Abstract
Abstract 525
We studied cytogenetic risk grouping schemes to stratify AML patients into prognostically distinct subgroups for relapse free (RFS) and overall survival (OS) after an allogeneic hematopoietic stem cell transplantation (HSCT).
We retrospectively analyzed consecutive patients who underwent their first HSCT with a matched related donor (MRD) or cord blood (CB) at the University of Minnesota for AML in remission between January 1995 and December 2007. Patients were divided according to cytogenetic abnormalities based on the MRC, SWOG, CALGB, Dana-Farber (DF) and recently described monosomal karyotype (MK) classification schemes and study group was stratified based on first complete remission (CR1) and beyond (CR2+) at HSCT. Cox regression analysis evaluated the prognostic factors on OS and RFS.
212 patients were analyzed with a median age 45 years (range 18-68); 27 had evolved from MDS. Disease status was, CR1 (n=134) and CR2+ (n=78). Donors were MRD (n=105) and CB (n=107). Conditioning intensity was myeloablative (MA, n=118) and non-myeloablative (NMA, n=94). Cytogenetic classification based on MRC, SWOG, CALGB and DF was concordant in 131 patients (62%). Ten (5%), 89 (42%) and 32 (15%) patients were in favorable, intermediate/standard and adverse/unfavorable groups in all 4 classification schemes. Fifty-five patients (26%) were classified as unfavorable/adverse in one scheme and standard/intermediate in another. Sixteen patients (7%) were classified as unknown significance and 10 (5%) were excluded in at least one classification scheme. Eighteen of 23 MK+ patients (78%) and 14 of 78 MK-patients (18%) were classified as adverse/unfavorable in all other schemes. The remaining 5 MK+ (22%) and 64 MK- patients (82%) were classified inconsistently in the other schemes. Five year probabilities were: OS 37 % (95% CI % 29%-45%), RFS 54% (95% CI 45%-64%). Six mo and 2 year cumulative incidence of transplant related mortality were 21% (95% CI 16%-27%) and 29% (95% CI 23%-35%).
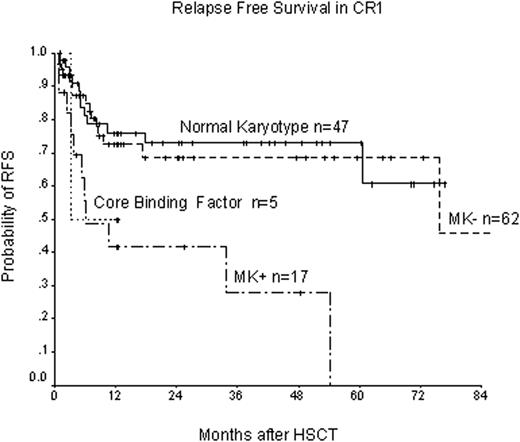
In multivariate analysis, after adjusting for age, conditioning intensity, disease status at HSCT, donor type and CMV status, only MK+ was associated with lower RFS in CR1 patients (HR=4.1, p=0.05). Cytogenetic classifications by the other 4 schemes were not predictive of RFS (SWOG HR=1.34 p=0.23, MRC HR=1.47, p=0.14, CALGB HR=1.43 p=0.15, DF HR=1.43 p=0.16). Median time to relapse was 6.1 mo for MK+ vs. 75.8 mo for MK- vs not reached for normal karyotype (NK) (Figure 1). In CR1, no covariates were associated with OS. In CR2+ patients, MK and CALGB predicted OS. MK+ (HR=2.93, p=0.04), MK- (HR=2.05, p=0.06) and NMA conditioning (HR=3.3, p=0.01) were associated with lower OS. All MK+ patients died within 3 years. CALGB adverse karyotype (HR=2.95, p=0.01) and NMA conditioning (HR=3.1, p=0.01) also associated with lower OS. All 5 classification schemes could predict RFS in CR2+. However, only MK could identify a very poor prognostic group, MK+ (HR=5.9, p<0.01, median RFS 2.5 mo) vs. a poor prognostic group, MK- (HR=2.0, p=0.06, median RFS 16.3 mo) (Figure 2).
HSCT in CR1 overcomes the poor prognosis associated with higher risk cytogenetic abnormalities. The MK classification can best identify a very poor prognostic group. In CR2+, HSCT particularly with NMA conditioning may not overcome the poor prognosis from cytogenetic subgroups. Among all classification schemes, MK can best predict outcome in CR1 and CR2+ patients.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.


This feature is available to Subscribers Only
Sign In or Create an Account Close Modal