Abstract
Allografts from HLA-matched sibling donors were mobilized and collected without granulocyte colony-stimulating factor (G-CSF) using AMD3100, a direct antagonist of CXCR4/stromal-derived factor 1 (SDF-1/CXCL12). Donors (N = 25) were treated with AMD3100 at a dose of 240 μg/kg by subcutaneous injection, and leukapheresis was then initiated just 4 hours later. Two-thirds of the donors collected an allograft with a CD34+ cell dose sufficient for transplantation after just one dose of AMD3100. No donor experienced more than grade 1 toxicity. After a myeloablative regimen, 20 patients with hematologic malignancies received allografts collected after AMD3100 alone. All patients engrafted neutrophils (median day 10) and platelets (median day 12) promptly. Acute graft-versus-host disease (GVHD) grades 2 through 4 occurred in 35% of patients. One patient died due to complications related to acute GVHD. No unexpected adverse events were observed in any of the recipients. All 14 patients surviving in remission have robust trilineage hematopoiesis and are transfusion-free with a median follow-up of 277 days (range, 139-964 days). Direct antagonism of CXCR4 by AMD3100 may provide a more rapid and possibly less toxic and cumbersome alternative to traditional G-CSF–based mobilization in normal donors. This trial was registered as no. NCT00241358 at www.ClinicalTrials.gov.
Introduction
Mobilization of hematopoietic stem and progenitor cells (HSPCs) from the bone marrow into the peripheral blood (PB) after granulocyte colony-stimulating factor (G-CSF) stimulation has become the standard method to collect allografts from healthy adult related donors for transplantation in patients with hematologic malignancies.1 G-CSF–mobilized HSPCs are associated with more rapid engraftment, a shorter hospital stay, and in some circumstances superior overall survival in comparison to unmanipulated bone marrow.2 While the use of mobilized HSPCs removes the requirement for a surgical procedure to obtain a sufficient allograft, donors often experience moderate albeit transient morbidity related to G-CSF administration.3 Because optimal mobilization requires from 4 to 6 days of G-CSF administration, donors may experience significant inconvenience, including absence from work during the mobilization process. While no long-term sequelae have been confirmed with short-term G-CSF administration, there are reports of serious acute toxicities related to its use as well as concerns that it can induce genetic and epigenetic modifications in hematopoietic cells.3-6 Accordingly, a safer and more rapid method for mobilizing and procuring HSPCs is highly desirable.
While the exact mechanisms by which G-CSF induces HSPC mobilization are not firmly established, multiple studies have indicated that the interaction between the chemokine stromal-derived factor 1 (SDF-1/CXCL12) and its receptor CXCR4 functions as a key regulator of HSPC trafficking.7-11 Disruption of this interaction either through cleavage of SDF-1 and CXCR4 or down-regulation of SDF-1 expression results in the rapid egress of HSPCs from the bone marrow. AMD3100 (Plerixafor; Genzyme, Cambridge, MA) is a small bicyclam molecule that functions as a reversible inhibitor of SDF-1 binding to CXCR4.10,12,13 Studies in murine models as well as healthy human volunteers and later patients have demonstrated a dose-dependent increase in HSPC mobilization within a few hours of AMD3100 administration.10,13,14 Importantly, short-term administration of AMD3100 has been shown to be well tolerated.13-15 A phase 2 trial demonstrated significant enhancement of HSPC mobilization when AMD3100 was combined with G-CSF in patients with non-Hodgkin lymphoma (NHL) and multiple myeloma.16 Two phase 3 studies comparing HSPC mobilization with G-CSF alone to G-CSF combined with AMD3100 were recently completed and showed a highly significant benefit for the AMD3100 plus G-CSF arms.17,18
Given these observations, we hypothesized that substituting AMD3100 for G-CSF would permit a potentially safer and more rapid method to procure HSPCs from healthy donors. The results of a pilot trial of HSPC mobilization with single-agent AMD3100 presented herein suggest that a direct antagonist of the SDF-1/CXCR4 interaction can safely and effectively mobilize functional HSPCs for the reconstitution of hematopoiesis after myeloablative chemoradiotherapy without the requirement for G-CSF.
Methods
Patients and donors
Eligible patients were between the ages of 18 and 65 years inclusive, had advanced hematologic malignancies suitable for transplantation, and had an HLA-identical sibling donor willing and able to donate a mobilized allograft. Patients had to have evidence of adequate organ function (left ventricular ejection fraction more than 40%, formal pulmonary function testing showing a forced expiratory volume in 1 second [FEV1] more than 50% of predicted and a diffusing lung capacity for carbon dioxide [DLCO] more than 40% of predicted [corrected for hemoglobin]), a serum creatinine clearance of more than 40% of normal, a total bilirubin less than 2 times normal or absence of hepatic fibrosis/cirrhosis, no evidence of a severe central or peripheral neurologic abnormality, no evidence of active infection at the time of the transplant preparative regimen, be HIV negative, and have an Eastern Cooperative Oncology Group (ECOG) performance status of 0 or 1. Eligible donors were between the ages of 18 and 70 years inclusive with evidence of adequate organ function as defined here for patients (although no formal cardiac or pulmonary function testing was performed in donors in the absence of symptoms or positive history), were HIV negative, and had an ECOG performance status of 0 or 1.
Both patients and donors gave written informed consent in accordance with the Declaration of Helsinki on a study approved by the Human Studies Committee (HSC) at Washington University. The study was also approved by The Food and Drug Administration (FDA) under an investigator-held investigational new drug (IND) application (IND no. 67227)
Donor mobilization procedure
All eligible donors received the same dose of AMD3100 (240 μg/kg based on actual donor weight) administered by subcutaneous injection at 8 am the morning of planned leukapheresis (LP; day 1). All donors were subsequently observed for signs of toxicity related to AMD3100 and if stable, began a standard large volume (20 L) LP at 12 pm the same day. Toxicities encountered by donors were graded according to the National Cancer Institute (NCI) common toxicity criteria (CTCAE) version 3.0. All mobilized products were collected using a Cobe Spectra apheresis device (Gambro BCT, Lakewood, CO). LP was performed using peripheral venous access (17-gauge needle) whenever possible. The minimum CD34+ cell dose necessary to proceed to transplantation was set at 2.0 × 106 CD34+ cells/kg actual recipient weight. There was no upper limit to the CD34+ cell dose for transplantation. If the minimum CD34+ cell dose for transplantation was reached on the first day of LP, no further collections were performed. That is, there was no “target” CD34+ cell dose, just the minimum dose required to proceed to transplantation. If the minimum CD34+ cell dose was not achieved after the first day of mobilization with AMD3100, the donor was asked to return in 2 days to repeat the identical process on day 3. Under those circumstances, if the combined total CD34+ cell dose from days 1 and 3 was at or above the minimum specified dose, the mobilization with AMD3100 was considered successful. Otherwise, the donor was considered an AMD3100 mobilization failure. A follow-up complete blood count (CBC) with differential count was drawn at or around 30 days after completion of the AMD3100 injection, and a telephone contact was made by the study coordinator to assess whether blood counts and symptoms had returned to baseline.
