Abstract
In this issue of Blood, van Rooijen and colleagues demonstrate that zebrafish carrying a mutation in the von Hippel Lindau gene (VHL) develop Chuvash polycythemia, a hereditary human disease characterized by the dysregulation of hypoxia-inducible proteins including erythropoietin.
Chuvash polycythemia (CP), a disorder associated with inappropriately high erythropoietin secretion and increased proliferation of erythrocyte precursors, has been linked to a specific mutation of the von Hippel Lindau (VHL) gene. The C598T mutation leads to replacement of arginine by tryptophan at position 200 (Arg200Trp).1 In addition, Chuvash patients show hyperactivity of cardiopulmonary reflexes which suggests that the product of the VHL gene (pVHL) also participates in the regulation of respiration and circulation.2 Patients with CP do not have an increased risk of tumor development. This is important because inactivating mutations of the VHL gene are observed in VHL disease, which is a hereditary cancer syndrome. VHL disease predisposes affected individuals to visceral cysts and hemangiomata of the retina, of the central nervous system (described by Eugen von Hippel in 1904 and by Arvid Lindau in 1926, respectively), to pheochromocytomas, and to clear cell renal cell carcinomas (CCRCC).3 In addition, in the majority of cases of sporadic CCRCC, VHL mutations are detectable. Many different VHL mutations can cause VHL disease. Notably, none of the patients carrying a VHL mutation displays all these pathologies. This raises the question: How can defects of a single gene lead to so many diverse and apparently unrelated pathologies?
BrdU incorporation assay in wild-type and Vhl−/− zebrafish. Increased cell proliferation is detectable in all hematopoietic tissues of Vhl−/− embryos 7.5 days after fertilization, as shown in whole mount and cross-sections (original magnification ×20). CHT indicates caudal hematopoietic tissue; and PHT, pronephric hematopoietic tissue. See the complete figure in the article beginning on page 6449.
BrdU incorporation assay in wild-type and Vhl−/− zebrafish. Increased cell proliferation is detectable in all hematopoietic tissues of Vhl−/− embryos 7.5 days after fertilization, as shown in whole mount and cross-sections (original magnification ×20). CHT indicates caudal hematopoietic tissue; and PHT, pronephric hematopoietic tissue. See the complete figure in the article beginning on page 6449.
To answer this, it is important to consider the cell physiologic functions of pVHL. It is well established that pVHL is the substrate-recognizing subunit of an E3 ubiquitin ligase, which is critical for the oxygen-dependent regulation of the α-subunit of hypoxia-inducible transcription factors (HIFs). The canonical pathway of HIF-activation by hypoxia occurs as follows: when oxygen concentration is normal, HIF-α is hydroxylated on specific proline residues in a strictly oxygen-dependent enzymatic reaction by prolyl hydroxylase domain proteins (PHDs). pVHL specifically binds the hydroxylated transcription factor. As a consequence of pVHL binding, HIF-α rapidly undergoes polyubiquitination and proteasomal degradation. Therefore, in pVHL competent cells, HIF is active only when the oxygen concentration becomes low and thus limiting for hydroxylation. In cells expressing nonfunctional or no pVHL, however, this regulation is lost and HIF drives target gene expression even at high oxygen concentration. In this scenario, tissue specific HIF-subunit distribution and target gene expression enable different pathologies to arise from VHL inactivation. Importantly, however, pVHL also takes part in HIF independent processes, for example, extracellular matrix formation and the regulation of microtubule stability.4 How the loss of HIF-independent pVHL functions contributes to pathologic conditions in VHL-related diseases remains largely unresolved.
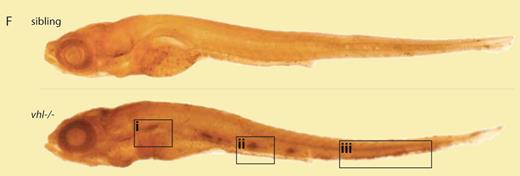
Van Rooijen et al have generated 2 zebrafish lines carrying inactivating Vhl mutations.5 The mutant embryos developed polycythemia (see figure) and showed up-regulation of hypoxia-inducible genes as well as hyperventilation, thus recapitulating key features of CP. Moreover, chemical activation of HIF by application of a prolyl hydroxylase inhibitor largely reproduced the Vhl-deficient phenotype. Injection of human wild-type VHL mRNA rescued the phenotype while the Arg200Trp mutant was almost ineffective. Of note, in cells from individuals affected with CP, the Arg200Trp mutation reduces but does not abrogate HIF binding. Therefore, it is thought that intermediate HIF activation causes human CP but is not sufficient to produce tumors. On the other hand, VHL patients carry a germline mutation of 1 VHL allele while the second allele is inactivated by somatic mutation later in life, which leads to tumor development in specific tissues. To date, the molecular event between biallelic VHL inactivation and tumor development is not entirely understood. Erythropoietin-producing cells, however, are not affected and therefore patients with VHL disease are usually not polycythemic.
Obviously, with respect to VHL functions and the consequences of VHL loss, many important issues have to be addressed. Therefore, van Rooijen et al have created a valuable tool to study VHL-associated human pathologies.
Conflict-of-interest disclosure: The authors declare no competing financial interests. ■

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal