Abstract
Recombinant adeno-associated virus (rAAV) vectors are considered promising for human gene replacement because they facilitate stable expression of therapeutic proteins in transduced tissues. Whether the success of gene therapy will be influenced by cellular immune responses targeting transgene-encoded proteins that are potentially immunogenic is unknown. Here we characterized CD8+ T-cell activity against β-galactosidase and enhanced green fluorescent protein, model antigens containing major histocompatibility complex (MHC) class I epitopes that are constitutively produced in murine skeletal muscle after rAAV vector transduction. Antigen-specific CD8+ T cells were detected in the spleen and liver of mice within 7 days of muscle transduction. CD8+ T-cell frequencies in these organs were stable, and effector functions were intact for months despite ongoing antigen production in muscle. CD8+ T cells also infiltrated transduced muscle, where frequencies were at least 5-fold higher than in untransduced spleen and liver. Significantly, the majority of antigen-specific CD8+ T cells in vector-transduced muscle were not functional. Loss of function in the muscle was associated with programmed death of the effector cells. Stable gene expression therefore depended on selective death of CD8+ T cells at the site of antigen production, an effective mechanism for subverting immunity that is also potentially reversible.
Introduction
Recombinant adeno-associated virus (rAAV) vectors have potential for delivery of therapeutic genes to humans. Viral replication (rep) and capsid (cap) genes can be substituted with up to 4.7 kilobases (kb) of heterologous DNA, resulting in a nonreplicating genome that can be packaged in an AAV capsid.1 Studies in rodents, canines, and nonhuman primates have documented long-term expression of transgenes encoding self and even some foreign proteins.2-7 Another useful feature of this vector is the capacity to transduce multiple tissue types, including the central nervous system, eye, liver, and skeletal muscle.8 Muscle is of particular interest for gene replacement because it is reasonably accessible for vector delivery and has the potential to produce large quantities of therapeutic proteins. Transduction of skeletal muscle with rAAV vectors encoding factor IX has at least transiently normalized blood clotting function in mice and dogs with hemophilia B.9-11 Likewise, in animal models of Duchenne muscular dystrophy, rAAV vectors encoding functional dystrophin genes can partially reverse the dystrophic phenotype of cardiac and skeletal muscle.12
The success of gene transfer to muscle may be influenced by host immunity. Transient immune suppression does seem to improve the longevity of factor IX or dystrophin gene expression in the muscle of genetically deficient dogs.13 This observation is consistent with immune-mediated clearance of antigen-positive myocytes in at least some individual subjects. CD8+ T cells are potentially important contributors to immune-mediated loss of transgene expression, but little is known about responses in muscle or the nature of antigens that might be targeted. AAV capsid proteins have been proposed as the target of an undesirable CD8+ T-cell response.14-18 Capsid genes are absent from the vector genome, but it is conceivable that particle-associated capsid proteins enter the class I or II major histocompatibility complex (MHC) processing pathway of transduced cells.
Therapeutic proteins such as factor IX and dystrophin should also have potential for immune recognition as neoantigens if expressed in the muscle of persons with genes that are absent, truncated, or contain missense mutations.19,20 Whether therapeutic proteins produced in rAAV vector-transduced myocytes will be effectively processed for MHC class I presentation is nonetheless controversial. Persistent synthesis of some foreign proteins in the muscle of immunocompetent mice might argue against this possibility.4,5,21-23 For instance, human factor IX failed to provoke a detectable CD8+ T-cell response when expressed in rAAV vector-transduced murine muscle.22 This apparent absence of CD8+ T-cell immunity against a human protein was overcome by intramuscular delivery of a recombinant adenovirus (rAd) vector carrying the identical factor IX transgene, resulting in destruction of antigen-positive muscle fibers.22 A similar outcome was reported when CD8+ T-cell immunity was compared in mice receiving rAAV and rAd vectors encoding bacterial β-galactosidase.21 Although these observations offer indirect evidence for failed priming of CD8+ T cells by the rAAV (but not the rAd) vector, detailed insight into mechanism(s) that subvert the response is still lacking. Two recent studies have described priming of murine CD8+ T cells specific for the same HIV-1 gag epitope expressed in rAAV vector-transduced murine myocytes.24,25 These T cells had an effector rather than memory phenotype and display poor proliferation after ex vivo stimulation, but whether defects in differentiation or function account for the failure to clear transduced myocytes in a gene therapy setting is not known.
In this study, we re-examined the priming and fate of CD8+ T cells targeting β-galactosidase and enhanced green fluorescent protein (eGFP), model antigens for gene therapy that are persistently expressed in rAAV vector-transduced muscle. Our findings indicated that durable CD8+ T-cell responses specific for eGFP and β-galactosidase were primed despite long-term expression of these antigens in murine skeletal muscle. Stable frequencies of CD8+ T cells specific for transgene-encoded proteins were maintained in the spleen and liver of the rAAV vector-treated animals, and their effector functions were not impaired. Significantly, antigen-specific CD8+ T cells also infiltrated rAAV vector-transduced muscle tissue, an unexpected result that seemed inconsistent with the long-term survival of antigen-producing cells. Failure to clear antigen-positive myocytes was associated with a loss of effector function that occurred because CD8+ T cells in the transduced muscle, but not spleen or liver, entered the programmed death pathway. Priming of antigen-specific CD8+ T cells in a model of successful gene transfer indicates that the balance between host immunity and survival of vector-transduced cells may be more tenuous than previously thought.
Methods
Vectors
Replication-defective serotype 2 rAAVeGFP and rAAVβgal vectors expressing transgenes controlled by the human cytomegalovirus immediate-early promoter were produced by The Research Institute at Nationwide Children's Hospital Vector Core facility (Columbus, OH). The replication-defective serotype 5 (ΔE1/E3) rAdeGFP vector expressing eGFP regulated by the same promoter was purchased from Vector Biolabs (Philadelphia, PA).
