Abstract
Improving the potency of immune responses is paramount among issues concerning vaccines against deadly pathogens. IL-28B belongs to the newly described interferon lambda (IFNλ) family of cytokines, and has not yet been assessed for its potential ability to influence adaptive immune responses or act as a vaccine adjuvant. We compared the ability of plasmid-encoded IL-28B to boost immune responses to a multiclade consensus HIV Gag plasmid during DNA vaccination with that of IL-12. We show here that IL-28B, like IL-12, is capable of robustly enhancing adaptive immunity. Moreover, we describe for the first time how IL-28B reduces regulatory T-cell populations during DNA vaccination, whereas IL-12 increases this cellular subset. We also show that IL-28B, unlike IL-12, is able to increase the percentage of splenic CD8+ T cells in vaccinated animals, and that these cells are more granular and have higher antigen-specific cytolytic degranulation compared with cells taken from animals that received IL-12 as an adjuvant. Lastly, we report that IL-28B can induce 100% protection from mortality after a lethal influenza challenge. These data suggest that IL-28B is a strong candidate for further studies of vaccine or immunotherapy protocols.
Introduction
Having a comprehensive understanding of the immune system and its components is critical not only for understanding host-pathogen interactions during infections, but also in the context of vaccine development and design. In regard to immune-associated signaling compounds, such as cytokines, vaccination studies may additionally give us a means by which to study how these molecules affect antigen-specific immune responses
DNA vaccination is a safe and effective method of inducing antigen-specific immune responses in vivo1-3 that lends itself to the introduction of immune modulators. The ability to easily add plasmids encoding cytokines into DNA vaccination platforms allows for the simultaneous assessment of how a cytokine may influence adaptive immune responses as well as determining its potential value as a vaccine adjuvant. Furthermore, recent data in nonhuman primates with optimized DNA formulations are showing more promising immune profiles. Improving on these encouraging results is an important goal.
The interferon λ family consists of 3 recently discovered cytokines: IL-29, IL-28A, and IL-28B (IFNλ 1, 2, and 3, respectively).4-7 All 3 cytokines have been shown to be expressed in response to viral infections in vitro, and are secreted primarily by dendritic cells and macrophages.4-7 In addition, all 3 cytokines are classified as interferons because treatment of cells with these cytokines can induce an antiviral state that inhibits viral replication in culture, as a result of STAT, IRF, and ISGF activation through the IL-28 receptor.4-7 Although receptor expression has been shown on a variety of leukocytes, including T lymphocytes,8 the relative ability of IL-28 to shape antigen-specific adaptive immune responses has not been extensively studied to this point.
In this study, we have analyzed the ability of IL-28B to act as an adjuvant in a DNA vaccination setting, and compared its ability to augment immune responses with that of IL-12, which is a potent and perhaps best established DNA immunoadjuvant.9-13 In doing so, we have characterized the impact of IL-28B on the antigen-specific adaptive immune response, which has not yet been studied. The inclusion of plasmid-encoded IL-28B or IL-12 led to increased antigen-specific cellular immune responses over vaccination with antigen alone, as gauged by IFNγ enzyme-linked immunosorbent spot (ELISpot) and detection of perforin by flow cytometry. IL-28B, but not IL-12, was further able to increase antigen-specific IgG2a, antigen-specific cytolytic degranulation, and the percentage of CD8+ T cells found in the spleen. In addition, we found that the IL-28B adjuvant reduced the number of CD4+/CD25hi/FoxP3+ cells (Tregs) found in the spleens of vaccinated animals, whereas IL-12 increased the size of this population. Lastly, we show here, when used as an adjuvant for vaccination in mice, IL-28B is able to augment immune responses in such a fashion as to result in 100% protection from death after a lethal influenza challenge. This study shows that IL-28B may act as an effective adjuvant for cellular immunity in vivo and is the first to describe the differential effects of IL-28B and IL-12 on Treg populations after DNA vaccination. This constitutes the first major analysis of the ability of IL-28B to shape adaptive immune responses in vivo.
Methods
Plasmids
The IL-12 plasmid encoding murine p35 and p40 proteins has been described.11,14 Murine IL-28B had a high efficiency leader sequence added to the 5′ end of the gene and was synthesized, codon optimized, and subsequently subcloned into the pVAX1 backbone by GeneArt (Renensberg, Germany). Plasmids expressing HIV-1 Gag (Gag4Y) were prepared as previously described.15
Animals
All animals were housed in a temperature-controlled, light-cycled facility at the University of Pennsylvania, and their care was under the guidelines of the National Institutes of Health (NIH, Bethesda, MD) and the University of Pennsylvania. All animal experiments were performed in accordance with national and institutional guidelines for animal care and were approved by the institutional review board of the University of Pennsylvania.
Immunization of mice
The quadriceps muscle of 8-week-old female BALB/c mice (The Jackson Laboratory, Bar Harbor, ME) were injected 2 times, 2 weeks apart, and electroporated as previously described16 using the CELLECTRA adaptive constant current device (VGX Pharmaceuticals, The Woodlands, TX). For experiments in mice, the animals (n = 4 or 8 per group) were immunized with either 10 μg pVAX1 or 10 μg HIV-1 Gag (Gag4Y) or influenza NP (NP) alone or with various amounts of murine IL-12 or murine IL-28B plasmid, depending on the experiment. Coadministration of various gene plasmids involved mixing the designated DNA plasmids before injection in 0.25% bupivicaine-HCL (Sigma-Aldrich, St Louis, MO) in isotonic citrate buffer to a final volume of 30 μL.
ELISpot
Both IFN-γ and IL-4 ELISpot was performed to determine antigen-specific cytokine secretion from immunized mice. ELISpots were carried out per the manufacturer's protocols (R&D Systems, Minneapolis, MN) using 96-well plates (Millipore, Billerica, MA). Splenocytes (2 × 105) from immunized mice were added to each well of the plate and stimulated overnight at 37°C, 5% CO2, in the presence of R10 (negative control), concanavalin A (positive control), or specific peptide (HIV-1 Gag) antigens (10 μg/mL). HIV-1 Consensus Gag Clade C 15-mer peptides spanning the entire protein, overlapping by 11 amino acids, were acquired from the AIDS Reagent and Reference Repository (Frederick, MD).
Cell culture and staining for flow cytometry
Splenocytes harvested from immunized mice were washed and then resuspended with R10 media to a final concentration of 107 cells/mL. Cells were seeded into 96-well plates in a volume of 100 μL, and an additional 100 μL media alone (negative control), media containing HIV-1 Gag Consensus Clade C peptides, or media containing PMA and ionomycin (positive control) was then added and plates were place at 37°C. In cultures being used to measure degranulation, anti-CD107a PE was added at this time as an enhanced stain. Cultures used to measure intracellular perforin levels did not receive this antibody. For these cultures, 10 minutes after the addition of media, peptide or PMA/ionomycin, Mg+2, and EGTA were added to cultures to a final concentration of 6 mM and 8 mM, respectively, to inhibit calcium-dependent cytolytic degranulation.17 All cultures were allowed to incubate at 37°C for 6 hours. At the end of this incubation period, plates were spun down and washed twice with PBS. Cells were then stained with a violet dye for viability (LIVE/DEAD Violet Viability Dye; Invitrogen, Frederick, MD) for 10 minutes at 37°C. After washing with PBS, cells were stained externally with anti-CD4 PerCPCy5.5 (BD Biosciences, San Jose, CA) and anti-CD8 APCCy7 (BD Biosciences) at 4°C, followed by fixing and permeabilization (Cytofix/Cytoperm Kit; BD Biosciences). Anti-CD3 PE-Cy5 (BD Biosciences) and antiperforin APC (eBioscience, San Diego, CA) were added and cells were incubated again at 4°C. Cells were given a final wash with PBS and fixed in PFA at a final concentration of 1%. For flow cytometry involving CD4+/CD25hi/FoxP3+ cells, the Mouse Regulatory T Cell staining kit was used (eBioscience). External staining was carried out with anti-CD4 FITC and anti-CD25 APC. Fixation, permeabilization, and internal staining were also carried out using anti-FoxP3 PE.
Influenza challenge
Twenty-eight days after immunization, anesthetized mice were intranasally inoculated with 10 LD50 of A/Puerto Rico/8/34 in 30 μL PBS.16 All murine challenge groups were composed of 8 mice per group. After challenge, clinical signs and mortality were recorded daily for 14 days.
Statistics
Data are presented as the mean plus or minus standard error of the mean (SE) calculated from data collected from at least 3 independent experiments. Where appropriate, the statistical difference between immunization groups was assessed using a paired Student t test and yielded a specific P value for each experimental group. Comparisons between samples with a P value less than .05 were considered statistically different and therefore significant.
Results
Plasmids encoding murine IL-12 and IL-28B express and secrete protein
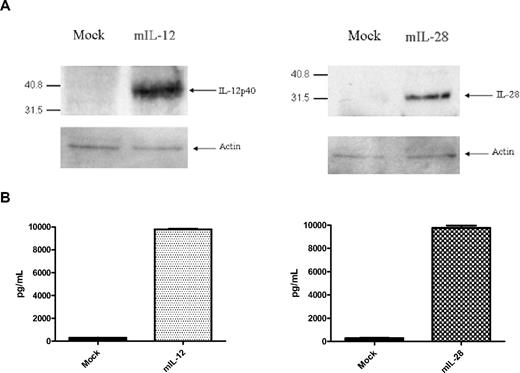
There is a constant need for discovery of new and improved adjuvants for vaccination against various viral pathogens. In the past, IL-12 has been shown to be a potent adjuvant when used in vaccination studies.9-13 IL-28B has not yet been used for this purpose. To compare the relative abilities of these cytokines to augment antigen-specific immune responses, we constructed plasmids encoding murine IL-1211 and murine IL-28B for use in our DNA vaccination studies (Figure 1A,B). To confirm whether these constructs expressed IL-12 and IL-28B, we tested them in vitro via transfection of HEK 293T cells with 3 μg plasmid. Cells were subsequently lysed and lysates were used in Western blots to test for protein expression. Blots for murine IL-12p40 and murine IL-28B proteins show that both constructs are expressed well in vitro (Figure 2A). To examine cytokine secretion to the extracellular environment, cell supernatants were obtained 48 hours after transfection. Enzyme-linked immunosorbent assays (ELISAs) to detect the active IL-12 p35/p40 heterodimer and the IL-28B protein from transfected cell culture supernatants were carried out. As shown in Figure 2B, IL-12 and IL-28B were both observed to be present at a concentration of roughly 10 000 pg/mL in transfected culture supernatants. Upon confirming the expression and release of both cytokines from transfected cells, we began vaccination studies to test the ability of these cytokines to adjuvant antigen-specific immune responses.
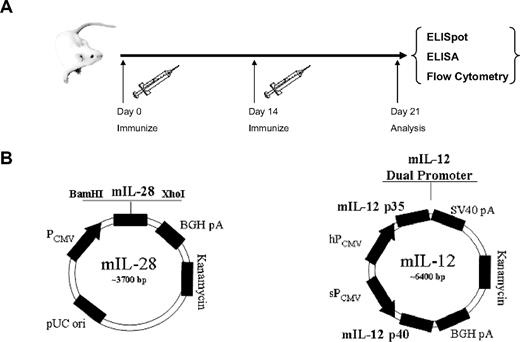
Immunization schedule and plasmid maps. (A) Mice were immunized on day 0 and day 14 with a multiclade HIV Gag construct and with or without adjuvant, followed by electroporation using the CELLECTRA adaptive constant current device after each immunization. On day 21, mice were killed and lymphocytes were isolated and analyzed. (B) Plasmid maps for murine IL-28B and IL-12 constructs.
Immunization schedule and plasmid maps. (A) Mice were immunized on day 0 and day 14 with a multiclade HIV Gag construct and with or without adjuvant, followed by electroporation using the CELLECTRA adaptive constant current device after each immunization. On day 21, mice were killed and lymphocytes were isolated and analyzed. (B) Plasmid maps for murine IL-28B and IL-12 constructs.
Expression and secretion of murine IL-12 and murine IL-28B in vitro. (A) Western blotting for murine IL-12p40 and murine IL-28 proteins from HEK 293T cell lysates 48 hours after transfection. Mock-transfected cells received empty pVAX vector. (B) ELISAs show secretion of the active IL-12 p35/p40 heterodimer as well as the IL-28 protein into the supernatants of transfected cells.
Expression and secretion of murine IL-12 and murine IL-28B in vitro. (A) Western blotting for murine IL-12p40 and murine IL-28 proteins from HEK 293T cell lysates 48 hours after transfection. Mock-transfected cells received empty pVAX vector. (B) ELISAs show secretion of the active IL-12 p35/p40 heterodimer as well as the IL-28 protein into the supernatants of transfected cells.
IL-28B adjuvants HIV Gag-specific IFNγ release after vaccination
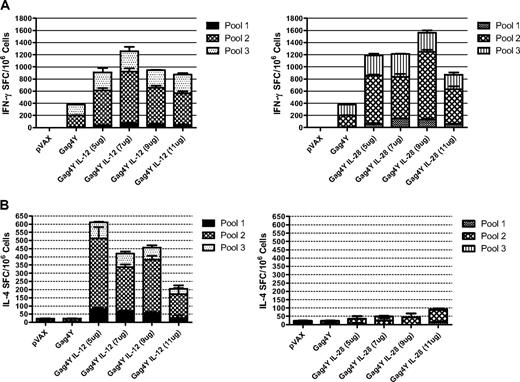
To determine whether IL-28B had the potential to function as an immunoadjuvant, we used it in DNA vaccination studies in combination with a plasmid encoding a multiclade consensus HIV-1 Gag protein (Gag4Y) as our target antigen. To have a measure of comparison of the potency of the adjuvant effects of IL-28B, we compared it with a cytokine that is frequently used as an adjuvant in vaccinations because it has previously been shown to have very potent immunoadjuvant effects: IL-12.9-13 To that end, groups of 8-week-old Balb/c mice (n = 4 per group) were immunized intramuscularly in the right rear quadriceps with 10 μg empty pVAX vector (control) or 10 μg HIV Gag4Y construct alone, followed by electroporation. Additional groups received 10 μg HIV Gag4Y in combination with either IL-28B or IL-12 at various doses, also followed by electroporation. Results of an IFNγ ELISpot assay show that although immunization with Gag4Y alone was able to induce a cellular immune response in the mice (∼ 400 SFU per million splenocytes), inclusion of IL-28B was able to further increase Gag-specific IFNγ release at all doses tested several fold (Figure 3A). Optimal adjuvant effects of IL-28B (3- to 4-fold over Gag4Y alone) were seen at a range of 7 to 9 μg (Figure 3A), leading us to use this dose for further experiments. IL-12 also increased Gag-specific IFNγ release in this assay by slightly more than 3-fold in the same range of doses as IL-28B (Figure 3A). Analysis of each assay showed that responses were mediated predominantly by CD8+ T cells (> 85% total response) and that this profile was not influenced by the presence or absence of adjuvant during vaccination (data not shown). These results suggest that IL-28B can, indeed, be used to bolster antigen-specific immune responses during vaccination, with increases in IFNγ release comparable or greater than those seen with IL-12, which is an established, potent immunoadjuvant.
HIV Gag-specific IFNγ and IL-4 ELISpots from isolated splenocytes. (A) Effects of cytokine adjuvants on the induction of a Th1 response were measured via the use antigen-specific IFNγ ELISpots performed on isolated splenocytes. ELISpots were performed on splenocytes harvested from mice that received IL-12 as an adjuvant or IL-28B as an adjuvant (n = 4) and IFNγ spot-forming units (SFU) were counted. (B) Effects of cytokine adjuvants on the induction of a Th2 response were measured in the same fashion using IL-4 ELISpots.
HIV Gag-specific IFNγ and IL-4 ELISpots from isolated splenocytes. (A) Effects of cytokine adjuvants on the induction of a Th1 response were measured via the use antigen-specific IFNγ ELISpots performed on isolated splenocytes. ELISpots were performed on splenocytes harvested from mice that received IL-12 as an adjuvant or IL-28B as an adjuvant (n = 4) and IFNγ spot-forming units (SFU) were counted. (B) Effects of cytokine adjuvants on the induction of a Th2 response were measured in the same fashion using IL-4 ELISpots.
Upon confirming that IL-28B could be used to increase the cellular immune response via increased release of the Th1-associated cytokine IFNγ, we next endeavored to determine whether this adjuvant could affect the release of a prototypical Th2 cytokine. Thus we used an IL-4 ELISpot to observe how IL-28B might be influencing the release of this Th2-associated cytokine. Interestingly, the inclusion of IL-12 in vaccination resulted in increases in Gag-specific IL-4 release at all doses tested, ranging from approximately 200 to 600 SFU (Figure 3B). The optimal doses for IL-12 in the IFNγ ELISpot assay resulted in approximately 400 to 450 SFU in the IL-4 ELISpot assay, whereas the inclusion of IL-28B did not show this type of effect. Instead, inclusion of IL-28B in vaccination resulted in IL-4 release that was quite similar to the HIV Gag4Y construct alone (Figure 3B), suggesting that IL-28B does not increase IL-4 release concomitant with increased IFNγ release at these doses. Thus, IL-28B may be thought of as inducing a more “pure” Th1-associated cytokine profile during vaccination compared with IL-12 in that it induces IFNγ (Th1-associated) release but not IL-4 (Th2-associated) release.
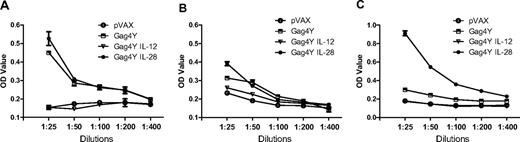
IL-28B but not IL-12 increases HIV Gag-specific IgG2a
As an effective vaccination against a viral pathogen may necessitate both a cellular and humoral immune response, we decided to examine the relative abilities of IL-28B and IL-12 to augment the level of circulating HIV Gag-specific antibodies when used as adjuvants during vaccination. To accomplish this, we tested sera taken from immunized mice in antigen-specific ELISAs. Inclusion of IL-12 or IL-28B in conjunction with the HIV Gag4Y construct resulted in markedly different antibody responses, as shown in Figure 4. In regard to total Gag-specific IgG, immunization with the Gag4Y construct together with the IL-28B construct led to a small increase in levels of antigen-specific antibodies compared with immunization with Gag4Y alone at the lowest dilution tested (1:25; Figure 4A). However, inclusion of IL-12 with Gag4Y immunization actively suppressed antigen-specific IgG, with values reading very similar to those of control (pVAX) mice. This effect of IL-12 is a phenomenon that has been reported previously in DNA vaccination,14 and is supported in the current study as well. We next examined different subtypes of IgG, including IgG1 and IgG2a, to determine additional effects on immune polarization. The IgG1 isotype is associated with Th2 skewing in mice, whereas IgG2a is associated with Th1 skewing.18 Regardless of the inclusion of adjuvant, DNA vaccination did not seem to augment Gag-specific IgG1 antibody levels in any group in our assay (Figure 4B). However, the inclusion of IL-28B in vaccination led to a greater than 2-fold increase in IgG2a compared with sera from mice vaccinated with HIV Gag4Y alone (Figure 4C). In addition, IL-12 continued to suppress antibody responses in this assay, as evidenced by the fact that no increase in IgG2a was seen in the IL-12 group compared with the control (pVAX) group. Thus IL-28B seems to be able to increase antigen-specific humoral immune responses in a heavily Th1-biased fashion, which is in agreement with its effect on the cellular immune response (Figure 3A,B).
HIV Gag-specific IgG in sera from vaccinated animals. Sera from control (pVAX) or immunized animals (n = 4) were assayed for the presence of HIV Gag-specific antibodies via ELISA 1 week after immunization. (A) Total IgG. (B) IgG1. (C) IgG2a.
HIV Gag-specific IgG in sera from vaccinated animals. Sera from control (pVAX) or immunized animals (n = 4) were assayed for the presence of HIV Gag-specific antibodies via ELISA 1 week after immunization. (A) Total IgG. (B) IgG1. (C) IgG2a.