The original protocol required all donors to consent to undergo mobilization and LP first using AMD3100. Regardless of whether the mobilization and collection process after AMD3100 was considered a success, the donors underwent a 7-day “washout” period, then were administered G-CSF alone at 10 μg/kg subcutaneously once daily with a 20-L LP commencing on day 5 and continuing daily for a maximum of 3 collections until the minimum CD34+ cell dose was achieved. All allografts were collected before the patient received transplant conditioning and were cryopreserved in dimethyl sulfoxide (DMSO) under controlled rate freezing conditions. If the allograft mobilized after AMD3100 contained at least the minimum CD34+ cell dose, that allograft alone was thawed and transplanted on day 0 following conditioning. The G-CSF mobilized allograft was reserved as a “backup” in the event the AMD3100 mobilized allograft did not result in neutrophil engraftment by day 21. In that event, the G-CSF–mobilized allograft was to be thawed and transplanted. After 10 donor/recipient pairs had been enrolled and 8 patients received transplants of AMD3100-mobilized allografts, it became clear that the AMD3100 allografts were functioning well and there was no need to collect a “backup” allograft with G-CSF. At that point, the study was amended to remove the requirement for a mandatory G-CSF mobilization provided that the minimum CD34+ cell dose was achieved following AMD3100. The amendment was approved by the FDA and the Washington University HSC, and the remaining 15 donors underwent mobilization after AMD3100 alone.
Conditioning regimen, GVHD prophylaxis, and supportive care
All patients received the same conditioning regimen consisting of cyclophosphamide at 60 mg/kg (ideal weight or adjusted for obesity) intravenously daily for 2 doses on days −3 and −2, followed by single-dose total body irradiation (TBI) delivered at a dose rate of 30 cGy/min for a total dose of 550 cGy on day −1 as previously described.19 All 20 patients who underwent transplantation received previously cryopreserved AMD3100-mobilized allografts that were thawed on day 0. Postthaw viability was assessed using trypan blue exclusion. All patients received an identical graft-versus-host disease (GVHD) prophylaxis regimen consisting of single-agent cyclosporine at 3 mg/kg per day (based on ideal body weight) by continuous intravenous infusion beginning on day −2. Patients were switched to oral cyclosporine once they were able to tolerate it. Target trough cyclosporine levels were 200 to 400 ng/mL. Cyclosporine tapering commenced on day 100 in the absence of GVHD. No methotrexate was given. This is the standard GVHD prophylaxis we have used with this conditioning regimen after HLA-matched sibling donor transplantation, and outcomes have been previously reported.19,20
All patients received subcutaneous G-CSF at 5 μg/kg per day beginning day 1 and continuing until the absolute neutrophil count (ANC) was more than 1.5 × 109/L (1500/μL) for 3 days. All patients received prophylactic acyclovir, but no routine bacterial or fungal prophylaxis was given. Patients with febrile neutropenia received broad-spectrum antibiotics according to Infectious Disease Society of America (IDSA) guidelines.21
Definitions
Neutrophil engraftment was defined as a rise in the ANC to 0.5 × 109/L (500/μL) or greater for 2 consecutive days after a conditioning regimen–induced nadir. Platelet engraftment was defined as the first day of platelet count greater than 20 × 109/L (20 000/μL) without transfusion for 7 consecutive days. Primary graft failure was defined as failure of neutrophil engraftment by day 28. Secondary graft failure was defined as primary engraftment followed by a drop in the neutrophil count to less than 0.5 × 109/L (500/μL) for more than 3 consecutive days without any apparent cause such as drugs or opportunistic infection. Patients with acute leukemia in first complete remission, myelodysplastic syndrome with refractory anemia or refractory anemia with ring sideroblasts, and chronic myelogenous leukemia in chronic phase were considered to have low-risk disease. All other patients were placed in the high-risk disease category. Acute and chronic GVHD were graded according to standard criteria.22,23 In most circumstances, attempts were made to obtain skin biopsies or biopsies of other relevant organs to confirm the diagnosis of acute or chronic GVHD, but the diagnosis could be made on clinical grounds only. Relapse was defined as reappearance of disease for patients in remission or the progression of disease for patients who received transplantations who were with active disease.
Chimerism analysis and immunophenotyping
Chimerism status was monitored in the PB by analysis of separated T-cell (CD3+) and granulocyte (CD15+) preparations using short tandem repeat techniques typically on or around days 28, 84, 180, and 365 after transplantation. Full donor chimerism was defined as greater than or equal to 95% donor cells within each compartment analyzed. Immunophenotyping was performed on donors during the mobilization phase on fresh specimens of peripheral blood progenitor cells (PBPCs) or PB. Lineage-negative (negative for CD3, CD14, CD11b, and CD19) CD34+ cells were measured by a modification of the technique of Roscoe et al.24 Lymphocyte subsets were enumerated by mixing samples containing 106 leukocytes with the following 4 cocktails of fluorescent-conjugated antibodies (Beckman-Coulter, Fullerton, CA): (1) CD3–fluorescein isothiocyanate (FITC), CD4-phycoerythrin (PE), CD8–phycoerythrin-Texas red (ECD), and CD45-PE-Cy5; (2) CD3-FITC, CD56-PE, CD19-ECD, and CD45-PE-Cy5; (3) CD2-FITC and CD45-PE-Cy5; and (4) IgG1-FITC, IgG1-PE, IgG1-ECD, and CD45-PE-Cy5. After 30 minutes of incubation at 4°C, a red cell lysis procedure was performed using 0.15 M NH4Cl, and samples were fixed with 1% paraformaldehyde. All flow cytometry analyses were performed on side-scatter CD45 gated lymphocytes using a Coulter Elite cytometer equipped with an argon laser (Beckman-Coulter, Fullerton, CA).
In a subset of 4 donors, analysis of naive, central memory (TCM), effector memory (TEM), and CD45RA-expressing effector memory (TEMRA) T-cell subsets in fresh PB samples was performed using monoclonal antibodies (all from Becton Dickinson, San Jose, CA; clone designations in parentheses) to CD3 (SK7), CD4 (RPA-T4), CD8 (Hit8a), CD27 (M-T271), CD45RA (L48), and CD62L (SK11) on a Coulter FC-500 flow cytometer (Beckman-Coulter, Miami, FL) within 24 hours of collection. FOXP3 staining was performed with a FOXP3 staining kit from eBioscience (San Diego, CA) according to the manufacturer's protocol.
Statistical considerations
Follow-up was through February 21, 2007, or on the last contact prior to that date. Nonparametric Wilcoxon–Mann-Whitney tests were used to compare continuous variables. Kaplan-Meier and Cox proportional hazards models were used to calculate time to acute GVHD, chronic GVHD, relapse, disease progression, and death from any cause. Time to chronic GVHD was examined among the subset of patients who were alive on day 100 after transplantation. The significance of differences between PB T-cell subsets before and 6 hours after administration of AMD3100 was tested using paired Student t tests. P values less than .05 were considered significant. Analyses were run using Stata 10.0 (Stata Corporation, College Station, TX).
Results
Patient and donor characteristics
A total of 25 HLA-identical sibling donor/recipient pairs were enrolled on this study between June 2004 and December 2006. Patient and donor characteristics are presented in Table 1. The median patient age was 52 years (range, 31-65 years). Of these, 15 were women and 10 were men. The most common diagnosis before transplantation was acute myeloid leukemia (AML). A total of 16 patients with high-risk disease and 4 patients with low-risk disease underwent transplantation. Median donor age was 52 years (range, 24-66 years). Of these, 20 were men and 5 were women. The median donor weight was 88.6 kg (range, 52.7-133.2 kg). All donors underwent large volume LP, processing up to 20 L of blood per LP procedure.
Recipient and donor characteristics
| . | Recipient . | Donor . |
|---|---|---|
| Median age, y (range) | 52 (31-65) | 52 (24-60) |
| Sex, no. M/F | 10/15 | 20/5 |
| Weight, kg (range) | 85 (53-130) | 88.6 (52.7-133) |
| Diagnosis | ||
| AML | 10 | |
| ALL | 4 | |
| NHL | 6 | |
| CML (AP) | 1 | |
| CLL | 3 | |
| MDS | 1 | |
| Risk group | ||
| High | 21 | |
| Low | 4 | |
| Sex mismatch | 10/25 |
| . | Recipient . | Donor . |
|---|---|---|
| Median age, y (range) | 52 (31-65) | 52 (24-60) |
| Sex, no. M/F | 10/15 | 20/5 |
| Weight, kg (range) | 85 (53-130) | 88.6 (52.7-133) |
| Diagnosis | ||
| AML | 10 | |
| ALL | 4 | |
| NHL | 6 | |
| CML (AP) | 1 | |
| CLL | 3 | |
| MDS | 1 | |
| Risk group | ||
| High | 21 | |
| Low | 4 | |
| Sex mismatch | 10/25 |
AML indicates acute myeloid leukemia; ALL, acute lymphoblastic leukemia; CML (AP): accelerated phase chronic myelogenous leukemia; NHL, non-Hodgkin lymphoma; CLL, chronic lymphocytic leukemia; and MDS, myelodyplastic syndrome.
Donor mobilization with AMD3100
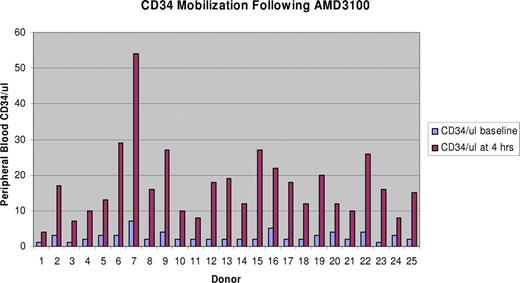
All 25 donors enrolled received at least one dose of AMD3100. The mean white blood cell (WBC) count rose from a baseline level of 6.76 (± 1.76) × 109/L to 18.8 (± 4.46) × 109/L (P < .001) The median baseline PB CD34 count just before AMD3100 administration was 2/μL (range, 1-7/μL). At 4 hours after a single dose of AMD3100, the CD34 count rose to a median of 16/μL (range, 4-54/μL), representing a median 8-fold increase (Figure 1). In all donors, the PB CD34 count remained significantly above baseline through the end of the LP procedure. One of the 25 donors could not undergo LP following AMD3100 due to repeated vasovagal episodes during peripheral line placement prior to commencing LP (donor 14). A total of 8 (33%) of the remaining 24 donors who commenced LP following AMD3100 on day 1 did not collect the minimum required CD34+ cell dose in one day and were eligible for a second day of drug administration and LP on day 3. In the 7 donors that did undergo a second day of collection, the day 3 PB CD34+ count rose from a median baseline of 2/μL to 11/μL. The median 5.5-fold increase with the day-3 mobilization was higher than the 4-fold increase on day 1 observed in these donors. All but one collected the same or higher CD34+ cell dose compared with day 1. Another donor did not complete LP on day 1, asking to be taken off apheresis due to fatigue and diaphoresis (donor 10). The remaining 23 donors tolerated LP well. Of the 24 donors undergoing 1 or 2 days of LP following AMD3100, 2 did not achieve a minimum CD34+ dose of 2.0 × 106/kg, for a failure rate of 8.3%. One of these donors mobilized a 2-day total graft content just under the set minimum (1.9 × 106 CD34+ cells/kg). That graft was transplanted. The other donor's graft containing 1.2 × 106 CD34+ cells/kg was never transplanted, as his recipient's disease had progressed.
Change in peripheral blood CD34 count from baseline to 4 hours after a single injection of AMD3100 on day 1.
Change in peripheral blood CD34 count from baseline to 4 hours after a single injection of AMD3100 on day 1.
A total of 10 donors were eligible for a second round of mobilization after G-CSF, before the protocol amendment. Of these, 2 donors did not proceed to G-CSF mobilization, including the one donor who had asked to be removed from apheresis after AMD3100. The other donor was not mobilized with G-CSF because she had poor venous access and a central venous catheter would have been required to perform LP. This protocol exception was granted by the Washington University HSC.
The baseline PB CD34+ count was 3/μL (range, 1-8/μL) just before initiation of G-CSF; this rose to a median of 46/μL on day 5, representing a median 15.3-fold increase from baseline. This fold increase after 5 days of G-CSF was significantly greater then the rise 4 hours after AMD3100 (P < .001).
There were notable differences in the final LP products mobilized and collected after AMD3100 or G-CSF in the 8 donors who received both drugs (Table 2). There were significantly fewer CD34+ cells/kg (2.9 × 106 vs 4.2 × 106; P = .006), but greater numbers of CD3+ cells/kg (4.7 × 108 vs 1.5 × 108; P = .006) and CD4+ cells/kg (3.1 × 108 vs 1.1 × 108; P = .002) in the AMD3100-mobilized products compared with the G-CSF–mobilized allografts. The differences in CD3+ and CD4+ cell content remained significant even after excluding the donors who underwent 2 LP procedures after AMD3100. Thus, more CD3+ and CD4+ cells are mobilized per unit of blood following AMD3100 compared with G-CSF. However, the differences in CD8+, CD19+, and CD56+ cell content were not significant.
AMD3100 and G-CSF allograft content
| . | AMD3100 (N = 24), median (range) . | G-CSF (N = 8), median (range) . |
|---|---|---|
| CD34, × 106/kg | 2.9 (1.2-6.3) | 4.2 (2.5-18.7) |
| CD3, × 108/kg | 4.6 (1.5-7.8) | 1.3 (1.2-6.8) |
| CD4, × 108/kg | 3.2 (1-5.7) | 1.1 (0.7-3.2) |
| CD8, × 108/kg | 1.3 (0.4-3.4) | 0.4 (0.3-3.4) |
| CD19, × 108/kg | 1.0 (0.2-2.4) | ND |
| CD56, × 108/kg | 0.3 (0.1-1.0) | 0.2 (0.1-0.5) |
| . | AMD3100 (N = 24), median (range) . | G-CSF (N = 8), median (range) . |
|---|---|---|
| CD34, × 106/kg | 2.9 (1.2-6.3) | 4.2 (2.5-18.7) |
| CD3, × 108/kg | 4.6 (1.5-7.8) | 1.3 (1.2-6.8) |
| CD4, × 108/kg | 3.2 (1-5.7) | 1.1 (0.7-3.2) |
| CD8, × 108/kg | 1.3 (0.4-3.4) | 0.4 (0.3-3.4) |
| CD19, × 108/kg | 1.0 (0.2-2.4) | ND |
| CD56, × 108/kg | 0.3 (0.1-1.0) | 0.2 (0.1-0.5) |
All doses are reported as medians and ranges.
ND indicates not done.
In 4 donors, extensive T-cell phenotyping was performed on whole-blood samples collected prior to AMD3100 and 6 hours after the administration of AMD3100 using markers for naive, central memory, effector memory, and CD45RA-expressing effector memory phenotypes. As shown in Table 3, the percentages of each of these subsets within the CD4+ and CD8+ T-cell populations did not differ significantly between the pre-AMD3100 and 6-hour post-AMD3100 PB samples. Furthermore, the frequency of circulating CD4+CD25+Foxp3+ regulatory T cells was not altered after treatment with AMD3100. Therefore, AMD3100 induced a “panmobilization” of each T lymphocyte subset, with no apparent skewing toward a particular subset.
Phenotype of PB T lymphocytes before and after treatment with AMD3100
| Phenotype . | Before AMD3100, mean (± SD) . | 6 h after AMD3100, mean (± SD) . | P . |
|---|---|---|---|
| Total CD3+ count, × 103/mm3 | 1.61 ± 0.35 | 2.23 ± 0.46 | .003 |
| CD3+T lymphocyte populations, %* | |||
| CD4+CD8− | 64.3 ± 17.2 | 67.3 ± 9.5 | NS |
| CD4−CD8+ | 34.1 ± 16.8 | 30.3 ± 9.8 | NS |
| CD4+T lymphocyte subsets, %† | |||
| Naive (CD45RA+CD27+) | 38.7 ± 15.4 | 36.9 ± 16 | NS |
| Cells expressing CD62L, % | 81.8 ± 25 | 78.5 ± 30.1 | NS |
| TEMRA (CD45RA+CD27−) | 2.6 ± 3.3 | 2.0 ± 2.2 | NS |
| Cells expressing CD62L, % | 32 ± 11.4 | 34.3 ± 12.6 | NS |
| TCM (CD45RA−CD27+CD62L+) | 31.4 ± 9.2 | 32.3 ± 9.6 | NS |
| TEMI (CD45RA−CD27+CD62L−) | 18.7 ± 7.7 | 20.9 ± 9.9 | NS |
| TEMII (CD45RA−CD27−) | 8.7 ± 6.6 | 7.9 ± 4.4 | NS |
| Cells expressing CD62L, % | 24.4 ± 10.8 | 23.3 ± 12.2 | NS |
| Treg (FOXP3+CD25+) | 4.6 ± 1.4 | 4.6 ± 1.6 | NS |
| CD8+T lymphocyte subsets, %† | |||
| Naive (CD45RA+CD27+) | 34.4 ± 12.1 | 40.4 ± 11.5 | NS |
| Cells expressing CD62L, % | 62.4 ± 30.3 | 70.5 ± 34.5 | NS |
| TEMRA (CD45RA+CD27−) | 12.5 ± 9 | 8.4 ± 6.2 | NS |
| Cells expressing CD62L, % | 32.4 ± 11.5 | 42.5 ± 18.1 | NS |
| TCM (CD45RA−CD27+CD62L+) | 16.4 ± 8 | 18.8 ± 6 | NS |
| TEMI (CD45RA−CD27+CD62L−) | 29.4 ± 16 | 27.1 ± 12.5 | NS |
| TEMII (CD45RA−CD27−) | 7.3 ± 3.8 | 5.4 ± 3.4 | NS |
| Cells expressing CD62L, % | 26 ± 13.8 | 32.9 ± 8.9 | NS |
| Phenotype . | Before AMD3100, mean (± SD) . | 6 h after AMD3100, mean (± SD) . | P . |
|---|---|---|---|
| Total CD3+ count, × 103/mm3 | 1.61 ± 0.35 | 2.23 ± 0.46 | .003 |
| CD3+T lymphocyte populations, %* | |||
| CD4+CD8− | 64.3 ± 17.2 | 67.3 ± 9.5 | NS |
| CD4−CD8+ | 34.1 ± 16.8 | 30.3 ± 9.8 | NS |
| CD4+T lymphocyte subsets, %† | |||
| Naive (CD45RA+CD27+) | 38.7 ± 15.4 | 36.9 ± 16 | NS |
| Cells expressing CD62L, % | 81.8 ± 25 | 78.5 ± 30.1 | NS |
| TEMRA (CD45RA+CD27−) | 2.6 ± 3.3 | 2.0 ± 2.2 | NS |
| Cells expressing CD62L, % | 32 ± 11.4 | 34.3 ± 12.6 | NS |
| TCM (CD45RA−CD27+CD62L+) | 31.4 ± 9.2 | 32.3 ± 9.6 | NS |
| TEMI (CD45RA−CD27+CD62L−) | 18.7 ± 7.7 | 20.9 ± 9.9 | NS |
| TEMII (CD45RA−CD27−) | 8.7 ± 6.6 | 7.9 ± 4.4 | NS |
| Cells expressing CD62L, % | 24.4 ± 10.8 | 23.3 ± 12.2 | NS |
| Treg (FOXP3+CD25+) | 4.6 ± 1.4 | 4.6 ± 1.6 | NS |
| CD8+T lymphocyte subsets, %† | |||
| Naive (CD45RA+CD27+) | 34.4 ± 12.1 | 40.4 ± 11.5 | NS |
| Cells expressing CD62L, % | 62.4 ± 30.3 | 70.5 ± 34.5 | NS |
| TEMRA (CD45RA+CD27−) | 12.5 ± 9 | 8.4 ± 6.2 | NS |
| Cells expressing CD62L, % | 32.4 ± 11.5 | 42.5 ± 18.1 | NS |
| TCM (CD45RA−CD27+CD62L+) | 16.4 ± 8 | 18.8 ± 6 | NS |
| TEMI (CD45RA−CD27+CD62L−) | 29.4 ± 16 | 27.1 ± 12.5 | NS |
| TEMII (CD45RA−CD27−) | 7.3 ± 3.8 | 5.4 ± 3.4 | NS |
| Cells expressing CD62L, % | 26 ± 13.8 | 32.9 ± 8.9 | NS |
TEMRA, CD45RA-expressing effector memory T cells; TCM, central memory T cells; TEMI, effector memory type I T cells; TEMII, effector memory type II T cells; Treg, regulatory T cell; and NS, not significant.
As a percentage of the total CD3+ T lymphocyte population.
As a percentage of the total CD4+ or CD8+ T lymphocyte population.
Toxicity in donors following AMD3100
Most donors experienced some adverse effects immediately after or within a few hours of AMD3100 administration, but none were greater than grade 1 (mild), with the exception of one donor who experienced grade 2 pain at the injection site. The most common grade 1 toxicities included lightheadedness (44%); nausea, bloating, or flatulence (36%); injection site discomfort or warm sensation (28%); perioral paresthesias, loose stools, or diaphoresis (20%); and headache (16%). These toxicities typically resolved in a few hours and did not require any intervention. There were no cardiac toxicities observed. In the donors that received a second day of AMD3100, there was no evidence of cumulative or more severe toxicity. Most of the donors who received G-CSF experienced grade 1 or 2 bone pain that resolved shortly after cessation. CBCs and donor symptoms had returned to baseline in all donors at a 30-day post–AMD3100 injection follow-up. No long-term toxicities have been observed in any of the donors.
Hematopoietic engraftment and chimerism
A total of 20 patients received allografts mobilized after AMD3100 alone on day 0. A total of 5 of the 25 patients enrolled did not proceed on study due to progressive disease during donor collection (2 patients), because their donors did not tolerate LP (2 patients), and due to a low cardiac ejection fraction (1 patient). One of these 5 (patient no. 3) was the recipient for a donor who mobilized a CD34+ cell dose of only 1.2 × 106/kg after AMD3100. The allografts that were transplanted contained a median CD34+ cell dose of 2.9 × 106/kg before cryopreservation. The median viability of cells contained within the allografts after thaw was 98% (range, 88%-99%). No assessment of postthaw viability on isolated CD34+ or CD3+ cells was performed. All 20 patients engrafted neutrophils and platelets promptly. The median time to ANC greater than 0.5 × 109/L (500/μL) was 10 days (range, 8-13 days). The median times to platelet counts greater than 20 and 50 × 109/L (20 000 and 50 000/μL) were 12 days (range, 8-32 days) and 18 days (range, 12-32 days), respectively. We compared the engraftment kinetics after transplantation of AMD3100-mobilized allografts to a historical group of recipients at Washington University given G-CSF–mobilized allografts containing a median CD34+ cell dose of 8.2 × 106/kg. This historical group has been previously reported and received the exact same conditioning regimen and supportive care as the recipients enrolled on the current trial.20 There was no difference in the median time to neutrophil or platelet engraftment between recipients in the AMD3100 group or the historical group receiving G-CSF–mobilized allografts.
Donor chimerism in each patient was 95% to 100% in whole bone marrow as well as the CD3+ and CD15+ cell compartments within the PB at all times analyzed. All surviving patients in remission continue to have robust and durable trilineage hematopoiesis and are transfusion free (Table 3).
GVHD
All 20 patients engrafted and were therefore evaluable for acute GVHD. A total of 15 patients developed clinical evidence of acute GVHD; 8 had grade 1 (cutaneous) only. Only one patient developed severe (grade 4) acute GVHD. None developed grade 3 acute GVHD. The cumulative incidence of grade 2 to 4 acute GVHD was 35% (95% confidence interval [CI]: 16% to 64%; Figure 2A). The skin was involved frequently, but only 2 patients had involvement of the gastrointestinal (GI) tract or liver. All patients with the exception of the patient with grade 4 acute GVHD responded completely to topical or systemic corticosteroids.
Cumulative incidence of GVHD. (A) Cumulative incidence of grades 2 to 4 acute GVHD. (B) Cumulative incidence of extensive chronic GVHD.
Cumulative incidence of GVHD. (A) Cumulative incidence of grades 2 to 4 acute GVHD. (B) Cumulative incidence of extensive chronic GVHD.
A total of 4 patients relapsed before day 100, and 2 died from relapse. The 2 others received additional treatment. One additional patient died from complications secondary to acute GVHD before day 100. These 5 were not evaluable for chronic GVHD. Of the 15 patients evaluable for chronic GVHD, 6 developed extensive chronic GVHD requiring systemic steroids. Of these patients, 4 still have active chronic GVHD requiring ongoing immunosuppression. The cumulative incidence of chronic GVHD at 1 year was 33% (95% CI: 16% to 68%; Figure 2B).
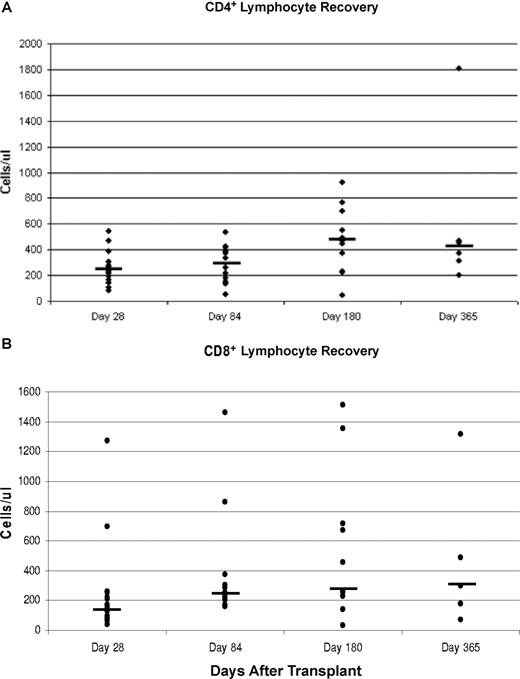
Immune reconstitution
We followed reconstitution of total CD3, CD3+CD4+, and CD3+CD8+ T cells within the PB of patients at days 28, 84, 180, and 365 after transplantation. Interestingly, median CD3+CD4+ cell counts were greater than 200/μL at all times evaluated, including as early as day 28. The median CD3+CD4+ cell counts were 244/μL (range, 82-543/μL) at day 28, 353/μL (range, 136-533/μL) at day 84, 471/μL (range, 42-921/μL) at day 180, and 414/μL (range, 198-1806/μL) at day 365. These were generally higher than the CD3+CD8+ counts at each time point analyzed, and most patients maintained a CD4/CD8 ratio greater than 1.0 throughout the period of observation (Figure 3).
Peripheral blood recovery. (A) Peripheral blood CD4+ cell recovery at days 28, 84, 180, and 365 after transplantation. (B) Peripheral blood CD8+ cell recovery at days 28, 84, 180, and 365 after transplantation. Horizontal bars represent median values.
Peripheral blood recovery. (A) Peripheral blood CD4+ cell recovery at days 28, 84, 180, and 365 after transplantation. (B) Peripheral blood CD8+ cell recovery at days 28, 84, 180, and 365 after transplantation. Horizontal bars represent median values.
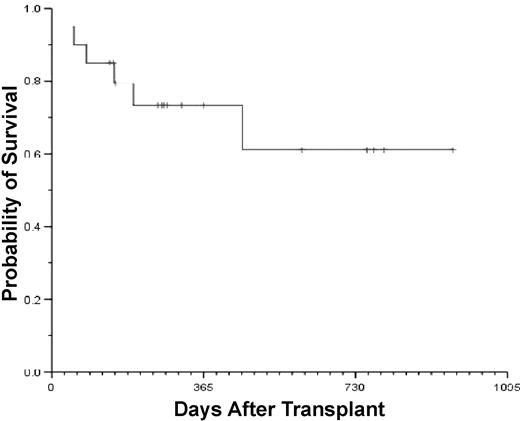
Relapse and survival
A total of 5 patients have relapsed between 47 and 257 days after transplantation (Table 4). One patient with AML underwent transplantation in second complete remission (CR2), relapsed at day 257 after transplantation, and was treated at that time with further chemotherapy. He is currently in a third complete remission with full donor chimerism at day 757. The other 4 have died from progressive disease. A total of 14 of 20 patients are surviving at a median follow-up of 277 days (range, 52-964 days). The Kaplan-Meier estimate of overall survival for the entire group at 1 year is 73% (95% CI: 63% to 87%; Figure 4). A total of 4 patients died from progressive disease, one died from refractory acute GVHD, and one died from Pneumocystis jiroveci pneumonia and chronic GVHD (Table 4).
Clinical outcomes
| Patient No. . | Age, y/sex, M/F . | Diagnosis/stage . | CD34 . | CD3 . | Day . | Survival, d . | Notes . | ||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| After A . | After G . | After A . | After G . | ANC more than 50 × 109/L . | Plt more than 20 × 109/L . | Plt more than 50 × 109/L . | |||||
| 1 | 51F | AML/CR2 | 2.6 | 2.9 | 4.9 | 1.3 | 11 | 14 | 21 | 964+ | |
| 2 | 54/M | ALL/Rel | 2.1 | 5.7 | 1.5 | 1.3 | NT | NT | NT | NT | |
| 3 | 50/M | AML/Rel | 1.2 | 2.5 | 2.7 | 6.8 | NT | NT | NT | NT | |
| 4 | 46/F | NHL/Rel | 2.5 | 2.8 | 6.8 | 1.2 | 11 | 20 | 25 | 774+ | |
| 5 | 31/M | AML/CR1 | 3.1 | 3.3 | 5.7 | 2.2 | 8 | 10 | 17 | 798+ | |
| 6 | 45/M | AML/Rel | 5.1 | NC | 1.9 | NC | 10 | 9 | 19 | 757+ | Alive in CR3 |
| 7 | 52/F | ALL/CR1 | 6.3 | 18.7 | 4.3 | 1.7 | 9 | 11 | 18 | 601+ | |
| 8 | 53/M | CML/AP | 2 | 5.0 | 3.8 | 1.2 | 13 | 32 | NR | 53 | Died; COD: GVHD |
| 9 | 37/F | NHL/Ref | 5.5 | 16.9 | 7.8 | 4.1 | 8 | 8 | 15 | 458 | Died; COD: pneumonia |
| 10 | 57/F | CLL/Rel | 1.5 | NC | 3 | NC | NT | NT | NT | NT | |
| 11 | 50/F | CLL/Ref | 1.9 | NC | 3.8 | NC | 10 | 15 | 18 | 196 | Died; COD: PD |
| 12 | 42/M | NHL/Ref | 2.9 | NC | 7.1 | NC | 11 | 13 | 17 | 365+ | |
| 13 | 59/F | AML/CR1 | 3.7 | NC | 3.7 | NC | 9 | 14 | 31 | 312+ | |
| 14 | 56/M | NHL/Rel | NC | NC | NC | NC | NT | NT | NT | NT | |
| 15 | 56/F | NHL/Ref | 4.1 | NC | 4.5 | NC | 8 | 12 | 12 | 83 | Died; COD: PD |
| 16 | 60/M | AML/Ref | 2.9 | NC | 6.2 | NC | 10 | 16 | 19 | 277+ | |
| 17 | 62/M | ALL/Rel | 2.3 | NC | 6.7 | NC | 10 | 11 | 21 | 270+ | |
| 18 | 55/F | ALL/CR1 | 2.1 | NC | 5.9 | NC | 9 | 10 | 17 | 265+ | |
| 19 | 34/M | AML/Rel | 3.7 | NC | 4.7 | NC | 5 | 22 | 25 | 255+ | |
| 20 | 53/F | NHL/Ref | 3.1 | NC | 6.7 | NC | 10 | 9 | 13 | 150 | Died; COD: PD |
| 21 | 62/F | MDS/RAEB | 3.2 | NC | 7.7 | NC | 9 | 11 | 15 | 153+ | |
| 22 | 40/F | AML/CR1 | 2.8 | NC | 2.6 | NC | 9 | 12 | 14 | 148+ | |
| 23 | 53/F | AML/Rel | 3.1 | NC | 5.8 | NC | NT | NT | NT | NT | |
| 24 | 51/F | CLL/Rel | 2.3 | NC | 2.8 | NC | 10 | 12 | 16 | 139+ | |
| 25 | 65/F | AML/Rel | 2.1 | NC | 4.5 | NC | 10 | 12 | 25 | 52 | Died; COD: PD |
| Patient No. . | Age, y/sex, M/F . | Diagnosis/stage . | CD34 . | CD3 . | Day . | Survival, d . | Notes . | ||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| After A . | After G . | After A . | After G . | ANC more than 50 × 109/L . | Plt more than 20 × 109/L . | Plt more than 50 × 109/L . | |||||
| 1 | 51F | AML/CR2 | 2.6 | 2.9 | 4.9 | 1.3 | 11 | 14 | 21 | 964+ | |
| 2 | 54/M | ALL/Rel | 2.1 | 5.7 | 1.5 | 1.3 | NT | NT | NT | NT | |
| 3 | 50/M | AML/Rel | 1.2 | 2.5 | 2.7 | 6.8 | NT | NT | NT | NT | |
| 4 | 46/F | NHL/Rel | 2.5 | 2.8 | 6.8 | 1.2 | 11 | 20 | 25 | 774+ | |
| 5 | 31/M | AML/CR1 | 3.1 | 3.3 | 5.7 | 2.2 | 8 | 10 | 17 | 798+ | |
| 6 | 45/M | AML/Rel | 5.1 | NC | 1.9 | NC | 10 | 9 | 19 | 757+ | Alive in CR3 |
| 7 | 52/F | ALL/CR1 | 6.3 | 18.7 | 4.3 | 1.7 | 9 | 11 | 18 | 601+ | |
| 8 | 53/M | CML/AP | 2 | 5.0 | 3.8 | 1.2 | 13 | 32 | NR | 53 | Died; COD: GVHD |
| 9 | 37/F | NHL/Ref | 5.5 | 16.9 | 7.8 | 4.1 | 8 | 8 | 15 | 458 | Died; COD: pneumonia |
| 10 | 57/F | CLL/Rel | 1.5 | NC | 3 | NC | NT | NT | NT | NT | |
| 11 | 50/F | CLL/Ref | 1.9 | NC | 3.8 | NC | 10 | 15 | 18 | 196 | Died; COD: PD |
| 12 | 42/M | NHL/Ref | 2.9 | NC | 7.1 | NC | 11 | 13 | 17 | 365+ | |
| 13 | 59/F | AML/CR1 | 3.7 | NC | 3.7 | NC | 9 | 14 | 31 | 312+ | |
| 14 | 56/M | NHL/Rel | NC | NC | NC | NC | NT | NT | NT | NT | |
| 15 | 56/F | NHL/Ref | 4.1 | NC | 4.5 | NC | 8 | 12 | 12 | 83 | Died; COD: PD |
| 16 | 60/M | AML/Ref | 2.9 | NC | 6.2 | NC | 10 | 16 | 19 | 277+ | |
| 17 | 62/M | ALL/Rel | 2.3 | NC | 6.7 | NC | 10 | 11 | 21 | 270+ | |
| 18 | 55/F | ALL/CR1 | 2.1 | NC | 5.9 | NC | 9 | 10 | 17 | 265+ | |
| 19 | 34/M | AML/Rel | 3.7 | NC | 4.7 | NC | 5 | 22 | 25 | 255+ | |
| 20 | 53/F | NHL/Ref | 3.1 | NC | 6.7 | NC | 10 | 9 | 13 | 150 | Died; COD: PD |
| 21 | 62/F | MDS/RAEB | 3.2 | NC | 7.7 | NC | 9 | 11 | 15 | 153+ | |
| 22 | 40/F | AML/CR1 | 2.8 | NC | 2.6 | NC | 9 | 12 | 14 | 148+ | |
| 23 | 53/F | AML/Rel | 3.1 | NC | 5.8 | NC | NT | NT | NT | NT | |
| 24 | 51/F | CLL/Rel | 2.3 | NC | 2.8 | NC | 10 | 12 | 16 | 139+ | |
| 25 | 65/F | AML/Rel | 2.1 | NC | 4.5 | NC | 10 | 12 | 25 | 52 | Died; COD: PD |
Plt indicates platelet count; CR, complete remission; Rel, relapsed; Ref, refractory; A, AMD3100; G, G-CSF; RAEB, refractory anemia with excess blasts; NT, never received transplant; NC, not collected; NR, not reached CR3, third complete remission; COD, cause of death; PD, progressive disease; and NE, not evaluable.
Discussion
The results of this trial support the hypothesis that directly targeting the interaction between CXCR4 and SDF-1/CXCL12 is an effective strategy to reduce the length of time required to procure a functional HLA-matched sibling donor hematopoietic allograft. In two-thirds of the donors, a single injection of AMD3100 just 4 hours after its administration induced the mobilization of sufficient numbers of HSPCs to reconstitute durable trilineage hematopoiesis. This is in contrast to the 4 to 5 days of G-CSF administration typically required to procure an adequate number of HSPCs for transplantation. Importantly, AMD3100 appeared to be at least as safe as G-CSF in the short term, because no donor experienced more than grade 1 toxicity. In addition, no donors experienced any bone pain, which is typically associated with G-CSF administration.3 Donors experienced no long-term consequences with at least a median follow-up of 9 months after donation. Longer follow-up and greater numbers of donors will be needed to assess the overall safety of AMD3100 in this setting.
Both in vitro and in vivo experiments have recently suggested that G-CSF induces HSPC mobilization by indirectly disrupting the interaction between CXCR4 and SDF-1.7,11,25,26 This requires several days for maximal effect. By directly targeting this interaction, AMD3100 induces rapid HSPC egress from the bone marrow and possibly other niches within just a few hours.10,13,14,16 Previous kinetic studies in healthy volunteers and patients demonstrated the peak effect of AMD3100 on CD34+ cell mobilization occurs approximately 9 to 10 hours after a single injection.13 In our trial, we chose to begin LP within 4 hours of AMD3100 for several reasons. First, a prior study by Liles and colleagues suggested that adequate numbers of CD34+ cells were mobilized as soon as 3 hours after injection, making collection feasible after just a few hours.13 Because we were using the agent in healthy donors, we wanted to observe the donors in clinic directly for any adverse effects. Further, the schedule we chose would render the entire mobilization and collection process feasible within 1 working day, making it significantly more manageable for both donors and staff. It is likely that the allografts would have contained a greater quantity of CD34+ cells if LP was begun 6 hours after AMD3100, which was closer to the peak of mobilization in donors as demonstrated by Liles and colleagues.27
The doses of CD34+ cells contained within the allografts collected after AMD3100 were significantly lower than what would be expected in LP products collected after 5 days of G-CSF treatment, as demonstrated in the 8 donors that received both agents (Table 2). These differences were to some degree due to the short interval between drug injection and LP, but the grafts would likely have contained fewer CD34+ cells compared with G-CSF–mobilized allografts even using the optimal (6-hour) dosing interval. Notwithstanding, the AMD3100-mobilized allografts functioned well and promoted rapid and durable trilineage hematopoiesis. This suggests the possibility of qualitative as well as quantitative differences among grafts collected following these 2 agents. In fact, recent studies in both mice and nonhuman primates suggest that grafts mobilized after AMD3100 are enriched for long-term repopulating cells compared with G-CSF.10,28,29 Whether this will result in any long-term functional consequences such as better immunologic reconstitution cannot be answered by our trial. However, taken together, the results of our small trial combined with recent insights in animal models suggest that direct comparisons between AMD3100- and G-CSF–mobilized allografts considering only the quantity of CD34+ cells as a measure of graft quality may not be appropriate. Further study in this regard is warranted, and longer follow-up will be necessary to assess graft durability.
Another potentially important difference between AMD3100- and G-CSF–mobilized allografts is the quantity and function of T cells mobilized by both agents. We observed roughly 2-fold higher numbers of CD3+ and CD4+ cells contained within the AMD3100-mobilized allografts compared with G-CSF–mobilized allografts. Of immediate concern was the potential for a greater risk of either acute or chronic GVHD due to the higher numbers of T cells transplanted with AMD3100-mobilized allografts. Although our trial was not designed for this comparison, the rates of acute and chronic GVHD we observed in the first 20 recipients were not significantly different compared with historical control patients at Washington University receiving G-CSF–mobilized allografts together with the exact same conditioning and GVHD prophylaxis.19,20 It is possible there may be functional differences in addition to the numerical differences noted. Data we have generated in mice do not suggest this, and preliminary flow cytometric analysis of T-cell subsets in a small sample of 4 donors did not demonstrate any prominent skewing of T-cell subsets toward a regulatory T-cell or activated T-cell phenotype after AMD3100.30 Some may argue that the cryopreservation of the AMD3100-mobilized allografts before transplantation could have downmodulated the potential alloreactivity of the T cells within the grafts, but the preponderance of clinical evidence does not support this contention.31 Alternatively, the higher numbers of mature T cells mobilized by AMD3100 may enhance immune reconstitution after transplantation, as suggested by the relatively rapid recovery of CD4 and CD8 counts observed in our patients. Nevertheless, it will be important to follow this distinction as future trials go forward, and more patients will need to be treated to assess for any differences in the risk of GVHD.
In summary, these preliminary data demonstrate that the length of time required to mobilize and procure a functional hematopoietic allograft can be reduced from a 5-day to a 1-day process by directly targeting the interaction between the chemokine receptor CXCR4 and its ligand SDF-1/CXCL12. Allografts mobilized just 4 hours after AMD3100 differ in the content of CD34+ and CD3+ cells compared with allografts mobilized after 5 days of G-CSF, yet function similarly. While this novel mobilization regimen requires optimization, these data suggest that mobilizing HLA-matched sibling donors by directly targeting CXCR4/SDF-1 may be an effective and possibly less toxic and cumbersome alternative to the traditional method of mobilizing donors with G-CSF.
An Inside Blood analysis of this article appears at the front of this issue.
Presented in part at an oral simultaneous session of the 48th Annual Meeting and Exposition of the American Society of Hematology, Orlando, FL, December 11, 2006.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 USC section 1734.
Acknowledgments
This study was supported in part by research funding from The Barnes Jewish Foundation (St Louis, MO) and Genzyme Corporation (Cambridge, MA) to S.M.D., J.F.D., and D.L.
Authorship
Contribution: R.V., M.R., and P.W. performed research and edited the manuscript; D.L. designed research and edited the manuscript; G.C. and G.B. analyzed and interpreted data and edited the manuscript; L.T., K.M., and N.F. collected data; and S.M.D. and J.F.D. designed and performed research, analyzed and interpreted data, performed statistical analysis, and drafted the manuscript.
Conflict-of-interest disclosure: G.C. and G.B. are employees of Genzyme Corporation and have stock ownership in that company. All other authors declare no competing financial interests.
Correspondence: Steven M. Devine, B316 Starling-Loving Hall, 320 West 10th Avenue, Columbus, OH 43210; e-mail: steven.devine@osumc.edu.