Animals, vector administration, and mononuclear cell isolation
BALB/C and C57BL/6 mice used in this study were purchased from Charles River Laboratories (Wilmington, MA). The Research Institute at Nationwide Children's Hospital Institutional Animal Care and Use Committee approved all animal experiments. DNase-resistant particles (2 × 1011) of rAAVeGFP, rAAVβgal, or 107 plaque-forming units of rAdeGFP in 50 μL of sterile saline were injected into the left quadriceps muscle of 6- to 8-week-old female BALB/C (rAAVeGFP and rAdeGFP) and C57BL/6 (rAAVβgal) mice. CD8+ T-cell responses were characterized using mononuclear cell suspensions from spleen, liver, and muscle. Livers perfused with phosphate-buffered saline were forced through wire mesh and centrifuged on a Percoll gradient to enrich intrahepatic mononuclear cells. Quadriceps muscle digested in 0.2% collagenase II (Sigma-Aldrich, St Louis, MO) and passed through wire mesh was also centrifuged over Percoll for mononuclear cell isolation.
IFN-γ ELISpot analysis
In brief, splenocytes (2 × 105/well) were cultured in duplicate wells of a 96-well flat-bottomed membrane plate (Millipore, Billerica, MA) previously coated with anti–interferon-γ (IFN-γ) antibodies (U-CyTech, Utrecht, The Netherlands). Cells were then stimulated with splenocytes from an uninjected donor pulsed with either 1 μg/mL eGFP200-208 or βgal96-103 peptides in 200 μL of RPMI 1640 medium (containing 10% fetal calf serum, penicillin, and streptomycin). Negative control H-2Kd-restricted peptide epitopes from the F protein of respiratory syncytial virus (RSVF85-93) and the H-2Kb-restricted epitope from chicken ovalbumin (OVA257-264) were also used. In some experiments, side-by-side flow analysis was used to determine the frequency of eGFP-tetramer-positive cells within each tissue before plating. Then, equal numbers of eGFP-tetramer-positive cells were plated per Enzyme-linked immunospot (ELISpot) well for each tissue analyzed. Splenocytes from an uninjected mouse were added so that the total number of cells per well (400 000) was identical for spleen, liver, and muscle. After 48 hours, plates were developed for IFN-γ spot formation and counted using a Cellular Technologies Limited Systems analyzer (CTL, Cleveland, OH). Responses were scored as positive if (1) there were fewer than 10 background spots in wells stimulated with control peptide epitopes and (2) wells stimulated with relevant peptide epitopes had at least 10 spots over background values. Responses are reported as the number of spot-forming cells (SFCs) per 106 mononuclear cells from liver or spleen.
Flow cytometry
Mononuclear cell suspensions were first stained with antibodies to CD3, CD4, F4/80, B220, and CD8 (Invitrogen, Carlsbad, CA) followed by incubation with the appropriate H-2Kd eGFP200-208 or H-2Kb β gal96-103 tetramer (provided by the National Institutes of Health Tetramer Facility, Atlanta, GA). In some experiments, mononuclear cells were also incubated with antibodies to CD44, CD62L, CD127 (Invitrogen), and the CD43 activation–associated glycoform (clone 1B11; BD Pharmingen, San Diego, CA), followed by streptavidin-allophycocyanin (Invitrogen) if required (CD127 and the CD43 activation–associated glycoform). Immediately before analysis, freshly stained mononuclear cells were briefly incubated (15 minutes at room temperature) in 1 μg/mL propidium iodide, a vital dye used for live/dead discrimination (Invitrogen). For detection of apoptosis, cells freshly stained with T-cell markers and tetramer were coincubated with propidium iodide and annexin V (BD Biosciences, San Jose, CA) immediately before analysis. An LSR II flow cytometer (BD Biosciences) was used to enumerate cell populations and the data were analyzed using FlowJo software (TreeStar, Ashland, OR).
Intracellular IFN-γ detection and CD107a/b degranulation assay
The degranulation assay was performed as described by Betts et al.26 Splenocytes stimulated with 1 μg/mL of eGFP200-208 peptide in the presence of costimulation (anti-CD49d and anti-CD28 antibodies; BD Pharmingen) and CD107a- and CD107b-specific antibodies (BD Pharmingen) for 6 hours at 37°C in the presence of monensin followed by surface staining with the relevant MHC class I tetramer and antibodies against CD4, B220, F4/80, CD3, and CD8. After fixation, cells were permeabilized before staining for intracellular IFN-γ. LIVE/DEAD Fixable Blue Dead Cell Stain (Invitrogen) was used as a live/dead discriminator.
Antigen capture ELISA for eGFP and β-galactosidase quantification
Supernatants from homogenized transduced and nontransduced muscle containing serial dilutions of eGFP (as a standard) were added to duplicate wells of Immunolon plates coated with goat anti-GFP polyclonal antibody (Rockland, Gilbertsville, PA) containing 2% goat serum. Plates were developed with biotinylated mouse, anti-GFP antibodies followed by NeutrAvidin-horseradish peroxidase (Pierce, Rockford, IL). Plates were developed with tetramethylbenzidine substrate and absorbance was read at 450 nm. β-Galactosidase was quantified using a β-gal enzyme-linked immunosorbent assay (ELISA) kit (Roche, Boulder, CO). Standard absorbance curves generated with recombinant eGFP (BioVision Incorporated, Mountain View, CA) and β-gal (Roche) proteins in nontransduced muscle homogenates were used to calculate antigen concentrations in tissue homogenates from transduced muscle.
Analysis of β-galactosidase enzymatic activity in tissue sections
Sectioned frozen quadriceps muscle tissue was fixed in a formaldehyde/0.2% glutaraldehyde solution (Sigma-Aldrich) and incubated in the presence of 1 mg/mL 5-bromo-4-chloro-3-indolyl-β-d-galactopyranoside (United States Biochemical, Cleveland, OH) in 5 mmol/L potassium ferrocyanide/2 mM MgCl2 (Sigma-Aldrich) for 4 hours at 37°C. Eosin was used as a counter-stain for visualization using a Zeiss Immersional 518C light microscope (Zeiss, Welwyn Garden City, United Kingdom). A Carl Zeiss Axio Camera and Axiovision 3.1 software were used to capture images at 10× magnification with a 10× objective lens.
Results
Expression of an eGFP transgene in vector-transduced muscle
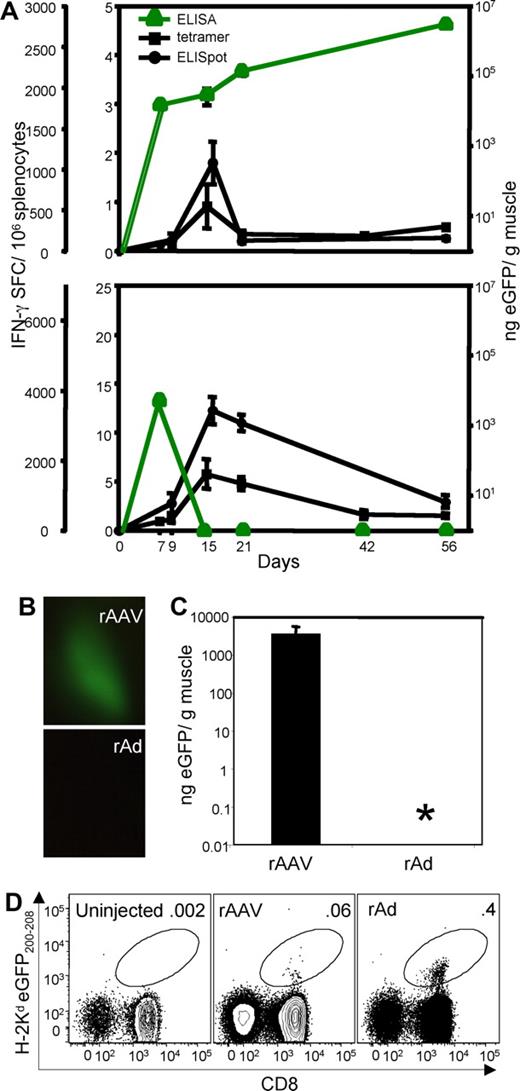
An rAAV vector encoding eGFP established a persistent pattern of transgene expression in the quadriceps muscle of BALB/C mice (Figure 1). Expression of eGFP was observed within 7 days of vector administration and increased through 56 days of follow-up (Figure 1A). Muscle-associated eGFP was still detected 252 days after vector delivery by live imaging of the quadriceps (Figure 1B) and quantification of antigen in tissue extracts by ELISA assay (Figure 1C). This persistent pattern of protein expression contrasted sharply with that in muscle transduced with a replication incompetent adenovirus vector expressing eGFP (rAdeGFP). Muscle recovered at day 7 after rAdeGFP vector treatment contained eGFP when assessed by antigen-capture ELISA assay, but the protein was not detected by day 15 or at later time points, indicating that transduced myocytes were cleared (Figure 1A). Rapid clearance of antigen-positive myocytes observed here is consistent with other studies in which model antigens were delivered to muscle with recombinant adenovirus vectors.21,22
Pattern of eGFP expression and CD8+ T-cell immunity in vector-treated animals. (A) Mice treated with rAAVeGFP (top panel) and rAdeGFP (bottom panel) were analyzed for eGFP protein content of transduced muscle and frequency of eGFP200-208 specific CD8+ T cells in spleen by IFN-γ ELISpot and tetramer analysis. Groups of 5 to 8 individual mice (with ± SEM) is shown (note differences in scale). eGFP gene expression in quadriceps muscle 252 days after vector administration was evaluated by direct imaging (B) and protein quantification by ELISA (C). Asterisk indicates that eGFP was below the ELISA detection limit. (D) Flow cytometric analysis of splenocytes from mice that were untreated (left) or inoculated intramuscularly 252 days earlier with rAAVeGFP (center) and rAdeGFP (right). Numbers represent the percentage of CD8+ T cells that stain with the H-2Kd eGFP200-208 tetrameric complex. Gated on FSC/SSC appropriate for lymphocytes, propidium iodide–negative (PI−)CD4−B220−F4/80−CD3+ cells.
Pattern of eGFP expression and CD8+ T-cell immunity in vector-treated animals. (A) Mice treated with rAAVeGFP (top panel) and rAdeGFP (bottom panel) were analyzed for eGFP protein content of transduced muscle and frequency of eGFP200-208 specific CD8+ T cells in spleen by IFN-γ ELISpot and tetramer analysis. Groups of 5 to 8 individual mice (with ± SEM) is shown (note differences in scale). eGFP gene expression in quadriceps muscle 252 days after vector administration was evaluated by direct imaging (B) and protein quantification by ELISA (C). Asterisk indicates that eGFP was below the ELISA detection limit. (D) Flow cytometric analysis of splenocytes from mice that were untreated (left) or inoculated intramuscularly 252 days earlier with rAAVeGFP (center) and rAdeGFP (right). Numbers represent the percentage of CD8+ T cells that stain with the H-2Kd eGFP200-208 tetrameric complex. Gated on FSC/SSC appropriate for lymphocytes, propidium iodide–negative (PI−)CD4−B220−F4/80−CD3+ cells.
CD8+ T-cell immunity in mice with eGFP-positive muscle
Mice treated with the rAAVeGFP and rAdeGFP vectors were next compared for CD8+ T-cell immunity against an H-2Kd–restricted eGFP epitope designated eGFP200-208. As expected, splenic antigen-specific CD8+ T cells expanded rapidly in mice treated with the rAdeGFP vector when measured with an MHC class I tetramer or by an IFN-γ ELISpot assay.27 Peak CD8+ T-cell activity at day 15 was kinetically associated with eGFP clearance from muscle and followed by a prolonged contraction phase to form a long-lived memory population that was still detectable 252 days later (Figure 1A bottom panel, and D). Antigen-specific CD8+ T cells were also observed as early as 7 days after delivery of the rAAVeGFP vector (Figure 1A top panel). The response peaked at day 15 but was not accompanied by a reduction in antigen production within the quadriceps muscle. This ineffective immune response was prolonged; antigen-specific CD8+ T cells were detected in spleen (Figure 1D) and liver (data not shown) 9 months after vector delivery despite ongoing eGFP production in myocytes. Long-term survival of rAAVeGFP-transduced myocytes in animals with stable frequencies of antigen-specific CD8+ T cells was unexpected. We therefore sought to understand how effector lymphocytes are subverted in mice with a well-established pattern of persistent antigen expression.
CD8+ T-cell phenotype and function
Mice that are chronically infected with the lymphocytic choriomeningitis virus (LCMV) display defects in CD8+ T-cell differentiation and function because of persistent antigenic stimulation.28 Long-lived expression of eGFP in the muscle treated with the rAAVeGFP vector suggested the potential for a similar defect in the development of CD8+ T-cell memory and/or maintenance of function. Therefore, the phenotype and function of antigen-specific CD8+ T cells in spleen was assessed 2 months after rAAVeGFP or rAdeGFP vector delivery to the quadriceps muscle.
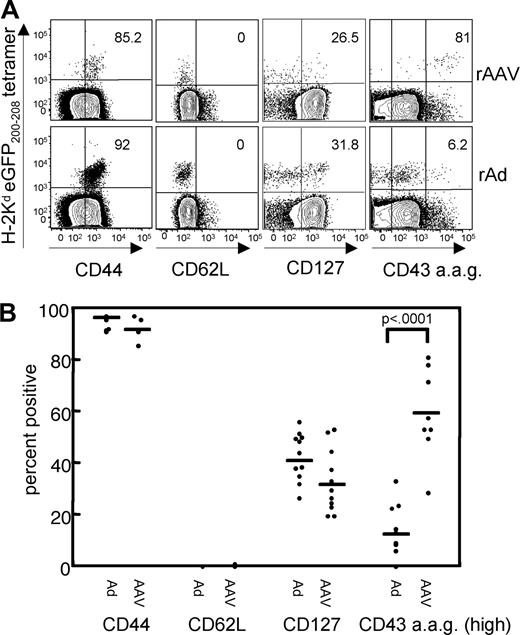
Previously published work described a “novel partially exhausted phenotype” for CD8+ T cells from rAd vector-primed mice,29 which is consistent with our observations. In brief, no obvious population of eGFP-tetramer positive CD8+ T cells with a central memory phenotype was observed in mice receiving the control rAdeGFP vector at day 56, as defined by coexpression of CD44 (a marker of antigen experienced cells), CD62L (required for lymph node homing of naive and memory subsets), and CD127 (interleukin [IL]–7α receptor, a survival factor expressed on naive and memory subsets; Figure 2), although a small percentage (31.8%) did express CD127 by this time point. In addition, early after rAdeGFP vector delivery, most eGFP200-208-specific CD8+ T cells showed high expression of the CD43 activation–associated glycoform, a marker of CTL function that is up-regulated on effector but not memory populations (Figure S1, available on the Blood website; see the Supplemental Materials link at the top of the online article). High expression of the CD43-activation–associated glycoform was lost on the rAdeGFP-primed cells by day 56 when antigen was no longer detected in muscle (Figure 2). Mice treated with the rAAVeGFP vector also lacked CD8+ T cells with a central memory phenotype at day 56. However, they were clearly different from those in rAdeGFP-treated animals because a statistically higher proportion (greater than 80%) expressed high levels of the CD43 activation–associated glycoform. Most antigen-specific CD8+ T cells from rAAVeGFP-treated animals therefore seemed to have a constant effector phenotype weeks after a persistent pattern of eGFP expression was established.
Phenotype analysis of splenic eGFP-specific CD8+ T cells. (A) 56 days after rAAVeGFP (top panel) or rAdeGFP (bottom panel) administration, splenocytes were costained with the eGFP200-208 tetramer and antibodies to CD8, CD44, CD62L, CD127, and CD43 activation–associated glycoform (CD43 a.a.g.). Numbers represent percentage of tetramer+ CD8+ T cells that stain positive for each cell surface molecule. Gated as in Figure 1D. Data represent 2 independent experiments with 5 to 8 individual animals per group. (B) Scatter plot representing eGFP200-208 tetramer and antibody staining to cell surface markers CD44, CD62L, CD127 and the CD43 activation–associated glycoform on splenocytes isolated from individual rAAVeGFP-treated and rAdeGFP-treated mice at day 56. Each dot represents the frequency of eGFP-tetramer+ cells that stain positive for each cell surface marker for an individual mouse. Statistical differences in surface marker expression between the rAdeGFP and rAAVeGFP-primed cells were analyzed using the Student t test.
Phenotype analysis of splenic eGFP-specific CD8+ T cells. (A) 56 days after rAAVeGFP (top panel) or rAdeGFP (bottom panel) administration, splenocytes were costained with the eGFP200-208 tetramer and antibodies to CD8, CD44, CD62L, CD127, and CD43 activation–associated glycoform (CD43 a.a.g.). Numbers represent percentage of tetramer+ CD8+ T cells that stain positive for each cell surface molecule. Gated as in Figure 1D. Data represent 2 independent experiments with 5 to 8 individual animals per group. (B) Scatter plot representing eGFP200-208 tetramer and antibody staining to cell surface markers CD44, CD62L, CD127 and the CD43 activation–associated glycoform on splenocytes isolated from individual rAAVeGFP-treated and rAdeGFP-treated mice at day 56. Each dot represents the frequency of eGFP-tetramer+ cells that stain positive for each cell surface marker for an individual mouse. Statistical differences in surface marker expression between the rAdeGFP and rAAVeGFP-primed cells were analyzed using the Student t test.
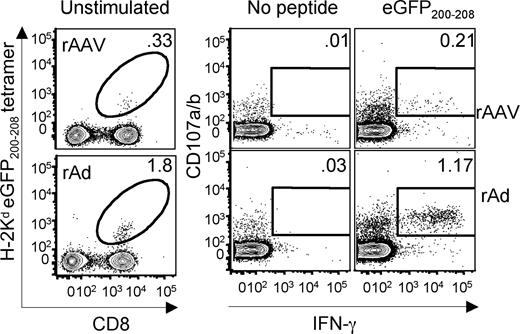
We next sought to determine whether the rAAVeGFP-primed CD8+ T cells in spleen maintained effector functions despite ongoing expression of the eGFP transgene in muscle. Both the rAAVeGFP-primed and the rAdeGFP-primed CD8+ T cells were tested for their ability to secrete the effector cytokine IFN-γ and degranulate in response to stimulation with cognate antigen (Figure 3). Persistent transgene expression in rAAVeGFP-treated animals was not necessarily facilitated by a loss of IFN-γ production or cytotoxic degranulation as measured by cell surface expression of CD107a and CD107b. At day 56, the frequency of spleen cells from rAAVeGFP and rAdeGFP-treated animals that released IFN-γ and degranulated after 6 hours of eGFP200-208 epitope stimulation (1.17% rAdeGFP versus 0.21% rAAVeGFP; Figure 3 left panel) was proportionally similar to the frequency of tetramer-positive cells (1.8% rAdeGFP versus 0.33% rAAVeGFP; Figure 3 right panel). Thus, approximately two-thirds of tetramer-positive CD8+ T cells in spleen were dually functional regardless of the vector used for priming. These observations suggested that eGFP-specific CD8+ T cells in the spleen of rAAVeGFP-transduced animals with a persistent pattern of antigen production had a functional profile similar to those measured in rAdeGFP-treated animals that successfully cleared the antigen. In summary, the phenotype and functional data together suggested that eGFP expression in the rAAVeGFP-treated mice persisted despite the priming and maintenance of a functional, effector CD8+ T-cell population.
Functional analysis of splenic eGFP-specific CD8+ T cells. The percentage of splenic CD8+ T cells staining with eGFP200-208 tetramer 56 days after intramuscular rAAVeGFP or rAdeGFP inoculation is indicated (left panel). The frequency of CD8+ T cells that coexpressed IFN-γ and CD107a/b after 6 hours in the presence or absence of eGFP200-208 peptide is also shown (right panel). Data are representative of 3 experiments each with spleens pooled from 5 animals. Dot plots gated on FSC/SSC appropriate for lymphocytes, LIVE/DEAD Blue−CD4−B220−F4/80−CD3+ (left panel) and CD8+ (right panel) cells.
Functional analysis of splenic eGFP-specific CD8+ T cells. The percentage of splenic CD8+ T cells staining with eGFP200-208 tetramer 56 days after intramuscular rAAVeGFP or rAdeGFP inoculation is indicated (left panel). The frequency of CD8+ T cells that coexpressed IFN-γ and CD107a/b after 6 hours in the presence or absence of eGFP200-208 peptide is also shown (right panel). Data are representative of 3 experiments each with spleens pooled from 5 animals. Dot plots gated on FSC/SSC appropriate for lymphocytes, LIVE/DEAD Blue−CD4−B220−F4/80−CD3+ (left panel) and CD8+ (right panel) cells.
Function and fate of intramuscular CD8+ T cells
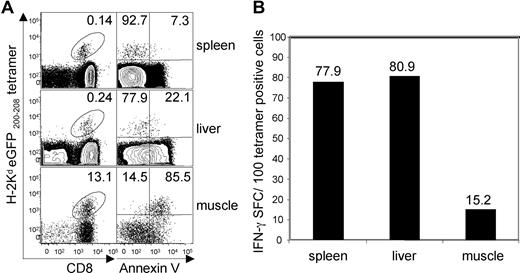
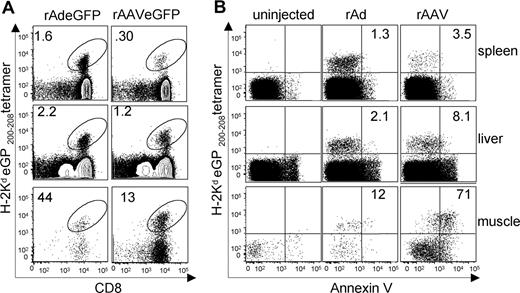
Why primed CD8+ T cells might fail to clear rAAVeGFP-transduced myocytes is unknown. It is possible that they did not migrate into transduced muscle or were present at frequencies too low to mediate clearance of antigen-positive myocytes. We therefore compared the homing of eGFP200-208-specific CD8+ T cells to muscle 2 months (56 days) after transduction with the rAdeGFP versus rAAVeGFP vectors. At this time point, mild focal inflammation was observed in antigen-positive muscle of rAAVeGFP-treated animals (data not shown), confirming earlier observations that mononuclear cell infiltration is limited or unremarkable despite persistent transgene expression.4,21 As expected, muscle from the rAdeGFP-transduced muscle was histologically normal several weeks after apparent antigen clearance (data not shown). Despite limited inflammation, approximately 5 times more CD8+ T cells were recovered from muscle treated with rAAVeGFP than that treated with rAdeGFP. Many of these infiltrating CD8+ T cells were antigen-specific. Indeed, eGFP-tetramer positive CD8+ T cells were highly enriched in the rAAVeGFP-transduced muscle (13.1%; Figure 4A left column) compared with untransduced spleen (0.14%; Figure 4A left column) and liver (0.24%; Figure 4A left column) from the same animals. There are at least 2 explanations for the failure of the muscle-infiltrating CD8+ T cells to clear rAAVeGFP-transduced myocytes. The first is that the target cells were resistant to immune-mediated destruction, although this seemed unlikely because persistent gene expression can be prevented by codelivery of an immunogenic rAd vector expressing the same transgene.21,24
Analysis of CD8+ T cells infiltrating rAAVeGFP-transduced quadriceps muscle. (A) (Left column) H-2Kd eGFP200-208 tetramer staining of lymphocytes isolated from spleen, liver, and muscle of mice injected with rAAVeGFP 56 days earlier. Numbers represent the percentage of CD8+ T cells that costain with the eGFP tetramer. Plots were gated as in Figure 1D. (Right column) Annexin V binding by H-2Kd eGFP200-208 tetramer+ CD8+ T lymphocytes isolated from spleen, liver, and muscle of mice injected with rAAVeGFP 56 days earlier. Numbers represent the percentage of tetramer+ cells that are negative (top left quadrant) and positive (top right quadrant) for annexin V binding. Plots were gated on FSC/SSC appropriate for lymphocytes, PI−CD4−B220−F4/80−CD3+CD8+ cells. (B) Side-by-side IFN-γ ELISpot analysis of eGFP200-208-specific CD8+ T lymphocytes harvested from spleen, liver, and quadriceps muscle 56 days after transduction with rAAVeGFP (performed in parallel with experiment depicted in panel A). Numbers represent the number of spot forming cells per 100 eGFP-tetramer+ cells. Data represent 2 independent experiments each with tissues pooled from 5 mice. The relationship between IFN-γ secretion and annexin V binding was assessed using the standard correlation equation, where r = −.95, P < .001; n = 6.
Analysis of CD8+ T cells infiltrating rAAVeGFP-transduced quadriceps muscle. (A) (Left column) H-2Kd eGFP200-208 tetramer staining of lymphocytes isolated from spleen, liver, and muscle of mice injected with rAAVeGFP 56 days earlier. Numbers represent the percentage of CD8+ T cells that costain with the eGFP tetramer. Plots were gated as in Figure 1D. (Right column) Annexin V binding by H-2Kd eGFP200-208 tetramer+ CD8+ T lymphocytes isolated from spleen, liver, and muscle of mice injected with rAAVeGFP 56 days earlier. Numbers represent the percentage of tetramer+ cells that are negative (top left quadrant) and positive (top right quadrant) for annexin V binding. Plots were gated on FSC/SSC appropriate for lymphocytes, PI−CD4−B220−F4/80−CD3+CD8+ cells. (B) Side-by-side IFN-γ ELISpot analysis of eGFP200-208-specific CD8+ T lymphocytes harvested from spleen, liver, and quadriceps muscle 56 days after transduction with rAAVeGFP (performed in parallel with experiment depicted in panel A). Numbers represent the number of spot forming cells per 100 eGFP-tetramer+ cells. Data represent 2 independent experiments each with tissues pooled from 5 mice. The relationship between IFN-γ secretion and annexin V binding was assessed using the standard correlation equation, where r = −.95, P < .001; n = 6.
The second possibility is that antigen-specific CD8+ T cells were silenced upon infiltration into muscle. We therefore assessed the capacity of antigen-specific CD8+ T cells from eGFP-positive muscle to produce IFN-γ after eGFP200-208 peptide stimulation. Equal numbers of tetramer-positive cells from spleen, liver, and muscle of rAAVeGFP-treated animals were tested for peptide-stimulated IFN-γ production in an ELISpot assay. When calculated as a percentage of tetramer-positive cells added to the ELISpot assay, most eGFP200-208-specific CD8+ T cells from spleen (78%) and liver (81%) were functional (Figure 4B), consistent with results obtained by intracellular cytokine staining (Figure 3). In sharp contrast, only 15% of antigen-specific CD8+ T cells from muscle produced IFN-γ, indicating that most were unable to respond to the cognate epitope (Figure 4B).
Effector CD8+ T cells infiltrating muscle might lose function if they receive a signal for activation-induced death upon re-encountering cognate antigen.30 Tetramer-positive CD8+ T cells recovered from muscle, liver, and spleen of rAAVeGFP-treated animals were therefore compared for binding of annexin V, an indicator of apoptosis. Greater than 80% of eGFP200-208 tetramer-positive CD8+ T cells from rAAVeGFP-transduced muscle bound annexin V (Figure 4A right column) compared with less than 25% in untransduced spleen and liver from the same animals, a difference that was statistically significant (spleen vs muscle, P < .01; liver vs muscle, P < .01; spleen vs liver, P > 0.1). Localization of nonapoptotic CD8+ T cells to liver and spleen is consistent with earlier studies involving model virus infections of mice.31,32 Viable, long-lived CD8+ T cells accumulated in these peripheral tissues even if infection was initiated with a virus such as influenza that replicated exclusively in the lung.31,32 Together these results indicated that programmed death was restricted to effector cells present in antigen-positive tissue (Figure 4A right column). It is noteworthy that the percentage of tetramer-positive CD8+ T cells in muscle that produced IFN-γ (15.2%; Figure 4B) was almost identical to the percentage that did not bind annexin V (14.5%; Figure 4A right column) in experiments in which function and apoptosis were analyzed simultaneously. Indeed, in all 3 tissues, the percentage of eGFP200-208-specific cells secreting IFN-γ was inversely proportional to the percentage that was apoptotic (correlation coefficient r = −.95, n = 6; P < .001). This observation indicated that annexin V binding CD8+ T cells were enriched in antigen-positive muscle and lacked function.
To confirm that susceptibility to programmed death was specific to rAAVeGFP-transduced muscle with a constitutive pattern of transgene expression, we also examined CD8+ T cells from the muscle of rAdeGFP-treated animals at day 56 after apparent clearance of antigen. A few CD8+ T cells specific for the eGFP200-208 epitope were still present in the rAdeGFP-treated muscle (Figure 5A), probably reflecting the propensity of antigen-specific cells to persist in tissues even after elimination of antigen.31,32 Less than 15% of these antigen-specific CD8+ T cells bound annexin V, indicating that the massive level of apoptosis observed in rAAV-eGFP treated muscle was largely absent (Figure 5B).
Analysis of CD8+ T cells infiltrating rAAVeGFP and rAdeGFP-transduced quadriceps muscle. (A) H-2Kd eGFP200-208 tetramer staining of lymphocytes isolated from spleen, liver, and muscle of mice injected with rAAVeGFP and rAdeGFP 56 days earlier. Numbers represent the percentage of CD8+ T cells that costain with the eGFP tetramer. Plots were gated as in Figure 1D. (B) Annexin V binding by H-2Kd eGFP200-208 tetramer+ CD8+ T lymphocytes harvested from quadriceps muscle 56 days after transduction with rAAVeGFP or rAdeGFP. Annexin V binding by eGFP200-208-specific CD8+ T cells isolated from the spleen and liver of the same animals are shown for comparison. Plots gated as in Figure 4A (right column). Numbers represent the percentage of tetramer+ cells (rAAVeGFP and rAdeGFP-inoculated animals) that bind annexin V. Data represent 4 independent experiments each with tissues pooled from 5 mice. For interpretation of differences in annexin V binding by tetramer+ cells in spleen, liver and muscle, an analysis of variance test was performed (1-way ANOVA for correlated samples followed by Tukey's test). For the rAAVeGFP-treated mice, spleen versus muscle P < .01, liver versus muscle P < .01 and spleen versus liver P > .1. For the rAdeGFP-treated mice, differences in variance among the 3 tissues were not significant.
Analysis of CD8+ T cells infiltrating rAAVeGFP and rAdeGFP-transduced quadriceps muscle. (A) H-2Kd eGFP200-208 tetramer staining of lymphocytes isolated from spleen, liver, and muscle of mice injected with rAAVeGFP and rAdeGFP 56 days earlier. Numbers represent the percentage of CD8+ T cells that costain with the eGFP tetramer. Plots were gated as in Figure 1D. (B) Annexin V binding by H-2Kd eGFP200-208 tetramer+ CD8+ T lymphocytes harvested from quadriceps muscle 56 days after transduction with rAAVeGFP or rAdeGFP. Annexin V binding by eGFP200-208-specific CD8+ T cells isolated from the spleen and liver of the same animals are shown for comparison. Plots gated as in Figure 4A (right column). Numbers represent the percentage of tetramer+ cells (rAAVeGFP and rAdeGFP-inoculated animals) that bind annexin V. Data represent 4 independent experiments each with tissues pooled from 5 mice. For interpretation of differences in annexin V binding by tetramer+ cells in spleen, liver and muscle, an analysis of variance test was performed (1-way ANOVA for correlated samples followed by Tukey's test). For the rAAVeGFP-treated mice, spleen versus muscle P < .01, liver versus muscle P < .01 and spleen versus liver P > .1. For the rAdeGFP-treated mice, differences in variance among the 3 tissues were not significant.
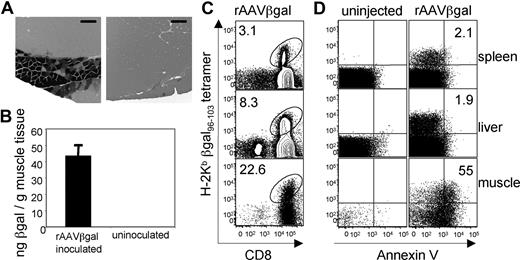
Finally, we extended this observation to a second model antigen, β-galactosidase (Figure 6). As expected,4,33 persistent β-galactosidase synthesis was observed in the quadriceps muscle of C57BL/6 mice at day 168 after rAAVβ gal vector delivery (Figure 6A). More than 20% of CD8+ T cells recovered from transduced muscle at day 56 stained with an H-2Kb tetramer containing a β-galactosidase epitope (βgal96-103) even though antigen persisted during months of follow-up. Tetramer-positive cells were also detected in spleen and liver, but again only those in muscle displayed high levels of annexin V binding (Figure 6C,D). Together, these results with eGFP and β-galactosidase document very high frequencies of CD8+ T cells in muscle constitutively producing cognate antigen. Apoptosis, not failure of CD8+ T cells to expand or accumulate in sufficient numbers at the site of antigen production, was associated with prolonged survival of rAAV vector-transduced myocytes.
Analysis of CD8+ T cells in quadriceps muscle positive for β-galactosidase. (A) Enzymatic detection of β-galactosidase in rAAVβgal-injected (left) and contralateral (right) quadriceps muscle 168 days after vector administration. Bar represents 100 μm. (B) β-Galactosidase was quantified in muscle by antigen-capture ELISA 56 days after rAAVβ-gal inoculation. (C) Numbers represent the percentage of CD8+ T cells that costain with the H-2Kb βgal96-103 tetramer in spleen, liver and muscle of mice injected with rAAVβgal 56 days earlier. Plots gated as in Figure 1D. (D) Annexin V binding by H-2Kb βgal96-103 tetramer+ CD8+ T lymphocytes from quadriceps muscle, liver, and spleen 56 days after transduction with rAAVβgal. Numbers represent the percentage of tetramer+ cells that bind annexin V. Dot plots gated as in Figure 4A (right panel). Data represent 2 independent experiments each with tissues pooled from 6 mice.
Analysis of CD8+ T cells in quadriceps muscle positive for β-galactosidase. (A) Enzymatic detection of β-galactosidase in rAAVβgal-injected (left) and contralateral (right) quadriceps muscle 168 days after vector administration. Bar represents 100 μm. (B) β-Galactosidase was quantified in muscle by antigen-capture ELISA 56 days after rAAVβ-gal inoculation. (C) Numbers represent the percentage of CD8+ T cells that costain with the H-2Kb βgal96-103 tetramer in spleen, liver and muscle of mice injected with rAAVβgal 56 days earlier. Plots gated as in Figure 1D. (D) Annexin V binding by H-2Kb βgal96-103 tetramer+ CD8+ T lymphocytes from quadriceps muscle, liver, and spleen 56 days after transduction with rAAVβgal. Numbers represent the percentage of tetramer+ cells that bind annexin V. Dot plots gated as in Figure 4A (right panel). Data represent 2 independent experiments each with tissues pooled from 6 mice.
Discussion
In this study, we investigated why CD8+ T-cell responses fail to clear antigen-positive myocytes transduced with rAAV vectors. We observed limited focal inflammation in the transduced muscle, consistent with earlier findings by others.4,21 Nevertheless, assays to detect antigen-specific CD8+ T cells, including MHC tetramers for visualization of these effectors, provided direct evidence that they are primed. This result was unexpected given prolonged expression of model transgenes in muscle and suggested that a defect in CD8+ T-cell function or survival, rather than an absence from antigen-positive tissue, was more likely to account for failure of immune-mediated clearance. Indeed, that at least 10% to 20% of CD8+ T cells in muscle were specific for eGFP and β-galactosidase MHC class I epitopes 2 months after vector administration indicates that priming and accumulation of effectors at the site of antigen production is robust and probably not a factor in the failure to clear transduced myocytes.
Survival of CD8+ T cells in the face of ongoing antigen production has also been observed in mice persistently infected with viruses such as LCMV and polyoma virus.34,35 This inability to clear antigen-positive cells is caused at least in part by functional exhaustion of effector CD8+ T cells.28,36,37 We did not observe obvious defects in cytotoxic degranulation or IFN-γ production after antigen stimulation, at least for CD8+ T cells isolated from spleen or liver (Figure 3). Our results suggest that loss of function in tissues that are persistently antigen positive occurs by a potentially unique mechanism that involves apoptosis. Active culling of antigen-specific CD8+ T cells in rAAV vector-transduced muscle but not distant untransduced tissues like spleen and liver was unexpected. CD8+ T cells infiltrating transduced muscle almost universally bound annexin V, indicating an exquisite susceptibility to activation-induced death. Most muscle infiltrating CD8+ T cells failed to produce IFN-γ when stimulated with antigen, suggesting that upon entering the programmed death pathway, they could no longer target transgene-expressing myocytes.