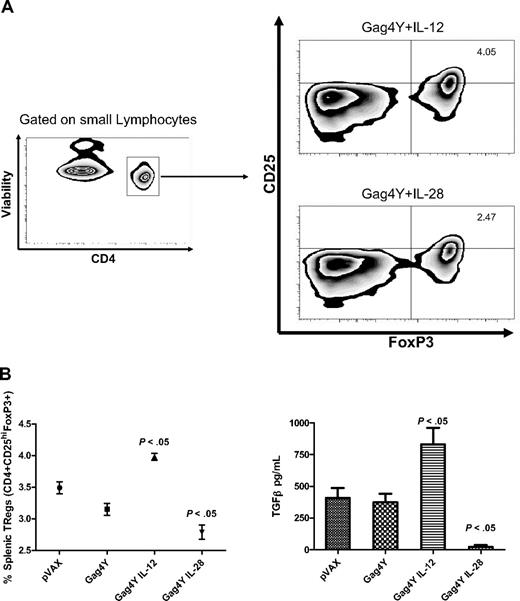
IL-28B decreases splenic CD4+/CD25hi/FoxP3+ cells, whereas IL-12 increases them
IL-28B is a member of the newly described IFNλ family, and thus is also known as IFNλ3.18-21 Other members of the IFNλ family include IL-28A (IFNλ2) and IL-29 (IFNλ1).18-21 A previous study has suggested that IL-29 may play a role in immune suppression and tolerance in that it may drive dendritic cells to specifically induce the proliferation of CD25hi/FoxP3+ CD4+ T cells (Tregs) in response to IL-2.5 The induction or expansion of Tregs could be considered a drawback to vaccination strategies within certain settings, and the ability of IL-28B to influence this subpopulation of CD4+ T cells has not previously been studied. As IL-28B falls into the same IFN family as IL-29, we addressed the possibility that it may exert similar effects on the Treg cell population. In addition, we looked at the ability of IL-12 to affect Tregs in this type of vaccination setting, which has not been previously examined.
By looking at the expression of CD4, CD25, and FoxP3 via flow cytometry (Figure 5A), we were able to study the impact of vaccination with and without cytokine adjuvants on Treg populations in immunized mice. The results of this analysis show that immunization with the HIV Gag4Y construct alone resulted in a small but not statistically significant decrease in the percentage of splenic Tregs from vaccinated mice (Figure 6B). This result is consistent with a previous report describing a similar change in Treg populations after vaccination.20 Inclusion of cytokine adjuvants in vaccination dramatically altered Treg populations in various fashions. Interestingly, the use of IL-12 as an immunoadjuvant significantly increased the number of splenic Tregs in immunized mice compared with mice vaccinated with the HIV Gag4Y construct alone (Figure 5B). This is the first time this phenomenon has been reported in a vaccination setting and may constitute a previously unrealized phenotype of IL-12 as an adjuvant for immunization. Also of considerable interest was the fact that the inclusion of IL-28B as an immunoadjuvant for vaccination caused a statistically significant decrease in the number of splenic Tregs compared with vaccination with HIV Gag4Y alone (Figure 5B). This is the first time this ability of IL-28B has been described and may be viewed as a significant benefit of this cytokine when it is used as an adjuvant for vaccination. Moreover, it suggests the possibility that although they are in the same IFN family, there may be key differences between IL-28B and IL-29.
Differential induction of regulatory T cells and TGFβ secretion during immunization. The presence of regulatory T cells (CD4+/CD25hi/FoxP3+) was assayed from isolated splenocytes from all groups (n = 4) via flow cytometry (A). Analysis of flow cytometry shows differences in Treg populations, whereas analysis of cytokine secretion from these cells shows differences in TGFβ release (B). P values reflect comparisons between mice vaccinated with Gag4Y alone with mice vaccinated with Gag4Y plus IL-12 or IL-28B.
Differential induction of regulatory T cells and TGFβ secretion during immunization. The presence of regulatory T cells (CD4+/CD25hi/FoxP3+) was assayed from isolated splenocytes from all groups (n = 4) via flow cytometry (A). Analysis of flow cytometry shows differences in Treg populations, whereas analysis of cytokine secretion from these cells shows differences in TGFβ release (B). P values reflect comparisons between mice vaccinated with Gag4Y alone with mice vaccinated with Gag4Y plus IL-12 or IL-28B.
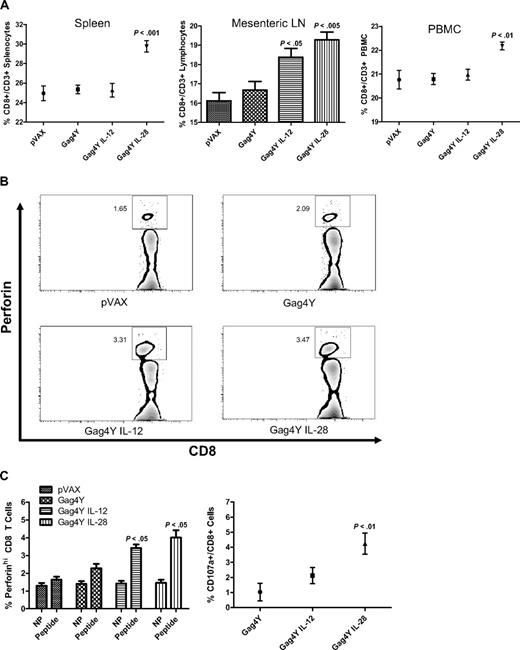
Changes in CD8+ T-cell populations, granularity, and degranulation. The percentage of CD8+ T cells (CD3+/CD8+) was assessed via flow cytometry in the blood, spleen, and mesenteric lymph nodes (A). Antigen-specific induction of perforin in CD8+ T cells was analyzed by flow cytometry via comparison of unstimulated cells (NP) with cells stimulated with HIV Gag peptides (Peptide). Results from a single experiment are shown (B) and averages for all experiments are graphed (C). Antigen-specific cytolytic degranulation was measured via stimulation with peptide in the presence of an antibody to CD107a, followed by analysis using flow cytometry (C). P values reflect comparisons between mice vaccinated with Gag4Y alone with mice vaccinated with Gag4Y plus IL-12 or IL-28B.
Changes in CD8+ T-cell populations, granularity, and degranulation. The percentage of CD8+ T cells (CD3+/CD8+) was assessed via flow cytometry in the blood, spleen, and mesenteric lymph nodes (A). Antigen-specific induction of perforin in CD8+ T cells was analyzed by flow cytometry via comparison of unstimulated cells (NP) with cells stimulated with HIV Gag peptides (Peptide). Results from a single experiment are shown (B) and averages for all experiments are graphed (C). Antigen-specific cytolytic degranulation was measured via stimulation with peptide in the presence of an antibody to CD107a, followed by analysis using flow cytometry (C). P values reflect comparisons between mice vaccinated with Gag4Y alone with mice vaccinated with Gag4Y plus IL-12 or IL-28B.
Splenocytes from mice that received IL-28B secrete less TGFβ
We reasoned that it was possible that the inclusion of IL-12 or IL-28B in vaccination may have been phenotypically altering normal CD4+ T cells to look like Tregs, instead of inducing the expansion of fully functional Tregs. Therefore, to determine whether these cells were functioning as Tregs in addition to phenotypically resembling Tregs, we measured the ability of splenocytes from vaccinated mice to produce TGFβ, which is recognized as one of the major mediators of Treg-based noncontact immunosuppression.21 To accomplish this, we cultured splenocytes from each group of mice for 48 hours with a combination of PMA and ionomycin to determine TGFβ release from activated cells. At the end of this time period, supernatants were taken from cell cultures and were used in ELISAs to detect TGFβ. As shown in Figure 5B, activation of splenocytes isolated from mice that received IL-12 as an adjuvant resulted in a statistically significant increase in TGFβ production compared with mice that received Gag4Y alone (Figure 5B). This result suggests that the differences in Treg numbers observed via flow cytometry between mice that received IL-12 and mice that received HIV Gag4Y alone are correctly identifying Treg populations. In addition, splenocytes isolated from mice that received IL-28B as an adjuvant produced significantly less TGFβ when activated by PMA and ionomycin (Figure 5B). This, again, supports the flow cytometry data suggesting that there are differences in Treg populations in mice that received IL-28B compared with mice that received HIV Gag4Y alone.
As IL-2 is a key cytokine in the induction and expansion of Tregs,21 we reasoned that differences in Treg populations between vaccinated groups could be due to differential production of IL-2. To test this possibility we again measured cytokine release from activated splenocytes isolated from each group. Analysis of IL-2 output from these cells shows no significant difference between any of the groups (data not shown), suggesting that there is an alternate mechanism responsible for differences in Treg populations seen after DNA vaccination.
IL-28B but not IL-12 increases splenic CD8+ T cells
Upon determining that IL-28B could affect the amount of splenic Tregs, we decided to investigate whether this adjuvant had similar effects on other cell types after vaccination. To that end, splenocytes from control and vaccinated mice were analyzed for the presence of CD8 T cells (CD3+/CD8+) by flow cytometry. As shown in Figure 6A, the percentage of CD8 T cells in the spleens of control (pVAX) mice were not significantly different from mice who received the Gag4Y construct alone, or the Gag4Y construct with the IL-12 adjuvant. However, mice that received IL-28B as an adjuvant showed significantly higher percentages of CD8 T cells in the spleen compared with all other groups, suggesting that IL-28B can expand the splenic CD8+ T-cell population after immunization. To determine whether this effect of IL-28B was restricted to the spleen or could be seen in other lymphoid organs and peripheral blood, we next analyzed lymphocytes isolated from the mesenteric lymph nodes (MLNs) as well as circulating peripheral blood mononuclear cells (PBMCs) from each group of mice. Mice immunized with the HIV Gag4Y construct alone showed a small but not statistically significant increase in the number of CD8+ T cells found in MLNs compared with control mice. Mice that received IL-12 as an adjuvant showed increased numbers of CD8+ T cells in MLNs compared with mice that received Gag4Y alone, and this increase was able to reach statistical significance (Figure 6A). Mice that received IL-28B in conjunction with the HIV Gag4Y construct during immunization had slightly higher increases in CD8+ T-cell percentages, which reached an impressive statistical significance (P < .005). Lymphocytes isolated from peripheral blood showed increases in CD8+ T-cell populations only in the group that received the IL-28B adjuvant, which is reminiscent of the pattern seen in the spleen (Figure 6A). These results indicate that IL-28B, but not IL-12, increases the size of CD8+ T-cell populations in the spleen and peripheral blood of immunized mice, whereas both adjuvants are able to increase CD8+ T cells in MLNs.
IL-28B significantly increases HIV Gag-specific CD8+ T-cell perforin induction and degranulation
Upon determining that IL-28B was having a significant impact on the percentage of splenic CD8+ T cells after vaccination, we decided to perform further analysis on this cellular subset. It has previously been shown that IL-12 may influence the granularity of CD8+ T cells.19 As our previous experiments suggested that IL-28B was having a strong influence on cellular immunity (via IFNγ release) that was equal to or greater than IL-12 (Figure 3A), we asked whether IL-28B could influence cell granularity in the same fashion as IL-12. Therefore, we designed experiments to measure the antigen-specific induction of perforin in CD8+ T cells isolated from the spleens of each group of mice. To determine the amount of antigen-specific perforin up-regulation, we incubated isolated splenocytes with a media control or with a set of overlapping HIV Gag Clade C peptides for 6 hours, followed by extracellular and intracellular staining for cellular markers and perforin, followed by analysis via flow cytometry (Figure 6B). To prevent cytolytic degranulation, EGTA and Mg+2 were added to cultures as described in “Cell culture and staining for flow cytometry.”17 The results of this stimulation are presented in Figure 6C. CD8+ T cells in splenocytes from all groups incubated with media alone showed roughly equivalent amounts of perforin, suggesting that vaccination, with or without adjuvants, had no significant affect on basal CD8+ T-cell granularity in this system. Stimulation of splenocytes with overlapping HIV Gag peptides showed different results. CD8+ T cells in splenocytes from mice immunized with the HIV Gag4Y construct alone showed a modest increase in the percentage of cells falling into the perforinhi gate (Figure 6B) compared with control mice. However, CD8+ T cells taken from mice that had received IL-12 or IL-28B both showed increases in perforinhi cell percentages that were clearly higher than those taken from mice that received the Gag 4Y construct alone (Figure 6C). This result is consistent with previous reports that IL-12 may increase the perforin content of lymphocytes22 and is the first time this effect has been reported for IL-28B.
With the knowledge that IL-28B could influence the perforin content of CD8+ T cells, we examined whether this cytokine adjuvant could be affecting antigen-specific degranulation as well. To test this, we incubated cells in the same fashion as we did to measure perforin induction, save for the fact that no EGTA or Mg+2 was added to cultures, and an antibody to CD107a, which is a marker for degranulation,23 was instead added at the time of peptide stimulation as an enhanced stain. Cells were again subjected to staining for cellular markers, followed by analysis via flow cytometry. We observed that CD8+ T cells from mice that had received the Gag 4Y construct alone showed a low level of Gag-specific degranulation (Figure 6C). CD8+ T cells from mice that received IL-12 in combination with the HIV Gag 4Y construct showed a modest increase in antigen-specific degranulation compared with mice that received the Gag construct alone, but this difference did not reach statistical significance. However, CD8+ T cells from mice that received the IL-28B plasmid as an adjuvant in vaccination showed a significant increase in HIV Gag-specific degranulation compared with T cells taken from mice that did not receive adjuvant (Figure 6C). The results show that IL-28B causes a major and statistically significant increase in CD8+ T-cell degranulation when used as an adjuvant in DNA vaccination.
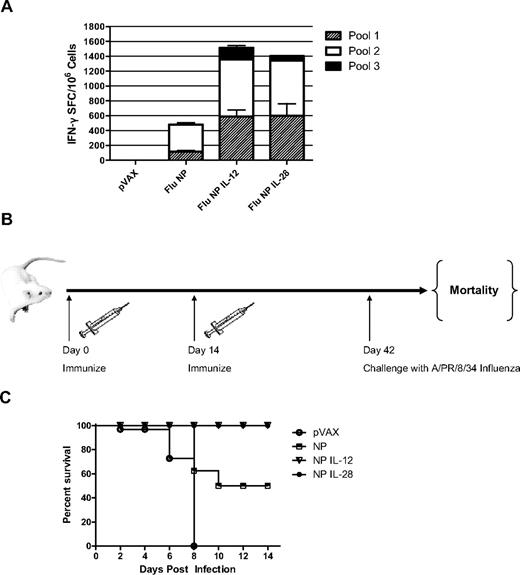
IL-28B protects from a lethal influenza challenge in vivo
Because our assays for cellular immune responses suggested that IL-28B had the potential to act as a strong adjuvant for Th1-biased cellular immunity, we decided to test the ability of this cytokine to protect against a lethal viral challenge in vivo. To accomplish this, we immunized 4 additional sets of mice (n = 8 mice per group) followed by electroporation. Control mice received 10 μg empty pVAX vector, whereas the other groups of mice received 10 μg of a plasmid encoding the influenza nucleoprotein (NP) alone or in addition to IL-12 or IL-28B. The nucleoprotein of influenza is an internal structural protein, and not exposed on the outside of the virion. Thus, immunity to influenza infection that is targeted against the NP protein is cellular as opposed to humoral immunity.16 Analysis of cellular immunity of vaccinated mice via IFNγ ELISpot showed that the IL-12 and IL-28B adjuvants induced increased responses to the influenza NP antigen in much the same way it augmented responses to the HIV Gag4Y construct (Figure 7A). After a 4-week postimmunization rest period (Figure 7B), all groups of mice were challenged intranasally with 10 LD50 of an H1N1 influenza strain: A/Puerto Rico/8/34 (A/PR/8/34). The mice were monitored over the course of the next 14 days for mortality associated with viral infection. Results of this experiment show that challenge of control mice resulted in 100% mortality by day 8 after infection (Figure 7C). Mice that received 10 μg of the NP construct showed 50% mortality over the next 14 days, suggesting that the NP construct alone was not completely sufficient to induce protection. IL-12, when used as an adjuvant in challenge studies, has been shown in the past to be able to induce significant protection against mortality associated with viral infections.13,14 This is also the case in the current study, as exhibited by the fact that mice that received IL-12 as an adjuvant to NP showed 100% protection from death as a result of infection. In addition, in agreement with our previous assays suggesting that IL-28B could induce potent cellular immune responses, mice that received IL-28B as an adjuvant to the NP construct also showed 100% survival after viral challenge. The results of this experiment show that IL-28B, when used as an adjuvant during DNA vaccination, may induce 100% protection from mortality associated with viral infection in vivo.
Protection from death in a lethal influenza challenge. (A) Mice (n = 8) were immunized on day 0 and day 14 with the influenza NP construct and with or without adjuvant, followed by electroporation using the CELLECTRA adaptive constant current device after each immunization. (B) IFNγ ELISpot responses were measured on day 21. (C) On day 42, mice were challenge intranasally with 10 LD50 A/PR/8/34, an H1N1 influenza strain. Mortality associated with influenza infection was tracked over the course of 14 days.
Protection from death in a lethal influenza challenge. (A) Mice (n = 8) were immunized on day 0 and day 14 with the influenza NP construct and with or without adjuvant, followed by electroporation using the CELLECTRA adaptive constant current device after each immunization. (B) IFNγ ELISpot responses were measured on day 21. (C) On day 42, mice were challenge intranasally with 10 LD50 A/PR/8/34, an H1N1 influenza strain. Mortality associated with influenza infection was tracked over the course of 14 days.
Discussion
The study presented here shows that plasmid-encoded IL-28B may have potent effects on antigen-specific immune responses when used as an adjuvant in DNA vaccination. IL-28B was able to augment antigen-specific immune response to a multiclade HIV Gag antigen in a Th1-biased fashion, which was evidenced by greatly enhanced IFNγ release during antigen-specific ELISpots as well as increased Gag-specific IgG2a levels detected in the sera of vaccinated mice. In addition, this is the first report to describe the ability of IL-28B to reduce splenic Treg populations after DNA vaccination, a great potential benefit of this cytokine. IL-28B was also shown here to be able to expand the splenic CD8+ T-cell population, and that these cells showed increased perforin induction and degranulation in response to cognate antigen. The fact that IL-28B was able to augment protection of mice in a lethal viral challenge model makes a strong case for continued testing of this cytokine as an adjuvant in vaccination.
The impact of IL-28B was measured against IL-12 because IL-12 is known to be a highly potent cytokine that is used often as an adjuvant in vaccination studies.9-13 Analysis of this comparison shows IL-28B to be at least as potent as IL-12 in some assays, if not better. Moreover, IL-28B affords additional benefits for vaccination that IL-12 does not, including increased antigen-specific antibody titers and an increased splenic CD8+ T-cell population that is capable of higher degrees of antigen-specific cytolytic degranulation. The effects of IL-28B and IL-12 on Treg populations were dramatically different. This is the first study to analyze the induction of Tregs in response to IL-12 in DNA vaccination and to report that this adjuvant may increase this cell population. Although the impact of this finding is not as yet clear, this result may support that IL-28B could be superior in specific situations where cellular immunity is paramount. The specific mechanism by which mice that received IL-12 had larger Treg populations remains unclear, although a recent report has highlighted the importance of the IL-12 receptor for the generation of Tregs in vivo,24 suggesting a possible link between this cytokine and the induction and expansion of the Treg population. The ability of IL-28B to reduce Treg numbers seems more likely to be a targeted mechanism, as it is able to increase some subsets of T cells (CD8) while reducing others (Treg). It is possible that this, too, is mediated through the IL-28 receptor, although additional studies into specific mechanisms are needed.
Results presented here constitute a significant analysis of the function of IL-28B in vivo and contribute to the beginning of our understanding of how IL-28B affects immune responses. The data suggest that IL-28B may be a regulator of the adaptive immune response in addition to its IFN-like functions, and this effect seems to focus largely on the number and function of CD8+ T cells. The fact that IL-28B induces an antiviral state in addition to being able to shape antigen-specific immune responses suggests that it is has the unique ability to bridge the gap between innate and adaptive immunity. Furthermore, IL-28B may have a unique role in immune therapy approaches over IL-12 in specific adjuvant settings. In particular, as an adjuvant in tumor immunity where tolerance is particularly an issue, IL-28B may be very useful. Further studies are needed to properly verify this.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 USC section 1734.
Acknowledgments
We thank Dr David Hokey for his input and technical assistance.
This work was supported in part by funding from the National Institutes of Health (D.B.W.).
National Institutes of Health
Authorship
Contribution: M.P.M. performed experiments, analyzed results, and made the figures; P.P., D.J.L., K.A.S., and N.C. performed experiments; J.Y. and M.P.M. designed and created plasmid constructs; and M.P.M. and D.B.W. conceived the study, designed experiments, and wrote the paper.
Conflict-of-interest disclosure: The laboratory of D.B.W. has grant funding and collaborations or consulting including serving on scientific review committees for commercial entities and in the interest of disclosure therefore notes potential conflicts associated with this work with Wyeth, VGX Pharmaceuticals, Bristol Myers Squibb, VIRxSYS, Ichor, Merck, Althea, Aldeveron, Inovio, and possibly others. The remaining authors declare no competing financial interests.
Correspondence: David Weiner, 422 Curie Blvd, 505 Stellar Chance Labs, University of Pennsylvania, Philadelphia, PA 19104; e-mail: dbweiner@mail.med.upenn.edu.