM of 3 independent experiments. A total of 200 cells were scored in each condition. (C) Representative immunofluorescence pictures corresponding to analysis shown in panel B. *Significant difference (P < .05). N.S. indicates not significant.
Phenotypic correction of FA-D1 fibroblasts with BRCA2-LVs
Ear fibroblasts from WT and FA-D1 mice were obtained by the desegregation of ear fragments with collagenase (0.25%) in DMEM supplemented with 10% FBS, 2 mM L-glutamine (Invitrogen), and 50 U/mL penicillin-streptomycin (Invitrogen) incubated for 8 hours at 37°C. Explants were washed and incubated overnight in DMEM supplemented with 10% FBS, 2 mM L-glutamine (Invitrogen), and 50 U/mL penicillin-streptomycin (Invitrogen). WT and FA-D1 mouse fibroblasts were transduced either with BRCA2-LVs or EGFP-LVs and seeded in plates with cover slides at a cell density of 7.5 × 104 cells per well, either with or without 30 nM of the interstrand cross-linker drug, mitomycin C (MMC; Sigma-Aldrich). Sixteen hours later, cells were fixed with 3.7% paraformaldehyde in phosphate-buffered saline (PBS) for 15 minutes, and permeabilized with 0.5% Triton X-100 in PBS for 5 minutes. After blocking for 30 minutes in the blocking buffer (10% FBS, 0.1% Nonidet P-40 [NP-40] in PBS), cells were marked with an anti-Rad51 mouse monoclonal antibody (Abcam, Cambridge, United Kingdom). Cells were subsequently washed and incubated with antimouse Texas Red–conjugated antibody (Jackson ImmunoResearch Laboratories, Cambridgeshire, United Kingdom) in combination with 4,6-diamidino-2-phenylindole. Forty-five minutes afterward, cells were washed 3 times with Tris-buffered saline, and the slides were mounted in Moviol. Slides were analyzed with a fluorescence microscope Axioplan2 (Carl Zeiss, Göttingen, Germany) using a 100×/1.45 oil working distance 0.17-mm objective. The number of cells with foci was scored after analyzing 200 cells per slide. Immunofluorescent images were acquired with an AxioCam MRm (Carl Zeiss) and were processed with AxioVision version 4.6.3 (Carl Zeiss) and Corel Photo-Paint 11 (Corel, Ottawa, ON).
Phenotypic correction of FA-D1 BM progenitors transduced with BRCA2-LVs
BM cells from FA-D1 mice were transduced as previously described.31 Briefly, cells were maintained overnight in Iscove modified Dulbecco medium (Invitrogen) supplemented with 20% FBS, 2 mM L-glutamine (Invitrogen), 50 U/mL penicillin-streptomycin (Invitrogen), human recombinant (hr) IL-11(100 ng/mL), and murine stem cell factor (mSCF; 100 ng/mL; both from Chemicon International, Temecula, CA) at a concentration of 105 cells/mL, and transduced with either BRCA2-LVs or EGFP-LVs for 16 hours. In some experiments (Figure 2), aliquots consisting of 5 × 104 mononuclear cells were maintained in liquid cultures with mSCF and hIL-11 and assessed for colony-forming cells (CFCs) in semisolid MethoCult GF M3534 culture medium (StemCell Technologies, Vancouver, BC). To determine whether the genetic treatment reverted the hypersensitivity of FA-D1 CFCs, BM cultures were conducted with and without 10 nM MMC.
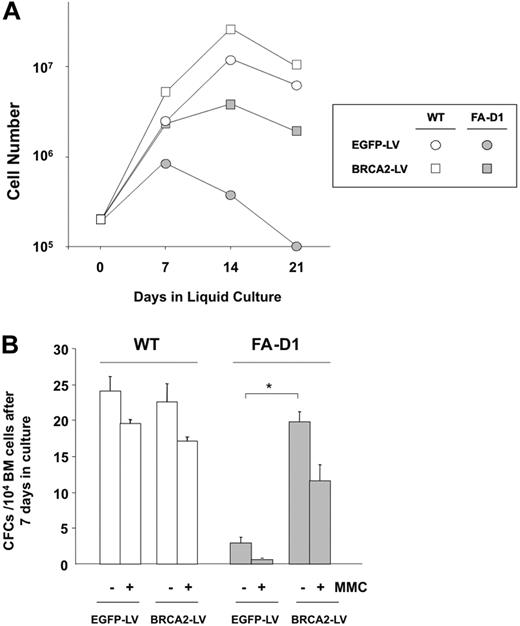
Correction of the in vitro proliferation defects and MMC hypersensitivity of FA-D1 BM progenitors transduced with LVs that express hBRCA2.C (A) Kinetics of ex vivo expansion of WT (○, □) and FA-D1 ( ,
,  ) BM cells previously transduced with EGFP-LVs or BRCA2-LVs (circles and squares, respectively). Data from a representative experiment are shown. (B) Content in CFCs of cultures corresponding to panel A after 7 days of ex vivo expansion in the absence or presence of 10 nM MMC. Data are mean plus or minus SEM of data obtained from 5 plates per point. *Significant difference between cells transduced with EGFP and BRCA2-LVs (P < .05).
) BM cells previously transduced with EGFP-LVs or BRCA2-LVs (circles and squares, respectively). Data from a representative experiment are shown. (B) Content in CFCs of cultures corresponding to panel A after 7 days of ex vivo expansion in the absence or presence of 10 nM MMC. Data are mean plus or minus SEM of data obtained from 5 plates per point. *Significant difference between cells transduced with EGFP and BRCA2-LVs (P < .05).
Correction of the in vitro proliferation defects and MMC hypersensitivity of FA-D1 BM progenitors transduced with LVs that express hBRCA2.C (A) Kinetics of ex vivo expansion of WT (○, □) and FA-D1 ( ,
,  ) BM cells previously transduced with EGFP-LVs or BRCA2-LVs (circles and squares, respectively). Data from a representative experiment are shown. (B) Content in CFCs of cultures corresponding to panel A after 7 days of ex vivo expansion in the absence or presence of 10 nM MMC. Data are mean plus or minus SEM of data obtained from 5 plates per point. *Significant difference between cells transduced with EGFP and BRCA2-LVs (P < .05).
) BM cells previously transduced with EGFP-LVs or BRCA2-LVs (circles and squares, respectively). Data from a representative experiment are shown. (B) Content in CFCs of cultures corresponding to panel A after 7 days of ex vivo expansion in the absence or presence of 10 nM MMC. Data are mean plus or minus SEM of data obtained from 5 plates per point. *Significant difference between cells transduced with EGFP and BRCA2-LVs (P < .05).
Analysis of the in vivo–repopulating properties of FA-D1 hematopoietic stem cells transduced with BRCA2-LVs
BM samples from male FA-D1 donors were enriched in precursor cells negative for lineage differentiation markers (Lin−) using the Lineage Depletion Kit from Miltenyi Biotec (Bergisch Gladbach, Germany) following the manufacturer's instructions. Lin− cells were then transduced as indicated in the previous section with BRCA2- and EGFP-LVs. Sixteen hours after transduction, cells were washed and aliquots of 5 × 105 cells were transplanted into FA-D1 female mice previously irradiated with 3 Gy (x-rays from a MG-325 equipment set at 300 kV, 12.8 mA; Philips, Hamburg, Germany).20 Monthly after transplantation, peripheral blood (PB) samples were obtained from FA-D1 female recipients, and the level of donor chimerism was analyzed by qPCR using primers for the male-specific SRY sequence and mouse β-actin in a Rotor Gene RG-3000 (Corbett Research Products, Foxboro, MA).20 Similar studies were conducted in hematopoietic colonies generated by BM cells obtained from femoral aspirates periodically obtained after transplantation. In these studies, individual colonies were picked and analyzed by a real-time quantitative reverse transcriptase-polymerase chain reaction (qRT-PCR).32 The presence of LV proviruses in these colonies was also determined using primers specific for the Rev-responsive element (RRE) present in the lentiviral backbone: lenti–RRE-F: 5′-ATCTCTAGCAGTGGCGCCC-3′ and lenti–RRE-R: 5′-CTGCGTCGAGAGAGCTCCTC-3′ and detected with the TaqMan probe lenti–RRE-P: 5′-FAM-CAGGGACTTGAAAGCGAAAGGGAAACC-BHQ1-3′. In some experiments, BM was harvested from primary recipients (6 months after transplantation) and retransplanted into secondary recipients (107 cells/mouse) previously irradiated with 3 Gy. Samples from these animals were studied as in primary recipients.
Analysis of hBRCA2 expression in BM from recipient FA-D1 mice
The expression of human mRNA in the BM of recipients of BRCA2-transduced cells was analyzed by qRT-PCR on cDNA obtained from total RNA. Samples from one mouse that received EGFP-transduced cells were used as a negative control. The relative transgene expression of hBRCA2 was determined by the 2−ΔΔCt as previously described (where Ct is the cycle threshold).33 Primers used for hBRCA2 expression analyses were as follows: BRCA2-F: 5′-CTTATGTTGCACAATGAGAAAAGAAATTAG-3′; and BRCA2-R: 5′-CGGAATCGGGCAAAACG-3′, as a probe BRCA2-P: 5′-FAM-ATTTACCTCAGCGTTTGTGTATCGGGCAAA-BHQ1-3′. For housekeeping control expression, murine glyceraldehyde-3-phosphate dehydrogenase (mGAPDH) was used: mGAPDH-F: 5′-TCCAAGGAGTAAGAAACCCTGGA-3′ and mGAPDH-R: 5′-GAAATTGTGAGGGAGATGCTCAG-3′ and mGAPDH-P: 5′-TR-TGAGCAAGAGAGAGGCCCTATTCCAACTC-BHQ2-3′ probe.
Structural chromosomal abnormalities
Liquid cultures of BM cells were left untreated or were treated with 30 nM MMC for a 48-hour period. To obtain metaphases, colcemid (0.1 μg/mL; Invitrogen, Paisley, United Kingdom) was added 2 hours before harvesting, and the cells were processed following standard cytogenetic procedures. Briefly, cells were dropped onto clean slides and air-dried overnight. Slides were stained with 10% Giemsa in phosphate buffer, pH 6.8. Ten metaphases per sample were analyzed for chromosome aberrations, including gaps, chromosome and chromatid breaks, acentric fragments, and chromosome- and chromatid-type exchanges.
Linear amplification–mediated PCR analyses
For the detection of the lentiviral integration sites, BM-DNA from primary and secondary recipients was extracted and preamplified by repeated primer extension using vector-specific 5′-biotinylated primers, SK-LTR1 (5′-GAGCTCTCTGGCTAACTAGG-3′) and SK-LTR2 (5′-GAACCCACTGCTTAAGCCTCA-3′) from 100 ng of each sample DNA. Selection of biotinylated extension products was performed with 200 μg of magnetic beads according to the manufacturer's instructions (Dynal Biotech, Oslo, Norway). The samples were incubated with Klenow polymerase (2 U; Roche Applied Science, Penzberg, Germany), deoxynucleoside triphosphates (250 μM), and a random hexanucleotide mixture (Roche Applied Science) in a volume of 20 μL for 1 hour at 37°C. Samples were washed on the magnetic particle concentrator (Dynal Biotech) and incubated with Tsp509I endonuclease (4 U in 20 μL; New England Biolabs, Beverly, MA) for 1 hour at 65°C. After an additional wash step, 100 pmol of a double-stranded asymmetric linker cassette and Fast Link Ligation Kit (2 U; Epicenter Technologies, Madison, WI) were incubated with the beads in a volume of 10 μL at room temperature for 5 minutes. Denaturing was performed with 5 μL 0.1 N NaOH for 10 minutes at room temperature. Each ligation product was amplified with AmpliTaq gold polymerase (5 U; Applied Biosystems, Foster City, CA), vector-specific primer SK-LTR3 (5′-AGCTTGCCTTGAGTGCTTCA-3′) (0.5 μM), and linker cassette primer LCP1 (5′-GACCCGGGAGATCTGAATTC-3′) (0.5 μM).28 Of each PCR product, 0.2% served as a template for a second, nested PCR with internal primers SK-LTR4 (5′-AGTAGTGTGTGCCCGTCTGT-3′) and LCP2 (5′-GATCTGAATTCAGTGGCACAG-3′) at identical conditions. Of this final product, one-fifth was separated on a Spreadex high-resolution gel, EL800 and EL400 (Elchrom Scientific, Cham, Switzerland).
Results
The LV-mediated expression of human BRCA2 corrects the cellular phenotype of mouse FA-D1 fibroblasts and BM progenitors in vitro
Because mutations in FANCD1/BRCA2 result in a defective induction of nuclear Rad51 foci after DNA damage,34 we investigated whether the transduction of mouse FA-D1 fibroblasts with BRCA2-LVs restored the formation of Rad51 foci after treatment with MMC. As expected, the proportion of WT cells with Rad51 foci increased markedly after an MMC exposure. Consistent with our previous findings,20 a defective generation of Rad51 foci after MMC treatment was observed in mouse FA-D1 fibroblasts transduced with EGFP-LVs. Significantly, the transduction of these cells with BRCA2-LVs restored the generation of Rad51 foci after MMC treatment, confirming the capacity of BRCA2-LVs to restore the homologous recombination pathway in mouse FA-D1 cells (Figure 1B,C).
Because defects in Fancd1/Brca2 also impair the proliferation capacity of BM progenitors and hypersensitize these cells to MMC, in the next set of experiments BM cells from WT and FA-D1 mice were transduced with EGFP- and BRCA2-LVs and then maintained in liquid cultures for 3 weeks. During this period, the cellularity of the cultures was periodically analyzed. In addition, total numbers of CFCs and numbers of MMC-resistant CFCs were determined 1 week after seeding. As shown in a representative experiment illustrated in Figure 2A, the growth of cultures established with EGFP-LV–transduced FA-D1 cells was very poor, whereas the transduction of FA-D1 cells with BRCA2-LVs markedly improved their proliferation potential. Compared with CFC numbers generated by WT BM cells, transduced either with EGFP- or BRCA2-LVs, EGFP-LV–transduced samples from FA-D1 mice contained very low numbers of CFCs (∼ 10% of normal values). In addition, these CFCs were highly sensitive to MMC. Transduction of FA-D1 BM samples with BRCA2-LVs significantly increased both the numbers and the MMC resistance of FA-D1 CFCs (Figure 2B).
The LV-mediated expression of hBRCA2 promotes an in vivo repopulation advantage of FA-D1 HSCs in FA-D1 recipients
To investigate whether BRCA2-LVs restored the in vivo–repopulating properties of FA-D1 HSCs, BM transplantation studies were conducted. In recent studies, we showed that BM cells from WT mice were capable of progressively repopulating the hematopoiesis of nonconditioned FA-D1 recipients up to 100%, provided that relatively high numbers of BM cells (approximately one femoral BM per recipient) were infused.20 To engraft FA-D1 mice with BM cells numbers similar to what would be required in human GT studies, we first evaluated the impact of conditioning these animals with a mild irradiation of 3 Gy, before the infusion of 500 000 Lin− WT BM cells (equivalent to one-fourth BM from a femur). Consistent with our previous observations,20 this number of BM cells did not engraft in unconditioned FA-D1 recipients. A mild conditioning with only 3 Gy facilitated, however, a predominant WT exogenous repopulation in 2 to 3 months after transplantation (Figure 3A). These data strongly suggested that a reduced conditioning regimen might be sufficient to facilitate the engraftment of FA-D1 recipients with low numbers of genetically corrected HSCs.
In vivo repopulation advantage of FA-D1 BM cells transduced with BRCA2-LVs in the PB of FA-D1 recipients conditioned with mild irradiation. (A) Influence of a mild conditioning of 3 Gy to facilitate the engraftment of FA-D1 recipients with moderate numbers (500 000 Lin− cells) of fresh BM cells from WT mice. Follow-up of donor engraftments obtained between 1 and 3 months after transplantation. □ and ■ represent unirradiated recipients and recipients irradiated with 3 Gy before the BM transplantation, respectively. (B) Kinetics of donor hematopoietic repopulation in FA-D1 recipients conditioned with 3 Gy and transplanted with 500 000 FA-D1 Lin− BM cells that were transduced with BRCA2- or EGFP-LVs. Donor repopulation data were obtained by qPCR analyses of SRY sequences (Y-chromosome specific) in PB samples from recipient mice. Mice 1 to 6 were transplanted with BRCA2-transduced cells. Mice 7 to 9 were transplanted with EGFP-transduced cells.
In vivo repopulation advantage of FA-D1 BM cells transduced with BRCA2-LVs in the PB of FA-D1 recipients conditioned with mild irradiation. (A) Influence of a mild conditioning of 3 Gy to facilitate the engraftment of FA-D1 recipients with moderate numbers (500 000 Lin− cells) of fresh BM cells from WT mice. Follow-up of donor engraftments obtained between 1 and 3 months after transplantation. □ and ■ represent unirradiated recipients and recipients irradiated with 3 Gy before the BM transplantation, respectively. (B) Kinetics of donor hematopoietic repopulation in FA-D1 recipients conditioned with 3 Gy and transplanted with 500 000 FA-D1 Lin− BM cells that were transduced with BRCA2- or EGFP-LVs. Donor repopulation data were obtained by qPCR analyses of SRY sequences (Y-chromosome specific) in PB samples from recipient mice. Mice 1 to 6 were transplanted with BRCA2-transduced cells. Mice 7 to 9 were transplanted with EGFP-transduced cells.
Two independent GT experiments were then conducted with Lin− BM cells from FA-D1 male mice either transduced with EGFP- or BRCA2-LVs. Cells doses of 500 000 transduced cells were transplanted into female FA-D1 recipients previously irradiated with 3 Gy (Figure 3B). As expected, moderate levels of donor repopulation were observed in recipients transplanted with EGFP-LV–transduced samples (Figure 3B). These levels remained stable over time, therefore suggesting that after the initial engraftment these cells did not have any proliferation advantage in vivo against the endogenous FA-D1 hematopoietic cells. Strikingly, FA-D1 grafts transduced with BRCA2-LVs mediated a progressive increase of donor repopulation in all FA-D1 recipients, reaching values of 80% to 100% in the PB at the end of the observation period (6 months after transplantation; Figure 3B). As expected, additional control experiments showed that transduction of WT BM cells with BRCA2-LVs did not promote any proliferation advantage in samples that already express Brca2 (data not shown).
To determine the contribution of donor cells in the BM and to analyze whether the in vivo proliferation advantage of FA-D1 repopulating cells harboring the hBRCA2 was the result of the presence of the transgene, BM aspirates from transplanted recipients were obtained at 2 and 6 months after transplantation and plated in standard progenitor assays. Hematopoietic colonies were individually picked and subjected to qPCR analyses to determine the proportion of CFCs of donor origin (SRY+ colonies) and positive for the LV provirus. In parallel, similar analyses were conducted on EGFP-LV–transduced samples. As shown in Figure 4A, the proportion of donor CFCs markedly increased from 2 to 6 months after transplantation in 5 of the 6 recipients that were transplanted with BRCA2-transduced FA-D1 cells. In the sixth recipient, the engraftment was already very high 2 months after transplantation. Significantly, 6 months after transplantation, more than 70% of CFCs in the BM of mice that had received BRCA2-LV–transduced cells were of donor origin, in good consistency with engraftments determined in the PB of these animals (Figure 4A).
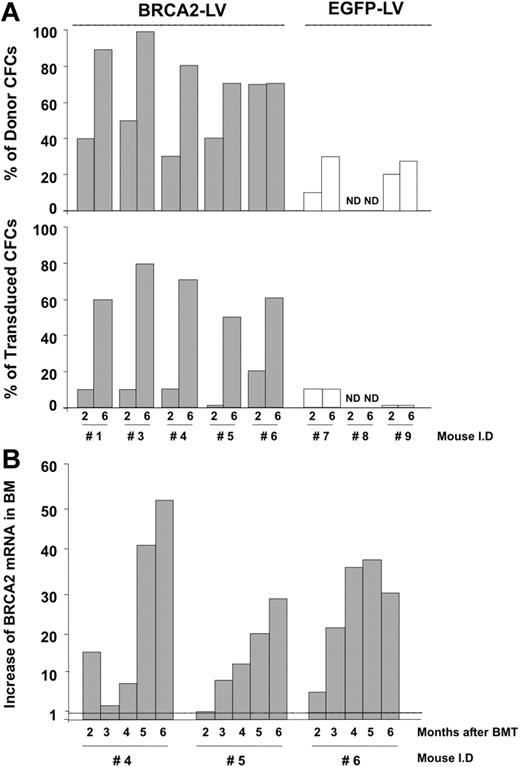
Characterization of the hematopoietic progenitors repopulating the BM of FA-D1 recipients after transplantation with EGFP- or hBRCA2-transduced FA-D1 cells. (A) Quantification of the proportion of CFCs present in the BM of FA-D1 recipients of donor origin (top panel) harboring BRCA2-LV or EGFP-LV proviruses (bottom panel). qPCR analyses of SRY sequences and of BRCA2 and EGFP-LV proviruses were determined in individually picked colonies generated by BM samples obtained 2 and 6 months after transplantation. (B) Kinetics of hBRCA2 mRNA expression in BM samples from 3 FA-D1 recipients transplanted with BRCA2-transduced cells. BM samples were periodically aspirated from the femora of recipient mice and analyzed by RT-PCR. Data show the increase in hBRCA2 expression compared with a mouse transplanted with EGFP-transduced cells (mouse 9).
Characterization of the hematopoietic progenitors repopulating the BM of FA-D1 recipients after transplantation with EGFP- or hBRCA2-transduced FA-D1 cells. (A) Quantification of the proportion of CFCs present in the BM of FA-D1 recipients of donor origin (top panel) harboring BRCA2-LV or EGFP-LV proviruses (bottom panel). qPCR analyses of SRY sequences and of BRCA2 and EGFP-LV proviruses were determined in individually picked colonies generated by BM samples obtained 2 and 6 months after transplantation. (B) Kinetics of hBRCA2 mRNA expression in BM samples from 3 FA-D1 recipients transplanted with BRCA2-transduced cells. BM samples were periodically aspirated from the femora of recipient mice and analyzed by RT-PCR. Data show the increase in hBRCA2 expression compared with a mouse transplanted with EGFP-transduced cells (mouse 9).
The marked proliferation advantage of BRCA2-LV–transduced HSCs and progenitor cells was confirmed when the proportion of CFCs harboring the BRCA2-LV provirus was investigated (Figure 4A). Whereas 5% to 20% of the CFCs obtained at 2 months after transplantation carried the BRCA2-LV provirus, 60% to 80% of progenitors were positive for the BRCA2-LV provirus at 6 months after transplantation, indicating that most of the donor CFCs in recipients' BM harbored the therapeutic hBRCA2 LV. As expected, in the case of samples transduced with EGFP-LVs, only a reduced proportion of CFCs harbored the proviral LV at 2 and 6 months after transplantation.
Because the repopulation advantage of BRCA2-LV–transduced FA-D1 BM should be a consequence of the ectopic expression of the transgene, we sought to prove that the level of hBRCA2 mRNA would continuously increase over time in the BM of mice. To this end, BM samples were aspirated periodically from the femora of 3 FA-D1 recipients (mice 4-6), and the level of hBRCA2 mRNA was determined by qRT-PCR. Data were normalized using BM cells from one FA-D1 recipient that was transplanted with EGFP-transduced BM cells (mouse 9). As shown in Figure 4B, a progressive increase in the level of hBRCA2 mRNA was observed in these BM samples along the posttransplantation period, further supporting the relevance of the expression of the hBRCA2 transgene in the proliferation advantage of FA-D1 HSCs.
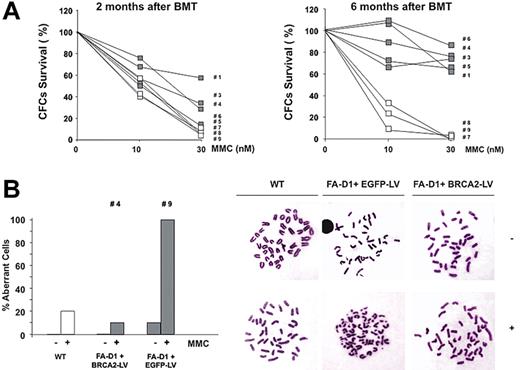
To further confirm that BRCA2-LVs restored the cellular phenotype of mouse FA-D1 BM cells in vivo, the characteristic hypersensitivity of FA CFCs to MMC in BM cells from FA-D1 recipients was assessed at 2 and 6 months after transplantation. Whereas only a modest correction of the MMC hypersensitivity of FA-D1 CFCs was observed 2 months after transplantation of BRCA2-LV–transduced cells, a marked reversion of the MMC hypersensitivity was observed when analyses were conducted 6 months after transplantation (Figure 5A). At this time point, more than 90% of the colonies that survived to 30 nM MMC were positive for the BRCA2-LV provirus (data not shown).
Reversion of the phenotype of BM cells from FA-D1 mice after transplantation with genetically corrected BM cells. (A) Reversion of the MMC sensitivity of hematopoietic progenitors present in the BM of recipient mice transplanted with BRCA2-transduced FA-D1 BM cells. The figure shows the increased resistance to MMC in samples obtained 6 months after BMT, compared with samples obtained 2 months after BMT. (B) Reversion of the chromosomal instability of BM cells from mice transplanted with BRCA2-LVs. The figure represents the chromosomal instability, spontaneous and MMC-induced, in BM cells from one recipient mouse corresponding to the therapeutic and control groups (mouse 4 and mouse 9, respectively).
Reversion of the phenotype of BM cells from FA-D1 mice after transplantation with genetically corrected BM cells. (A) Reversion of the MMC sensitivity of hematopoietic progenitors present in the BM of recipient mice transplanted with BRCA2-transduced FA-D1 BM cells. The figure shows the increased resistance to MMC in samples obtained 6 months after BMT, compared with samples obtained 2 months after BMT. (B) Reversion of the chromosomal instability of BM cells from mice transplanted with BRCA2-LVs. The figure represents the chromosomal instability, spontaneous and MMC-induced, in BM cells from one recipient mouse corresponding to the therapeutic and control groups (mouse 4 and mouse 9, respectively).
Because FA-D1 BM cells are characterized by their chromosomal instability,20 we also investigated whether our GT approach reverted this phenotype in BM cells of one FA-D1 recipient transplanted with BRCA2-LV–transduced cells (no. 4), compared with a control FA-D1 recipient transplanted with EGFP-LV–transduced cells (no. 9). As seen in the cytogenetic analyses shown in Figure 5B, the genetic correction of FA-D1 BM cells completely reverted the chromosomal instability characteristic of FA-D1 cells, providing an additional proof for the efficacy of the GT approach for restoring the functionality of FA-D1 precursor cells capable of repopulating mildly conditioned recipients.
To finally demonstrate that the correction of transduced FA-D1 cells occurred in true HSCs, BM samples from 2 primary recipients transplanted with BRCA2-transduced BM (no. 1 and no. 3) were retransplanted into 1 or 2 secondary FA-D1 recipients (107 BM cells/secondary recipient) also preconditioned with 3 Gy. As a control, BM cells from one recipient transplanted with EGFP-transduced cells were also retransplanted into one secondary 3 Gy–conditioned recipient. Nine months after transplantation, secondary recipients were killed to determine the level of donor cell engraftment and also the percentage of genetically modified cells (Figure 6A). As deduced from the analysis of PB samples, the engraftment of secondary FA-D1 recipients by the original donor BM cells (male origin) reached values of 80% to 100% when samples were transduced with the therapeutic BRCA2-LV, but not with the control vector (Figure 6B). The very high repopulating ability of BRCA2-transduced FA-D1 HSCs was confirmed when BM CFCs from secondary recipients were analyzed. As happened in primary recipients, most of the CFCs from these animals were of donor origin and harbored the therapeutic BRCA2-LV (Figure 6C). Consistent with these data, most of the progenitors corresponding to the BRCA2 group survived to MMC doses that were highly toxic for CFCs from the control group (30 nM MMC; Figure 6D). Taken together, these data clearly demonstrate the reverted phenotype, including a long-term proliferation advantage, of genetically corrected FA-D1 HSCs.
Long-term repopulation ability of FA-D1 HSCs genetically corrected with BRCA2-LVs. (A) Schematic representation of the experimental protocol used to assess the long-term repopulating capacity of FA-D1 BM grafts transduced with BRCA2-LVs. Six months after the infusion of EGFP- or BRCA2-transduced FA-D1 BM cells, recipients were killed and BM cells from 2 recipients corresponding to the therapeutic group (recipients 1 and 3) and from one recipient of the control group (recipient 9) were transplanted (107 BM cells per mouse) into 4 secondary FA-D1 recipients (recipients 1.1, 3.1, 3.2, and 9.1) previously irradiated with 3 Gy. (B) Analysis of the proportion of donor repopulation (cells positive for SRY sequences) in the PB of secondary recipients 9 months after BMT. (C) Proportion of donor-derived CFCs (SRY+; ▩) and the proportion of transduced CFCs (hBRCA2+ or EGFP+; ■) as deduced from qPCR analyses conducted with individually picked colonies. (D) Percentage of CFCs obtained from the BM of secondary recipients (9 months after BMT) that survived to 30 nM MMC added to the clonogenic cultures.
Long-term repopulation ability of FA-D1 HSCs genetically corrected with BRCA2-LVs. (A) Schematic representation of the experimental protocol used to assess the long-term repopulating capacity of FA-D1 BM grafts transduced with BRCA2-LVs. Six months after the infusion of EGFP- or BRCA2-transduced FA-D1 BM cells, recipients were killed and BM cells from 2 recipients corresponding to the therapeutic group (recipients 1 and 3) and from one recipient of the control group (recipient 9) were transplanted (107 BM cells per mouse) into 4 secondary FA-D1 recipients (recipients 1.1, 3.1, 3.2, and 9.1) previously irradiated with 3 Gy. (B) Analysis of the proportion of donor repopulation (cells positive for SRY sequences) in the PB of secondary recipients 9 months after BMT. (C) Proportion of donor-derived CFCs (SRY+; ▩) and the proportion of transduced CFCs (hBRCA2+ or EGFP+; ■) as deduced from qPCR analyses conducted with individually picked colonies. (D) Percentage of CFCs obtained from the BM of secondary recipients (9 months after BMT) that survived to 30 nM MMC added to the clonogenic cultures.
The proliferation advantage of genetically corrected FA-D1 BM grafts is not the result of a monoclonal expansion of transduced HSCs caused by insertional mutagenesis
Although no evidence of leukemias or myelodysplastic syndromes was deduced from PB cell counts and histologic examination of recipient mice (data not shown), we investigated whether BRCA2-LV–transduced cells exhibited an altered clonal repopulation pattern, which could account for the repopulation advantage observed in recipient FA-D1 mice. To rule out this possibility, we determined the clonal repertoire present in the BM from primary and secondary FA-D1 recipients by linear amplification–mediated PCR (LAM-PCR). As shown in Figure 7, a similar pattern of oligoclonal repopulation was observed in mice transplanted with either BRCA2- or EGFP-LV–transduced grafts. This observation, and the absence of a monoclonal repopulation in any of the animals transplanted with the therapeutic vector, indicated that the proliferation advantage of genetically corrected FA-D1 HSCs was not the result of dysregulated proliferation of these cells. These data are consistent with our results in Figures 3 and 4, showing, for the first time, that the restored function of BRCA2 confers a proliferation advantage in FA-D1 HSCs transplanted into mild-conditioned FA-D1 recipients.
LAM-PCR analysis of the clonal repertoire repopulating the BM of primary and secondary FA-D1 recipients transplanted with genetically corrected FA-D1 grafts. The figure represents the clonal repertoire detected in the BM of primary (6 months after BMT) and secondary recipients (9 months after secondary BMT) originally transplanted with BRCA2- and EGFP-transduced FA-D1 BM cells (see protocol in Figure 6A). Arrows indicate the position of the internal band. * indicates nonspecific bands that were amplified in different LAM-PCR analyses.
LAM-PCR analysis of the clonal repertoire repopulating the BM of primary and secondary FA-D1 recipients transplanted with genetically corrected FA-D1 grafts. The figure represents the clonal repertoire detected in the BM of primary (6 months after BMT) and secondary recipients (9 months after secondary BMT) originally transplanted with BRCA2- and EGFP-transduced FA-D1 BM cells (see protocol in Figure 6A). Arrows indicate the position of the internal band. * indicates nonspecific bands that were amplified in different LAM-PCR analyses.
Discussion
The acquisition of an in vivo proliferation advantage in HSCs subjected to ex vivo GT constitutes a critical aspect for the therapy of patients with autologous genetically corrected HSCs. In this situation, the question of whether transduced HSCs and their progeny acquire in vivo proliferation advantage over uncorrected cells is of fundamental importance to define whether any conditioning strategy of FA patients before reinfusion of cells will be necessary. Successful genetic therapies in patients without an in vivo selection advantage for the transduced cells, such as in chronic granulomatous disease, required the conditioning of the patients with myelosuppressive protocols.35 In patients with SCIDs, adenosine deaminase-SCID patients could be successfully engrafted after nonmyeloablative conditioning,7 whereas SCID-X1 patients were successfully engrafted without any conditioning.6,8
In FA, normalized values of all lineages in PB can be observed in some patients with somatic mosaicism,3-5 demonstrating that the natural self-correction in one allele of the affected FA gene can confer spontaneous in vivo repopulation advantage of reverted FA HSCs and their progeny. Although these observations strongly suggested that the progeny of FA HSCs subjected to ex vivo GT will acquire proliferation advantage over untransduced cells in vivo, no evidence for this phenomenon has been found so far in recipients of FA HSCs that were transduced with therapeutic vectors. In the murine system, a number of studies have already shown the efficacy of gammaretroviral,12,14 lentiviral,16 and foamyviral13 vectors for restoring the functionality of FA-HSCs. However, the in vivo proliferation advantage of corrected HSCs and their progeny was only detected when animals that received transplants were later exposed to genotoxic treatments.14-16 In 3 clinical trials with gammaretroviral vectors where FA patients received corrected autologous CD34+ cells without any conditioning, neither long-term persistence of genetically marked hematopoietic cells nor any clinical improvement was observed.9-11 These results raise the concern that, in contrast to observations made in FA mosaic patients, ex vivo genetic correction may not be sufficient to confer proliferation advantage to HSCs after reinfusion.
To investigate whether a lentiviral GT approach may result in a proliferation advantage of corrected FA HSCs in vivo, we took advantage of mice with a hypomorphic mutation on both alleles of the Brca2 gene.21 In this FA-D1 model, we have recently reported the progressive repopulation of the entire hematopoietic system in these animals with WT HSCs in the absence of any preparative treatment either before or after transplantation.20 FA-D1 mice therefore appear to be an ideal model system to investigate whether GT confers an in vivo growth advantage to corrected autologous FA HSCs and their progeny over the unmodified endogenous cells.
To this end, an LV expressing the 10.3-kb cDNA of the human BRCA2 was constructed. Because human and mouse FA-D1 cells are characterized by a deficient induction of nuclear Rad51 foci after DNA damage,20,34 we initially demonstrated the functionality of our BRCA2-LV by the restoration of Rad51 foci formation in mouse FA-D1 fibroblasts exposed to MMC (Figure 1). We also demonstrated normal proliferation capacity and resistance to MMC in FA-D1 cells transduced with the BRCA2-LV. Strikingly, without MMC, the proportion of cells with RAD51 foci was higher in BRCA2-LV–transduced FA-D1 cells than in WT cells, either transduced with EGFP- or BRCA2-LVs. This observation could be explained by increased levels of spontaneous DNA damage that had been accumulated in FA-D1 cells before restoration of the deficient FA/BRCA pathway with the therapeutic vector. Important additional evidence for the ability of the hBRCA2-LV to correct the phenotype of mouse FA-D1 cells is the correction of the ex vivo expansion capacity and MMC hypersensitivity of FA-D1 BM progenitors.
Based on our previous data showing that the engraftment of nonconditioned FA-D1 mice requires infusion of high numbers of WT BM cells,20 and considering the low numbers of HSCs that can be obtained from FA patients,11 we decided to prepare our FA-D1 recipients with a mild irradiation of 3 Gy before the transplantation with transduced BM cells. As deduced from the analysis of PB of recipients early after transplantation, this preparative regimen facilitated the initial engraftment of FA-D1 mice with genetically corrected FA-D1 HSCs, similar to that seen with BM cells from WT mice. In addition, our experiments showed that the transduction of FA-D1 BM cells with the BRCA2-LV mediated a progressive increase in the proportion of genetically corrected donor CFCs during the posttransplantation time, as demonstrated by the increased resistance to MMC. These observations and the fact that the expression of the hBRCA2 transgene progressively increased after transplantation clearly indicate that the expression of the therapeutic hBRCA2 transgene continues to confer a proliferation advantage of FA-D1 HSCs in FA-D1 recipients months after the mild conditioning. Cytogenetic analyses conducted in the BM of these animals also revealed the reversion of the chromosomal instability in corrected FA-D1 BM cells. Finally, the results obtained after the transplantation of FA-D1 recipient BM into secondary recipients provide final proof that the correction of the hematopoietic phenotype was the result of genetic modification of FA-D1 HSCs with the BRCA2-LV.
Because previous clinical35,36 and experimental studies37 have shown that proviral integrations in the vicinity of specific genes can mediate clonal dominance in transplanted recipients, we wanted to exclude that this mechanism accounted for the repopulation advantage that we had observed in animals receiving BRCA2-transduced FA-D1 HSCs. Therefore, LAM-PCR analyses were conducted on BM cells from primary and secondary recipient mice. Our data in Figure 7 confirmed that several transduced clones were present in each mouse as a consequence of the repopulation of the animals with either BRCA2- or EGFP-transduced grafts. These findings are in good consistency with our results showing that, although both viruses had integrated into repopulating cells, the proliferation advantage of genetically modified FA-D1 HSCs was only associated with the re-expression of the hBRCA2 gene in FA-D1 BM cells.
Although none of our animals showed any symptom of malignancy, safety issues suggest that the use of strong promoters, such as the SFFV used in this study, should be limited to diseases in which a high expression of the therapeutic transgene is required for the therapeutic effect or the size of the cDNA might be a critical factor in achieving sufficient protein levels.38,39 Therefore, further studies should be conducted in the different subtypes of FA to investigate whether a weak expression system of the corresponding gene can be curative.31
The role that cytokines released by the mild conditioning of recipients had on the engraftment and in vivo proliferation of genetically corrected FA-D1 HSCs is open to discussion. On the one hand, it is possible that, at least initially after transplantation, cytokines such as tumor necrosis factor-α or interferon-γ might have promoted a preferential growth of genetically corrected over uncorrected FA-D1 precursors, as already shown in FA-A, FA-C, and FA-G mice that had received continuous infusions with these cytokines.18,19 On the other hand, the short in vivo half-life of these effects/cytokines and our data showing proliferation advantage of WT HSCs in nonconditioned FA-D1 suggest that the release of cytokines may not be the critical factor here. It appears also highly improbable that the mild irradiation might be the main reason for the continuous expansion of the pool of genetically corrected cells over months. Therefore, we postulate that the more severe hematopoietic phenotype of FA-D1 mice, especially compared with other FA mouse models, and the re-expression of BRCA2 are the critical factors that can readily explain the proliferation advantage in FA-D1 HSCs, leading to progressive in vivo expansion of corrected cells over months.
In conclusion, it is important to take into account that, although the cellular phenotype of FA-D1 mice is most severe among all the FA mouse models, the hematopoietic defects in these FA-D1 mice20 are still milder than those observed in the majority of FA patients. The data presented here therefore suggest that the transduction of human FA-HSCs with therapeutic LVs will promote the repopulation advantage of genetically corrected cells after transplantation in FA patients. The FA-D1 mouse model might therefore be an important tool to develop novel strategies to improve both engraftment and in vivo expansion of autologous cells, genetically modified by integrating vector systems introducing the therapeutic gene.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 USC section 1734.
Acknowledgments
The authors thank M. Garín for the careful reading of the manuscript and helpful suggestions; Sergio García, Jesús Martínez, and Elena López for excellent technical work; and Roser Pujol for cytogenetic analysis.
This work was supported by grants from the European Program “Life Sciences, Genomics and Biotechnology for Health” (Concerted Safety and Efficiency Evaluation of Retroviral Transgenesis [CONSERT]; Ref 005242), Comisión Interministerial de Ciencia y Tecnología (SAF2005-00058 and SAF-2006-03440), Centro de Investigación Biomédica en Red de Enfermedades Raras (CIBERER), and Genoma España. Centro de Investigaciones Energéticas, Medioambientales y Tecnológicas (CIEMAT) also received support from the Marcelino Botín Foundation for Translational Research on Biomedicine. This work was also supported by a grant from Consejo de Desarrollo Científico Humanístico y Tecnológico–Universidad de Los Andes (CDCHT-ULA; M-941-08-07-A) (N.W.M.) and Deutsche Forschungsgemeinschaft (H2322/1, SPP1230) (H.H.).
Authorship
Contribution: P.R., N.W.M., A.G.-M., S.N., L.A., J.S., M.C., and G.G. performed the experiments; and J.A.B., P.R., J.C.S., and H.H. designed the experiments and wrote the paper.
Conflict-of-interest disclosure: H.H. may receive royalties based on a license agreement between Indiana University and Takara Shuzo, Ltd, resulting from the sale of the fibronectin fragment CH296 (Retronectin). The remaining authors declare no competing financial interests.
Correspondence: Juan A. Bueren, Hematopoiesis and Gene Therapy Division, Centro de Investigaciones Energéticas, Medioambientales y Tecnológicas, Avda Complutense, No. 22, 28040 Madrid, Spain; e-mail: juan.bueren@ciemat.es.





This feature is available to Subscribers Only
Sign In or Create an Account Close Modal