The possibility that annexin V binding CD8+ T cells that no longer produce IFN-γ retain cytotoxic capability cannot be formally excluded. We consider this possibility very unlikely, however, because in other models of CD8+ T-cell anergy, highly differentiated effector functions such as cytotoxicity and IL-2 production are lost first.36 IFN-γ synthesis is most resistant to functional exhaustion and is usually the last effector activity to be lost before physical deletion of the cells commences.36 The observation that most CD8+ T cells infiltrating muscle bound annexin V and failed to produce IFN-γ suggests that this hierarchical process of functional impairment was complete and that the process of apoptosis leading to physical destruction was well under way. Whether apoptosis is the fate of all intramuscular rAAV vector-primed CD8+ T cells is unknown. It is noteworthy that a small fraction of the muscle-infiltrating cells were functional. It is most likely that they were recent immigrants that had not yet received a death signal. However, we cannot exclude the possibility that surviving antigen-specific CD8+ T cells are apoptosis-resistant and thus silenced by a second mechanism that does not lead to programmed death. Candidate pathways for negative regulation under these circumstances might include certain B7-family members such as programmed death 1 (PD-1) or cytotoxic T-lymphocyte attenuator-4 (CTLA-4).
Continuous apoptosis of CD8+ T cells at the site of transgene-expression suggests that there must be a mechanism for vigorous self-renewal. If CD8+ T cells primed by rAAV vectors are susceptible to antigen-driven apoptosis, then continuous replacement by low-level antigen-driven proliferation of effectors may be unlikely.38 The alternative is that CD8+ T-cell populations lost by antigen-driven apoptosis are continuously replaced by newly primed effectors, a mechanism that has been described for persistent polyoma virus infection of mice.39 Why CD8+ T cells primed by the rAAV vectors but not the rAd vector were susceptible to death at the site of antigen production is unknown. Features of the muscle microenvironment that determine the fate of tissue infiltrating CD8+ T cells need further study. rAd vectors elicit strong inflammatory signals in muscle40 that seem to be attenuated or absent in rAAV vector-treated animals.21,22,41 Inadequate costimulation during initial priming could predispose CD8+ T cells to apoptosis, possibly by enhancing death signaling via a tumor necrosis factor (TNF) superfamily member such as TNF-α, Fas (CD95), or the TNF-related apoptosis-inducing ligand (TRAIL).30 This possibility is illustrated by the observation that primed “helpless” CD8+ T cells are highly susceptible to TRAIL-mediated programmed death upon antigen re-stimulation.42 It is also possible that T regulatory cells play a role in localized death of muscle-infiltrating CD8+ T cells, perhaps by through a process of cytokine deprivation-induced apoptosis.43 Unraveling the mechanism(s) of CD8+ T-cell apoptosis may suggest approaches for modification of rAAV gene therapy vectors to reinforce signaling through death receptors or their ligands.
It should be emphasized that not all rAAV vector-encoded proteins expressed in muscle generate defective CD8+ T-cell immunity. For instance herpes simplex virus type 2 and influenza virus glycoproteins stimulate functional CD8+ T cells when produced in myocytes.44,45 At least in the case of the influenza hemagglutinin, priming of CD4+ and CD8+ cells was associated with rapid clearance of rAAV vector-transduced myofibers.45 It is not clear why in inbred mouse models the CD8+ T-cell response to a protein like influenza hemagglutinin effectively terminates antigen expression, whereas responses generated by eGFP, β-galactosidase, or the clinically relevant factor IX do not.3,4,6,7 Duration of transgene expression in tissues like muscle can be altered when proteins are retargeted from the cytoplasm to the plasma membrane of rAAV vector-transduced cells.23 It can also be modulated by rAAV vector dose, route of delivery, capsid serotype, and selection of genetic elements such as promoters that regulate the tissue specificity and level of protein production.41,46 Precisely how these factors might contribute to a persistent or transient pattern of transgene expression is poorly understood, but it is conceivable that they influence the priming and/or effector function(s) of CD8+ T cells. The consequence of manipulating these variables merits further study; the ability to engineer changes that select for functional versus impaired CD8+ T-cell populations could have a very practical application to gene therapy or vaccination where rAAV vectors are targeted to muscle.
In summary, these studies indicate that vector-encoded proteins containing MHC class I epitopes are processed for priming of CD8+ T cells, even when persistently expressed in muscle. This observation may be particularly relevant to diseases such as muscular dystrophy or hemophilia B, in which therapeutic proteins are potentially antigenic because germ-line coding sequences are deleted or modified by mutation. Indeed a single amino acid substitution can transform a human self-protein into a neoantigen capable of eliciting CD8+ T-cell immunity in subjects carrying the relevant MHC class I gene(s).47 Transient expression of a therapeutic factor IX gene in the rAAV vector-transduced liver of one human subject with hemophilia B suggests a role for host immunity in the outcome of gene therapy.14 Whereas attention has been focused on the AAV capsid as a target of an undesirable CD8+ T-cell response,14-18 our observations suggest that transgene-specific cellular immune responses should also be considered as a potential risk to success of gene transfer with this vector. Loss of function and programmed death by most tissue-infiltrating CD8+ T cells in our model would seem to argue against their direct participation in clearance of rAAV vector-transduced target cells. Nevertheless, there is convincing precedent for cytokine-mediated rescue of apoptotic T lymphocytes.48-51 Our findings suggest a potentially tenuous balance between ongoing death of effector CD8+ T cells and long-term survival of rAAV vector-transduced cells producing therapeutic proteins. That even transient salvage of a CD8+ T-cell response by cytokines like IL-2 produced during acute or chronic infection could undermine the effectiveness of gene therapy should be considered.
The online version of this article contains a data supplement.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 USC section 1734.
Acknowledgments
We gratefully acknowledge support from the National Institutes of Health Tetramer Facility for providing the H-2Kd eGFP200-208 and H-2Kb β-gal96-103 tetramers.
This work was supported by a US Public Health Service grant (5R01-AI06388-5) to C.M.W., a Ruth L. Kirshstein National Research Service Award (F31AI68609-2) to V.M.V., and by a C.J. Martin Fellowship from the National Health and Medical Research Council of Australia to D.G.B.
National Institutes of Health
Authorship
Contribution: V.M.V. designed and executed the experiments and wrote drafts of the manuscript; D.G.B. assisted with data interpretation and design of experiments; and C.M.W. designed experiments, interpreted data, and had overall responsibility for the writing of the manuscript.
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Correspondence: Christopher Walker, The Center for Vaccines and Immunity, The Research Institute at Nationwide Children's Hospital, 700 Children's Drive, Columbus, OH 43205; e-mail: christopher.walker@nationwidechildrens.org.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal