Abstract
Glycoprotein VI (GPVI) mediates platelet activation on exposed subendothelial collagens at sites of vascular injury and thereby contributes to normal hemostasis, but also to the occlusion of diseased vessels in the setting of myocardial infarction or stroke. GPVI is an attractive target for antithrombotic therapy, particularly because previous studies have shown that anti-GPVI antibodies induce irreversible down-regulation of the receptor in circulating platelets by internalization and/or ectodomain shedding. Metalloproteinases of the a disintegrin and metalloproteinase (ADAM) family have been proposed to mediate this ectodomain shedding, but direct evidence for this is lacking. Here, we studied GPVI shedding in vitro and in vivo in newly generated mice with a megakaryocyte–specific ADAM10 deficiency and in Adam17ex/ex mice, which lack functional ADAM17. We demonstrate that GPVI cleavage in vitro can occur independently through either ADAM10 or ADAM17 in response to distinct stimuli. In contrast, antibody (JAQ1)–induced GPVI shedding in vivo occurred in mice lacking both ADAM10/ADAM17 in their platelets, suggesting the existence of a third GPVI cleaving platelet enzyme. This was supported by in vitro studies on ADAM10/ADAM17 double–deficient platelets. These results reveal that ectodomain shedding of GPVI can be mediated through multiple differentially regulated platelet–expressed proteinases with obvious therapeutic implications.
Introduction
At sites of vascular injury, the subendothelial extracellular matrix (ECM) becomes exposed to the flowing blood and triggers platelet adhesion and aggregation. Under high shear flow conditions, the initial contact is mediated by the interaction between collagen-bound von Willebrand factor (VWF) and the glycoprotein (GP)Ib-V-IX complex on the platelet surface. This interaction is transient and reduces the velocity of the cells and thereby enables interactions between the low-affinity platelet collagen receptor, glycoprotein VI (GPVI) and collagen, leading to platelet activation and subsequent firm adhesion and aggregation.1 GPVI is a type I transmembrane protein of approximately 68 kDa that is noncovalently associated with the FcRγ-chain,2-4 which represents the signaling subunit of the receptor complex.3,5 Ligand binding of GPVI results in phosphorylation of the immunoreceptor tyrosine–based activation motif (ITAM) of the FcRγ-chain, followed by a cascade of tyrosine phosphorylation steps involving the adapter linker of activated T cells (LAT) and leading to the activation of various effector molecules, including phospholipase (PL)Cγ2.6
GPVI-deficient patients7-9 and mice3,10,11 display defective platelet responses to collagen, but only a moderate bleeding tendency, making GPVI a promising antithrombotic target. We have previously shown that in vivo administration of monoclonal anti-GPVI antibodies (JAQ1, 2, 3) leads to down-regulation of the GPVI receptor in circulating murine platelets12,13 and long-term protection in models of arterial thrombosis and ischemic stroke.14-16 Such an antibody-induced loss of GPVI is also seen in human platelets of autoimmune patients who had developed anti-GPVI antibodies8,9 or in human platelets circulating in nonobese diabetic/severe combined immunodeficiency mice,17 confirming that anti-GPVI treatment may be a powerful strategy to specifically shut off this central activation pathway in platelets for a prolonged period of time while preserving other functions. The recent identification of GPVI as a central pathogenic factor in a model of rheumatoid arthritis18 indicates that the targeted down-regulation of GPVI may also have anti-inflammatory potential.
Down-regulation of GPVI from the platelet surface can occur through internalization12,13 or metalloproteinase-dependent ectodomain shedding.19,20 In vitro, this shedding can be triggered by the activation of metalloproteinases using carbonyl cyanide m-chlorophenylhydrazone (CCCP),19 which induces mitochondrial injury by uncoupling the oxidative phosphorylation, or in the presence of the calmodulin inhibitor W7,20 which blocks the association between calmodulin and GPVI.20 In contrast, JAQ-antibody–induced GPVI shedding occurs efficiently in vivo, but for unknown reasons not in vitro.12,13
To date, the identity of the GPVI sheddase(s) in platelets has not been firmly established. Platelets abundantly express sheddases of the a disintegrin and metalloproteinase (ADAM) family, most notably ADAM17 (also referred to as the tumor necrosis factor–converting enzyme, TACE) and ADAM10, but their physiologic function is not fully understood. Studies on GPVI-based synthetic peptides indicated a role for ADAM10 in GPVI cleavage,21 but direct evidence for this has been lacking. The analysis of mice lacking functional ADAM17 (TACEΔZn/ΔZn) revealed that this enzyme mediates the constitutive and agonist-induced shedding of GPIbα22 and is required for the agonist-induced shedding of GPV.23 Only recently, a role for ADAM10 in the shedding of GPV has been proposed,21 indicating that different ADAM family members can contribute to the shedding of individual surface receptors in platelets.
Given the central role of GPVI in platelet activation in thrombosis and hemostasis and the fact that targeted down-regulation of the receptor in platelets represents a potential antithrombotic regimen, a detailed understanding of the underlying mechanisms is warranted. Here, we studied GPVI regulation in mice lacking ADAM10, ADAM17, or both sheddases in platelets. We demonstrate that GPVI cleavage in vitro can occur through either ADAM10 or ADAM17 and that these events are differentially regulated. Furthermore, we provide evidence that a third protease exists in platelets that cleaves GPVI in vivo.
Methods
Mice
Animal studies were approved by the local authorities (Bezirksregierung Unterfranken). Adam10fl/fl mice were crossed with mice carrying the Cre recombinase under the platelet factor 4 (PF4) promoter.24 In this manuscript, Adam10fl/fl, PF4-Cre mice are referred to as Adam10−/−. Adam17ex/ex mice were generated as previously described.25
Reagents
Nonidet P-40 (Roche Diagnostics), 3,3,5,5-tetramethylbenzidine (EUROPA), ECL solution (Amersham), apyrase (grade 3), CCCP (Sigma-Aldrich), W7, N-ethylmaleimide (NEM), GM6001 (Calbiochem), EZ-Link sulfo-NHS-LC-biotin (Pierce), and horseradish peroxidase (HRP; Dianova) and fluorescein isothiocyanate (FITC)–conjugated streptavidin (DAKO) were used. Anti-ADAM10 antibody was purchased from Calbiochem. Other antibodies were generated and modified in our laboratories as described previously.26
Generation of Adam10fl/fl mice
BAC (bacterial artificial chromosome) clones containing the Adam10 region were verified by polymerase chain reaction using exon 2–specific primers and by physical mapping via Southern blotting (data not shown). The targeting vector was designed in the way that exon 2 is flanked by loxP sites to induce a site-specific deletion of Adam10 after recombination of the loxP sites mediated by a Cre recombinase. A neomycin cassette flanked by FRT sites was inserted, which was later removed after recombination by a Flp recombinase. The targeting vector was electroporated into Sv129-derived embryonic stem (ES) cells to obtain homologous recombination. Successfully targeted ES cells were injected into C57BL/6 blastocysts. Germ line transmission was obtained by backcrossing the resulting chimeric mice with C57BL/6 mice.
Generation of bone marrow chimeric mice
Recipient C57BL/6 mice of an age between 5 and 6 weeks were lethally irradiated with 10 Gy. Femur and tibia of donor mice were prepared. Bone marrow was flushed, and at least 4 million cells were intravenously injected into 1 recipient mouse.
Western blotting
Proteins of lysed platelets were separated by sodium dodecyl sulfate polyacrylamide gel electrophoresis (SDS-PAGE) and blotted onto polyvinylidene difluoride membranes. To monitor ADAM10 protein expression, after blocking, the membrane was incubated with an anti-ADAM10 overnight at 4°C. Goat anti–rabbit immunoglobulin G HRP (1 hour at room temperature; DAKO) and ECL were used for visualization.
To determine amounts of glycocalicin in plasma, equal volumes of plasma were used for analysis with an HRP-labeled anti-GPIb antibody.
Determination of platelet count, size, and surface protein expression
To measure platelet size and surface protein expression, heparinized blood was diluted 1:20 and stained for 15 minutes with saturating amounts of fluorophore-conjugated antibodies and immediately analyzed on a FACSCalibur (Becton Dickinson). Platelet volumina were determined in a Sysmex KX-21N cell counter (Sysmex Europe).
Platelet preparation
Mice were bled under isofluran anesthesia from the retro-orbital plexus. Blood was collected in a tube containing 20 U/mL heparin, and platelet-rich plasma (prp) was obtained by centrifugation twice at 300g for 6 minutes at room temperature (RT). For preparation of washed platelets, prp was washed twice at 1000g for 5 minutes at RT and the pellet was resuspended in modified Tyrodes-HEPES (N-2-hydroxyethyl-piperazone-N′2-ethanesulfonic acid) buffer (134mM NaCl, 0.34mM Na2HPO4, 2.9mM KCL, 12mM NaHCO3, 5mM HEPES, 1mM MgCl2, 5mM glucose, 0.35% bovine serum albumin, pH 7.4) in the presence of prostacyclin (0.1 μg/mL) and apyrase (0.02 U/mL). Platelets were then resuspended in modified Tyrodes-HEPES buffer containing 2mM CaCl2 and 0.02 U/mL apyrase.
Shedding of glycoproteins from the platelet surface
Washed platelets resuspended at a concentration of ∼ 1.5 × 109 platelets/mL in Tyrodes-HEPES buffer containing 2mM CaCl2 and 0.02 U/mL apyrase were treated for 1 hour with CCCP (100μM) or W7 (150μM) at 37°C and immediately analyzed on a FACSCalibur. Alternatively, platelets were incubated with NEM (2mM, 20 minutes, 37°C) in the presence or absence of the broad range metalloproteinase inhibitor GM6001 (100μM, 30 minutes, 37°C) and immediately analyzed on a FACSCalibur. Besides GPIbα, GPV, and GPVI levels, also GPIX levels and platelet size were determined as internal controls. Alternatively, samples were lysed with 1% Nonidet P-40 (NP-40) and prepared for Western blotting.
In vitro ELISA detection of cleaved GPVI
The experiments were performed as previously described.19 Washed platelets were resuspended in Tyrodes-HEPES buffer without CaCl2, containing PGI2 (0.1 μg/mL) and apyrase (0.02 U/mL). Biotinylated JAQ1 antibody (10 μg/mL) was added and incubated for 5 minutes at RT. After centrifugation, platelets were resuspended in Tyrodes-HEPES buffer containing 2mM CaCl2 and 0.02 U/mL apyrase. To induce GPVI shedding, the cells were then treated with CCCP (100μM) or W7 (150μM) for 1 hour at 37°C. Alternatively, platelets were incubated with NEM (2mM, 20 minutes, 37°C) in the presence or absence of the broad range metalloproteinase inhibitor GM6001 (100μM, 30 minutes, 37°C). Platelets were centrifuged and supernatants were incubated on JAQ3-coated (10 μg/mL) enzyme-linked immunosorbent assay (ELISA) plates for 1 hour at 37°C. After extensive washing, plates were incubated with HRP-labeled streptavidin for 45 minutes at 37°C and developed using TMB (3,3,5,5-tetramethylbenzidine). The reaction was stopped by the addition of 2N H2SO4, and absorbance at 450 nm was recorded on a Multiskan (Thermo Scientific).
Ex vivo GPVI shedding ELISA assay
Experiments were performed as described previously.27 Plasma of mice treated with 100 μg biotinylated JAQ1 or vehicle was incubated on JAQ3-coated (10 μg/mL) plates for 1 hour at 37°C and further processed as described in “In vitro ELISA detection of cleaved GPVI.”
Results
Generation of mice lacking ADAM10 in megakaryocytes/platelets
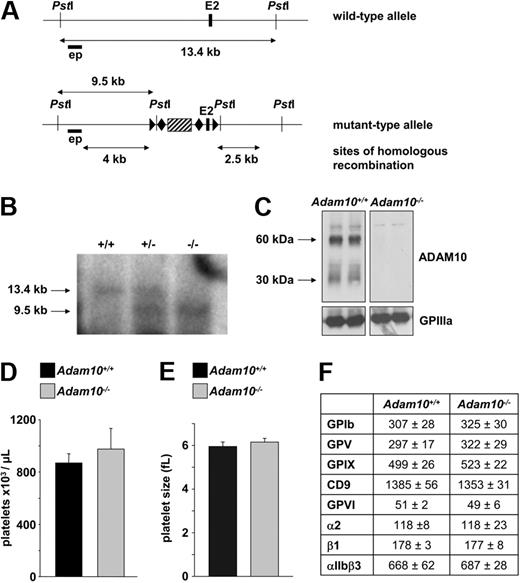
As previously reported,28 Adam10−/− mice die during embryogenesis at day 9.5 due to multiple defects, mainly in the cardiovascular system, the central nervous system, and the somites. To investigate the role of ADAM10 in platelet–receptor regulation, a vector was designed to conditionally target the Adam10 allele by inserting a neomycin resistance gene flanked by FRT sites and loxP sites that were essential for the removal of exon 2 (Figure 1A). The targeting vector was electroporated into Sv129-derived ES cells, and ES cells with successful homologous recombination were injected into C57BL/6 blastocysts. Germ line transmission of the targeted allele was obtained by crossing resulting chimeric mice with C57BL/6 mice. Heterozygous mutant mice were intercrossed, and Southern blot analyses (Figure 1B) revealed that wild-type, heterozygous, and homozygous mice were obtained in a Mendelian ratio (data not shown). The external probe (forward: 5′-CAGTGATTGGATTATGGCT-3′ and reverse: 5′-CCCTTGATTTCCACAGCTGG-3′) recognized a sequence in intron 1. Digestion with the PstI enzyme revealed band sizes for the wild-type allele of 13.4 kb and for the targeted allele of 9.5 kb. The neomycin resistance gene was excised by crossing the mutant mice with mice expressing the Flp recombinase. Adam10fl/fl mice were crossed with mice carrying Cre recombinase under the platelet factor 4 (PF4) promoter,24 leading to loss of Adam10 gene expression in megakaryocytes and platelets. Western blot analysis confirmed the absence of the Adam10 protein in platelets from Adam10fl/fl, PF4-Cre mice (below referred to as Adam10−/− mice; Figure 1C). Platelet count and size and the expression of prominent platelet surface proteins were unaltered in Adam10−/− mice, compared with wild-type controls (Figure 1D-F). This demonstrates that ADAM10 is dispensable for normal platelet production, and it does not apparently represent a constitutive sheddase of the tested platelet surface receptors.
Generation of mice with a megakaryocyte-specific ADAM10 deficiency. (A) The scheme depicts detection of Adam10 wild-type and floxed alleles. The external probe (black horizontal bar) recognizes a sequence upstream of exon 2. Exon 2 is represented as a black vertical bar. The wild-type band between 2 PstI sites is 13.4 kb, whereas the floxed band recognized by the external probe is 9.5 kb. The region used for homologous recombination is indicated. Striped black box: neomycin resistance gene. ▶: lox P site; ♦: FRT site. (B) Southern blot analysis from tail DNA of wild-type (+/+), conditionally targeted heterozygous (+/−), and conditionally targeted homozygous (−/−) mice. − indicates the floxed allele. (C) Western blot of platelet lysates from control and Adam10fl/fl, PF4-Cre mice. Whole platelet proteins were separated by SDS-PAGE and immunoblotted with an anti-ADAM10 antibody. Bands at 60 kDa are the mature protein, whereas bands at 30 kDa show the degraded protein. GPIIIa was used as a loading control. Flow cytometric analysis of platelet count (D) and platelet size (E). (F) Protein expression: platelets were stained with the indicated fluorophore-labeled antibodies for 15 minutes and analyzed directly. (F) Platelet size was determined in a Sysmex cell counter.
Generation of mice with a megakaryocyte-specific ADAM10 deficiency. (A) The scheme depicts detection of Adam10 wild-type and floxed alleles. The external probe (black horizontal bar) recognizes a sequence upstream of exon 2. Exon 2 is represented as a black vertical bar. The wild-type band between 2 PstI sites is 13.4 kb, whereas the floxed band recognized by the external probe is 9.5 kb. The region used for homologous recombination is indicated. Striped black box: neomycin resistance gene. ▶: lox P site; ♦: FRT site. (B) Southern blot analysis from tail DNA of wild-type (+/+), conditionally targeted heterozygous (+/−), and conditionally targeted homozygous (−/−) mice. − indicates the floxed allele. (C) Western blot of platelet lysates from control and Adam10fl/fl, PF4-Cre mice. Whole platelet proteins were separated by SDS-PAGE and immunoblotted with an anti-ADAM10 antibody. Bands at 60 kDa are the mature protein, whereas bands at 30 kDa show the degraded protein. GPIIIa was used as a loading control. Flow cytometric analysis of platelet count (D) and platelet size (E). (F) Protein expression: platelets were stained with the indicated fluorophore-labeled antibodies for 15 minutes and analyzed directly. (F) Platelet size was determined in a Sysmex cell counter.
ADAM10 is essential for GPVI shedding triggered by calmodulin inhibition
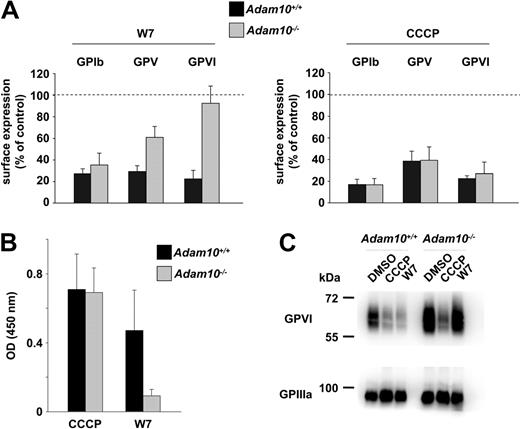
We have previously shown that GPVI can be down-regulated from the platelet surface by internalization and proteolytic cleavage of the receptor.12,13 Furthermore, we19 and others20,21 have demonstrated that shedding of GPVI is controlled by metalloproteinases, and ADAM10 has been proposed to be involved in this process based on the observation that this enzyme cleaved GPVI-related peptides.21 To test this hypothesis directly, Adam10−/− and control platelets were treated with the calmodulin inhibitor, W7 (150μM, 1 hour, 37°C), which has previously been shown to induce shedding of the GPIbα, GPV, and GPVI.20,21 This treatment resulted in virtually complete shedding of all 3 receptors in wild-type platelets, as shown by flow cytometric analysis (Figure 2A). The residual expression rate (∼20%) of the analyzed proteins was further decreased when the experiment was performed with longer incubation times (3 hours, data not shown). Different results were obtained with Adam10−/− platelets. While GPIbα cleavage occurred to the same extent (and with the same kinetics) as in wild-type platelets, cleavage of GPV was significantly reduced and GPVI shedding was completely abrogated in the absence of ADAM10. ELISA measurements27 confirmed the absence of cleaved GPVI in the supernatant of W7-treated Adam10−/− platelets, whereas strong signals were obtained with wild-type controls (Figure 2B). Finally, Western blot analyses confirmed the loss of intact GPVI in W7-treated wild-type, but not Adam10−/−, platelets (Figure 2C). These results provided the first direct evidence that ADAM10 is essential for GPVI shedding in response to calmodulin inhibition and support previous findings by Gardiner et al, who predicted ADAM10 to be a GPVI sheddase in platelets.21
W7-induced GPVI shedding is abrogated in Adam10−/− platelets. (A) Washed platelets were treated with the indicated reagents (W7: 150μM, 1 hour at 37°C; CCCP: 100μM, 1 hour at 37°C), stained with a fluorophore-labeled antibody recognizing the indicated glycoproteins, and analyzed on a FACSCalibur. (B) Washed platelets were incubated with biotinylated JAQ1 and then treated with CCCP (100μM) or W7 (150 μM) for 1 hour at 37°C. Supernatants were applied on a JAQ3-coated ELISA plate, and GPVI-JAQ1biotin complexes were detected with HRP-conjugated streptavidin. (C) Western blot detection of intact GPVI (JAQ1-HRP) in CCCP (100μM), W7 (150μM), or vehicle-treated platelets. GPIIIa was used as a loading control. Results of experiments in panels A and B are mean ± SD (n = 4 mice per group, representative for 3 individual experiments).
W7-induced GPVI shedding is abrogated in Adam10−/− platelets. (A) Washed platelets were treated with the indicated reagents (W7: 150μM, 1 hour at 37°C; CCCP: 100μM, 1 hour at 37°C), stained with a fluorophore-labeled antibody recognizing the indicated glycoproteins, and analyzed on a FACSCalibur. (B) Washed platelets were incubated with biotinylated JAQ1 and then treated with CCCP (100μM) or W7 (150 μM) for 1 hour at 37°C. Supernatants were applied on a JAQ3-coated ELISA plate, and GPVI-JAQ1biotin complexes were detected with HRP-conjugated streptavidin. (C) Western blot detection of intact GPVI (JAQ1-HRP) in CCCP (100μM), W7 (150μM), or vehicle-treated platelets. GPIIIa was used as a loading control. Results of experiments in panels A and B are mean ± SD (n = 4 mice per group, representative for 3 individual experiments).
Interestingly, however, a different picture emerged when receptor shedding was induced by the mitochondrial damage reagent, CCCP.22,23 Under these conditions, wild-type and Adam10−/− platelets displayed comparable down-regulation of GPIbα, GPV, and GPVI (Figure 2A). The strong cleavage of GPVI in wild-type and mutant platelets was confirmed by ELISA detection of the released GPVI-ectodomain (Figure 2B), and the virtually complete absence of intact GPVI in the platelet pellet was revealed by Western blot (Figure 2C). These results demonstrated that ADAM10 cleaves GPVI in the presence of a calmodulin inhibitor, but not when shedding is induced through mitochondrial damage.19
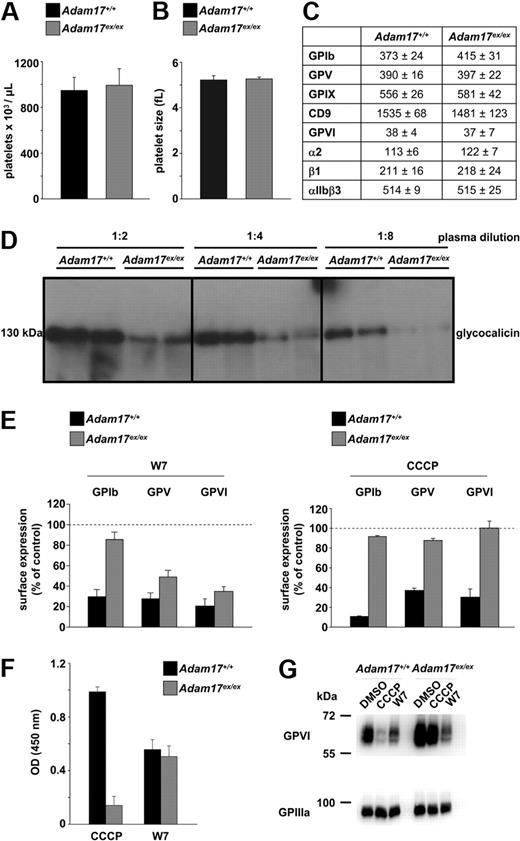
Mitochondrial damage–induced GPVI cleavage is mediated by ADAM17
As ADAM10 was not required for the proteolytic cleavage of GPVI in response to mitochondrial damage, we next tested a possible role for ADAM17 in this process. ADAM17 is a well-described sheddase of GPIbα22,29 and involved in the release of GPV from the platelet surface.23 Mice lacking functional ADAM17 die between day 17.5 of embryonic development and birth.30,31 Therefore, we capitalized on ADAM17-deficient mice, which were generated by the EXITS (exon-induced translational stop) approach, where a new exon within the Adam17 gene was introduced, which starts with an in-frame translational stop codon.25 This strategy enables the study of ADAM17 function in viable adult mice (below referred to as Adam17ex/ex mice), because the new exon was used in 95% of the Adam17 mRNA of Adam17ex/ex mice, resulting in a dramatic loss of the protein in all cell types. The phenotypic defects of these mice, which were born with a reduced birth rate (heterozygous mating: 11.9% of Adam17ex/ex mice), resembled those of Adam17−/− mice.25 To restrict the lack of ADAM17 to the hematopoietic system, we generated bone marrow chimeric (BMc) Adam17ex/ex mice, which were subsequently used for all experiments. Adam17ex/ex BMc mice had normal platelet counts (Figure 3A), and platelet size was comparable to that in BMc control mice (Figure 3B). Surface expression of prominent platelet membrane proteins was determined by flow cytometry in washed blood and yielded no significant differences between wild-type and mutant platelets (Figure 3C). However, when washed platelets were incubated in Tyrodes-HEPES buffer containing 2mM CaCl2 for 1 hour at 37°C, a significant decrease in GPIbα expression was detected in control, but not Adam17ex/ex, platelets (GPIb expression, mean fluorescence intensity: control: 292 ± 59; Adam17ex/ex: 457 ± 24; P < .001), confirming the proposed function of ADAM17 in GPIbα shedding in in vitro stored platelets.22 Furthermore, glycocalicin levels were profoundly reduced in plasma of Adam17ex/ex mice, compared with control, confirming that ADAM17 constitutively releases GPIbα from the platelet surface in vivo22 (Figure 3D; densitometric quantification of plasma glycocalicin in %: control 100 ± 16.5, Adam17ex/ex 22.9 ± 6.4). Also, CCCP- or W7-induced GPIbα shedding was virtually abolished in Adam17ex/ex platelets, confirming that these cells lack functional Adam17 (Figure 3E). Interestingly, down-regulation of both GPV and GPVI was only slightly affected in Adam17ex/ex platelets in response to W7 but almost completely abolished in response to CCCP. The stimulus-specific lack of GPVI shedding in Adam17ex/ex platelets was confirmed by the absence of cleaved GPVI in the supernatant of CCCP-treated Adam17ex/ex platelets (Figure 3F), whereas intact GPVI was still found in platelet lysates, as shown by immunoblotting (Figure 3G). These findings revealed the differential regulation of GPVI ectodomain shedding by ADAM10 or ADAM17 in response to specific stimuli in vitro.
CCCP-induced GPVI shedding is abolished in Adam17ex/ex platelets. Platelet count (A) and size (B) in Adam17ex/ex BMc and control mice. (C) Surface protein expression was determined by flow cytometry. Platelets were stained with the indicated fluorophore-labeled antibodies for 15 minutes and analyzed directly. (D) Glycocalicin levels in plasma were determined by Western blot. (E) Washed platelets were treated with the indicated reagents (W7: 150μM, 1 hour at 37°C; CCCP: 100μM, 1 hour at 37°C), stained with the indicated fluorophore-labeled antibody, and analyzed on a FACSCalibur. (F) Washed platelets were incubated with biotinylated JAQ1 and then treated with CCCP (100μM) or W7 (150μM) for 1 hour at 37°C. Supernatants were applied on a JAQ3-coated ELISA plate, and GPVI-JAQ1biotin complexes were detected with HRP-conjugated streptavidin. (G) Western blot detection of intact GPVI (JAQ1-HRP) in CCCP (100μM), W7 (150μM), or vehicle-treated platelets. GPIIIa was used as a loading control. Results of experiments (A-C and E-F) are mean ± SD (n = 4 mice per group, representative of 3 individual experiments).
CCCP-induced GPVI shedding is abolished in Adam17ex/ex platelets. Platelet count (A) and size (B) in Adam17ex/ex BMc and control mice. (C) Surface protein expression was determined by flow cytometry. Platelets were stained with the indicated fluorophore-labeled antibodies for 15 minutes and analyzed directly. (D) Glycocalicin levels in plasma were determined by Western blot. (E) Washed platelets were treated with the indicated reagents (W7: 150μM, 1 hour at 37°C; CCCP: 100μM, 1 hour at 37°C), stained with the indicated fluorophore-labeled antibody, and analyzed on a FACSCalibur. (F) Washed platelets were incubated with biotinylated JAQ1 and then treated with CCCP (100μM) or W7 (150μM) for 1 hour at 37°C. Supernatants were applied on a JAQ3-coated ELISA plate, and GPVI-JAQ1biotin complexes were detected with HRP-conjugated streptavidin. (G) Western blot detection of intact GPVI (JAQ1-HRP) in CCCP (100μM), W7 (150μM), or vehicle-treated platelets. GPIIIa was used as a loading control. Results of experiments (A-C and E-F) are mean ± SD (n = 4 mice per group, representative of 3 individual experiments).
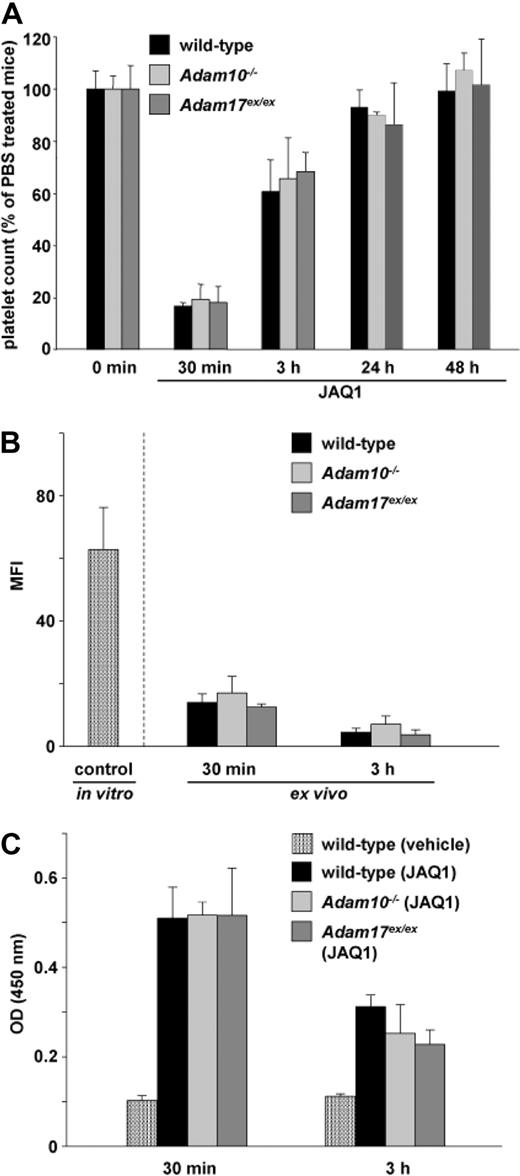
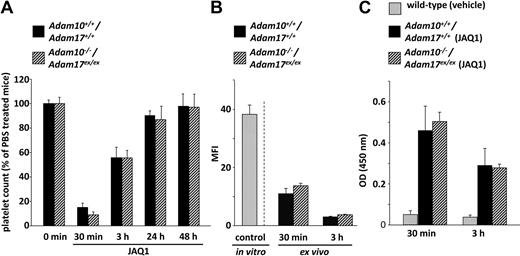
Unaltered antibody–induced GPVI ectodomain shedding in vivo in Adam10−/− and Adam17ex/ex mice
To test the roles of ADAM10 and ADAM17 in JAQ-antibody–induced GPVI shedding and the associated transient thrombocytopenia, wild-type and mutant mice were treated with biotinylated JAQ1,12,13 and platelet counts, GPVI surface expression, and cleaved GPVI levels in plasma were measured after 30 minutes and 3 hours. We have previously demonstrated that the “classical” GPVI signaling pathway via LAT and PLCγ2 is required for the induction of receptor shedding and the transient drop of the platelet count after JAQ-antibody injection, but it is unclear whether these 2 events are mechanistically linked.27 Interestingly, JAQ1 injection resulted in comparable transient thrombocytopenia in Adam10−/−, Adam17ex/ex BMc, and the respective control mice (Figure 4A) with a maximal drop to approximately 20% of vehicle-treated mice after 30 minutes and a return to normal levels at later time points (Figure 4A). Furthermore, GPVI was down-regulated from the platelet surface in all mice (Figure 4B), and this occurred through ectodomain shedding as similar levels of cleaved GPVI were detected in plasma of wild-type and mutant animals by ELISA 30 minutes and 3 hours after antibody injection (Figure 4C). This ELISA system yielded no significant signal in the plasma of mice genetically deficient in GPVI, confirming previous results.27 Together, these results demonstrated in vivo that JAQ1-induced GPVI shedding, and the associated transient thrombocytopenia is unaltered in the absence of ADAM10 or ADAM17, suggesting that neither ADAM10 nor ADAM17 alone is the exclusive sheddase for GPVI in vivo.
GPVI is cleaved in Adam10−/− and Adam17ex/ex mice in vivo. Control and mutant mice were injected intravenously with 100 μg of biotinylated anti-GPVI (JAQ1) antibody. Flow cytometric analysis of platelet count (A) and GPVI surface expression (B; indirectly: streptavidin-FITC) was performed. As a positive control in (B), wild-type platelets from untreated mice were incubated with 10 μg/mL biotinylated-JAQ1 in vitro and stained with streptavidin-FITC. (C) Mice were injected with 100 μg biotinylated-JAQ1, and plasma was collected at the indicated time points. Levels of GPVI-JAQ1biotin complexes in plasma were determined by ELISA. Results of all experiments are mean ± SD (n = 4 mice per group, representative for 3 individual experiments).
GPVI is cleaved in Adam10−/− and Adam17ex/ex mice in vivo. Control and mutant mice were injected intravenously with 100 μg of biotinylated anti-GPVI (JAQ1) antibody. Flow cytometric analysis of platelet count (A) and GPVI surface expression (B; indirectly: streptavidin-FITC) was performed. As a positive control in (B), wild-type platelets from untreated mice were incubated with 10 μg/mL biotinylated-JAQ1 in vitro and stained with streptavidin-FITC. (C) Mice were injected with 100 μg biotinylated-JAQ1, and plasma was collected at the indicated time points. Levels of GPVI-JAQ1biotin complexes in plasma were determined by ELISA. Results of all experiments are mean ± SD (n = 4 mice per group, representative for 3 individual experiments).
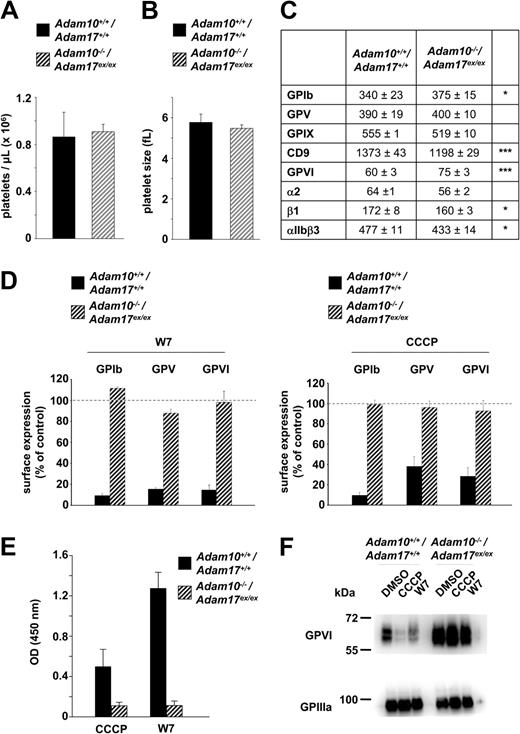
Analysis of Adam10−/−/Adam17ex/ex double-mutant platelets in vitro
Adam10fl/fl, PF4-Cre/Adam17wt/ex mice were intercrossed to obtain double-deficient mice. Adult mice deficient in both metalloproteinases were rarely obtained (frequency: 2.5%). Therefore, bone marrow of double mutant mice was transferred into lethally irradiated recipient C57BL/6 mice, and the mice were analyzed after 8 weeks. Platelet counts (Figure 5A) and size (Figure 5B) were normal, but expression levels of different surface proteins were slightly altered, compared with controls (Figure 5C). Most notably, surface levels of GPVI were modestly, but consistently, increased in the double mutant cells. Treatment of Adam10−/−/ Adam17ex/ex platelets with W7 or CCCP failed to induce significant down-regulation of GPIbα, GPV, or GPVI (Figure 5D), which was expected, based on the results obtained with the single mutant mice (Figures 2–3). In line with this, no cleaved GPVI was detectable by ELISA in the supernatant of W7- or CCCP-treated double mutant platelets (Figure 5E), but unchanged levels of intact GPVI were found in platelet lysates (Figure 5F). These results confirm the results obtained from the analysis of the single-deficient mice, and demonstrate that ADAM10 and ADAM17 are the only in vitro sheddases of GPIbα, GPV, and GPVI under these conditions.
GPVI shedding in Adam10−/−/Adam17ex/ex platelets in vitro. Platelet count (A) and size (B) in Adam10−/−/Adam17ex/ex BMc and control mice. (C) Surface protein expression was determined by flow cytometry. Platelets were stained with the indicated fluorophore-labeled antibodies for 15 minutes and analyzed directly. *P < .05; ***P < .001). (D) Washed platelets were treated with the indicated reagents (W7: 150μM, 1 hour at 37°C; CCCP: 100μM, 1 hour at 37°C), stained with a fluorophore-labeled antibody recognizing the indicated glycoprotein, and analyzed in a flow cytometer. (E) Washed platelets were incubated with the biotinylated anti-GPVI antibody, JAQ1, and then treated with CCCP (100μM) or W7 (150μM) for 1 hour at 37°C. Supernatant was collected and applied on a JAQ3-coated ELISA plate and incubated with HRP-conjugated streptavidin. (F) Washed platelets were treated with CCCP (100μM) or W7 (150μM) for 1 hour at 37°C and immediately lysed with 1% Nonidet P-40. The lysates were separated on a SDS-PAGE and incubated with an HRP-labeled anti-GPVI antibody. GPIIIa was used as a loading control. Results of experiments (A-E) are mean ± SD (n = 4 mice per group, representative for 3 individual experiments).
GPVI shedding in Adam10−/−/Adam17ex/ex platelets in vitro. Platelet count (A) and size (B) in Adam10−/−/Adam17ex/ex BMc and control mice. (C) Surface protein expression was determined by flow cytometry. Platelets were stained with the indicated fluorophore-labeled antibodies for 15 minutes and analyzed directly. *P < .05; ***P < .001). (D) Washed platelets were treated with the indicated reagents (W7: 150μM, 1 hour at 37°C; CCCP: 100μM, 1 hour at 37°C), stained with a fluorophore-labeled antibody recognizing the indicated glycoprotein, and analyzed in a flow cytometer. (E) Washed platelets were incubated with the biotinylated anti-GPVI antibody, JAQ1, and then treated with CCCP (100μM) or W7 (150μM) for 1 hour at 37°C. Supernatant was collected and applied on a JAQ3-coated ELISA plate and incubated with HRP-conjugated streptavidin. (F) Washed platelets were treated with CCCP (100μM) or W7 (150μM) for 1 hour at 37°C and immediately lysed with 1% Nonidet P-40. The lysates were separated on a SDS-PAGE and incubated with an HRP-labeled anti-GPVI antibody. GPIIIa was used as a loading control. Results of experiments (A-E) are mean ± SD (n = 4 mice per group, representative for 3 individual experiments).
Lack of ADAM10 and ADAM17 in platelets does not prevent GPVI shedding in vivo
To test the effect of ADAM10/ADAM17 double deficiency on JAQ1-induced GPVI ectodomain shedding and associated thrombocytopenia, double mutant BMc mice were injected with biotinylated JAQ1, and platelet counts, GPVI surface expression, and cleaved GPVI levels in plasma were determined. JAQ1 induced comparable transient thrombocytopenia in wild-type and double mutant mice (Figure 6A). Remarkably, GPVI was down-regulated from the surface of Adam10−/−/Adam17ex/ex platelets with the same kinetics and to the same extent as in wild-type controls (Figure 6B), and similar levels of cleaved GPVI were detected in plasma of both groups of mice (Figure 6C). Thus, antibody-induced ectodomain shedding of GPVI in vivo occurs independently of the 2 major sheddases responsible for shedding of the receptor in vitro.
Unaltered JAQ1-induced GPVI shedding in Adam10−/−/Adam17ex/ex double mutant mice. Control and Adam10−/−/Adam17ex/ex BMc mice were injected intravenously with 100 μg JAQ1biotin. Flow cytometric analysis of platelet count (A) and GPVI expression (B; indirectly: streptavidin-FITC) was performed. As a positive control in (B), wild-type platelets from untreated mice were incubated with 10 μg/mL biotinylated-JAQ1 and stained with streptavidin-FITC. (C) Mice were injected with 100 μg biotinylated-JAQ1, and plasma was collected at the indicated time points. GPVI levels in plasma were determined by ELISA. Results of all experiments are mean ± SD (n = 4 mice per group, representative for 3 individual experiments).
Unaltered JAQ1-induced GPVI shedding in Adam10−/−/Adam17ex/ex double mutant mice. Control and Adam10−/−/Adam17ex/ex BMc mice were injected intravenously with 100 μg JAQ1biotin. Flow cytometric analysis of platelet count (A) and GPVI expression (B; indirectly: streptavidin-FITC) was performed. As a positive control in (B), wild-type platelets from untreated mice were incubated with 10 μg/mL biotinylated-JAQ1 and stained with streptavidin-FITC. (C) Mice were injected with 100 μg biotinylated-JAQ1, and plasma was collected at the indicated time points. GPVI levels in plasma were determined by ELISA. Results of all experiments are mean ± SD (n = 4 mice per group, representative for 3 individual experiments).
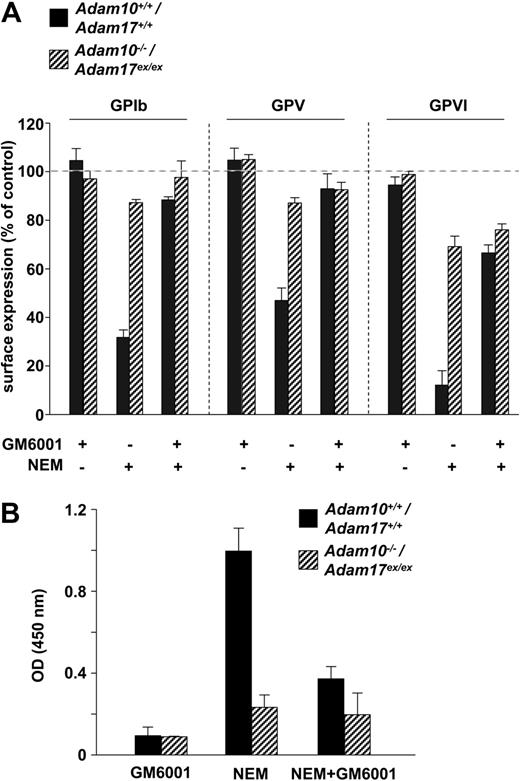
Evidence for a third GPVI cleaving GM6001-insensitive protease in platelets
The experiment described in the previous paragraph suggested that GPVI can be shed from the platelet surface by ADAM10, ADAM17, and a third, yet undefined, protease. Because JAQ-induced GPVI shedding occurs only in vivo but not in vitro,12,13 it appeared possible that this third protease may not be present in platelets, but in other compartments. To test for the presence of an additional GPVI cleaving activity in platelets, washed wild-type and Adam10−/−/Adam17ex/ex platelets were treated with the thiol-modifying reagent, NEM (2mM, 20 minutes, 37°C), which directly activates surface (metallo)proteinases.32 This treatment resulted in profound cleavage of GPIbα, GPV, and GPVI in wild-type controls. Shedding of GPIbα and GPV was almost completely blocked in the presence of the broad range metalloproteinase inhibitor GM6001 (100μM, 30 minutes, 37°C; Figure 7A). Interestingly, GM6001 only partially inhibited NEM-induced shedding of GPVI. In contrast, while shedding of GPIbα and GPV was virtually abolished in double mutant platelets, partial down-regulation of GPVI was detected by flow cytometry, and significant amounts of cleaved GPVI ectodomain were detectable in the supernatant of the cells (Figure 7A-B). This residual shedding of GPVI in double mutant platelets was not blocked in the presence of GM6001. These results suggested the existence of a GPVI cleaving protease in ADAM10/ADAM17 double-deficient platelets that is not sensitive to GM6001 inhibition.
Evidence for a third GPVI-cleaving protease in platelets that is insensitive to GM6001 inhibition. (A) Washed platelets were treated with NEM (2mM, 20 minutes, 37°C) in the presence or absence of GM6001 (100μM, 30 minutes, 37°C), stained with a fluorophore-labeled antibody recognizing the indicated glycoprotein, and analyzed in a flow cytometer. (B) Washed platelets were incubated with the biotinylated anti-GPVI antibody, JAQ1, and then treated with NEM (2mM, 20 minutes, 37°C) in the presence or absence of GM6001 (preincubation: 100μM, 30 minutes, 37°C). Supernatant was collected and applied on a JAQ3-coated ELISA plate and incubated with HRP-conjugated streptavidin. Results of experiments are mean ± SD (n = 4 mice per group, representative for 3 individual experiments).
Evidence for a third GPVI-cleaving protease in platelets that is insensitive to GM6001 inhibition. (A) Washed platelets were treated with NEM (2mM, 20 minutes, 37°C) in the presence or absence of GM6001 (100μM, 30 minutes, 37°C), stained with a fluorophore-labeled antibody recognizing the indicated glycoprotein, and analyzed in a flow cytometer. (B) Washed platelets were incubated with the biotinylated anti-GPVI antibody, JAQ1, and then treated with NEM (2mM, 20 minutes, 37°C) in the presence or absence of GM6001 (preincubation: 100μM, 30 minutes, 37°C). Supernatant was collected and applied on a JAQ3-coated ELISA plate and incubated with HRP-conjugated streptavidin. Results of experiments are mean ± SD (n = 4 mice per group, representative for 3 individual experiments).
Discussion
GPVI is the central platelet collagen receptor and has been established as a promising antithrombotic1,33 and anti-inflammatory18 target, particularly because the receptor can be irreversibly down-regulated from the surface of circulating platelets in vivo, resulting in a “GPVI knockout-like” phenotype12,13 and profound antithrombotic protection in vivo.15,16,34 However, antibody-induced GPVI depletion is associated with a transient, but profound, drop in platelet counts and increased bleeding times due to a diminished protease-activated receptor activity in early phases upon treatment.17,35 An alternative approach to down-regulate GPVI in circulating platelets could be the selective activation of the cleaving enzyme. In this study, we demonstrated that GPVI can be down-regulated from the platelet surface by ectodomain shedding through different proteases that are differentially activated in response to distinct stimuli. This unexpected finding indicates a rather complex regulation of GPVI surface expression under (patho-)physiologic conditions and reveals different potential molecular targets that may allow therapeutic down-regulation of the receptor in patients at thrombotic risk. We used newly generated mice with a megakaryocyte/platelet-specific ADAM10 deficiency and the recently described Adam17ex/ex mouse line25 alone and in combination to reveal essential functions of these metalloproteinases in GPVI shedding in response to distinct stimuli. Furthermore, our data suggest the existence of a third GPVI cleaving, GM6001-insensitive enzyme in platelets.
Previous studies have shown that GPVI is down-regulated in platelets by a metalloproteinase-dependent mechanism,19,20,36 but the identity of the responsible protease has remained elusive. The observation that ADAM17-mediated shedding of GPIbα occurs in response to platelet stimulation with thrombin, collagen-related peptide (CRP), or the protein kinase C (PKC) activator, phorbol 12-myristate 13-acetate (PMA), whereas GPVI levels remain unchanged under these conditions, led to the assumption that ADAM17 is not responsible for GPVI shedding.19 In later studies, it was speculated that ADAM10 may be the GPVI sheddase,29 and indirect experimental evidence in support of this was provided.21 We here show that both ADAM17 and ADAM10 are efficient GPVI sheddases that cleave the receptor independently of each other in response to distinct stimuli. Interestingly, CCCP treatment induced GPVI shedding by an ADAM17-dependent mechanism (Figure 3), although other ADAM17 activating stimuli (eg, CRP, thrombin, PMA) have no such effect. This demonstrates that agonist-induced activation of ADAM17 is not sufficient to induce GPVI cleavage and that additional factors determine whether or not shedding of this receptor occurs.
This is further supported by the observation that calmodulin inhibition by W7, which is known to activate ADAM17-dependent shedding of GPIbα, did not induce ADAM17-dependent shedding of GPVI (Figure 3). However, under these conditions, shedding still occurred but in a strictly ADAM10-dependent manner (Figure 2), which is in line with the findings of Gardiner et al, who showed in their cleavage studies on GPVI-based synthetic peptides that ADAM10 is the GPVI sheddase using W7.21 This is the first demonstration that GPVI can be down-regulated in vitro by 2 different metalloproteinases, ADAM10 and ADAM17, under different experimental conditions. It has previously been shown that certain substrates can be cleaved by more than 1 sheddase, such as CX3CL-1, the cellular prion protein (PrP), the amyloid precursor protein (APP),37-41 and the interleukin-6 receptor,42 and that these proteins are processed by both ADAM10 and ADAM17. It was described that CX3CL-1, PrP, and APP are differentially regulated by ADAM10 as the constitutive sheddase and ADAM17 after stimulation with PMA.38-41 To understand these processes in more detail, it will be important to dissect the molecular pathways involved in ADAM10/17 activation in platelets. Recent studies showed that ADAM17 activation is dependent on p38 mitogen-activated protein kinase signaling.43,44
Our data indicate that besides ADAM10 and ADAM17, a third GPVI cleaving, GM6001-insensitive enzyme is present in platelets (Figure 7). While the potential of this unknown protease to cleave GPVI in vitro (in the presence of the thiol-modifying reagent, NEM) was limited, our studies on JAQ1-treated Adam10−/−/Adam17ex/ex mice suggest that this enzyme very efficiently mediates the antibody-induced shedding of GPVI in vivo (Figure 6). Moreover, both the kinetics and extent of JAQ1-induced GPVI shedding in the double mutant mice were indistinguishable from the wild-type control, indicating that neither ADAM10 nor ADAM17 play a major role in this process. This was surprising given the pivotal role of these 2 enzymes in the in vitro shedding of GPVI. These findings are in line with recent studies by Wang and coworkers, who provided evidence that shedding of the adhesion receptor, L-selectin, during late stages of neutrophil activation occurs in mice lacking its principal sheddase, ADAM17, in hematopoietic cells. Based on the observation that this shedding was still detectable in the presence of a selective ADAM10 inhibitor, the authors concluded that another protease mediates this cleavage.45 A possible alternative explanation could be that receptor shedding occurs in trans, that is, by ADAM10 and/or ADAM17 expressed in other cell types. Such a mechanism has been shown in vitro in heterologous cell systems.46 We cannot completely exclude this possibility, because we used mice with a platelet-specific ADAM10 deficiency and mice lacking functional ADAM17 only in the hematopoietic system. However, given the extremely high numbers of platelets in the blood stream of mice (∼ 109/mL) and the very rapid time course and high efficiency of antibody-induced GPVI shedding in vivo (within minutes), we consider this very unlikely.
One candidate enzyme to mediate GPVI shedding could be ADAM9 because it is widely expressed, highly conserved between species, and a catalytically active metalloproteinase. It has been suggested that ADAM9 could have a potential function in the shedding of receptors.47 However, platelets express many other proteases that could potentially mediate GPVI cleavage, including matrix metalloproteinases, which also contain a regulatory Cys switch and hence can be activated by NEM.32,48 However, both ADAM9 and platelet matrix metalloproteinases are known to be sensitive to GM6001 inhibition in other experimental settings, making it unlikely that one of them accounts for the observed NEM-induced GPVI shedding in ADAM10/ADAM17 double-deficient platelets in vitro.
Interestingly, in contrast to other antibodies that are able to induce down-regulation of their substrate via ectodomain shedding in vitro,49,50 JAQ-induced GPVI down-regulation in murine platelets does not occur in vitro, but very efficiently in vivo,12,13 and similar observations have been reported for human platelets in a nonobese diabetic/severe combined immunodeficiency mouse model.17 This indicates that the antibody-induced activation of this GPVI cleaving protease requires a costimulus that is present in vivo but not in vitro. On the other hand, we have previously shown that the “classical” GPVI signaling pathway via LAT and PLCγ2 is essentially required for JAQ-induced GPVI shedding to occur in vivo, and this is associated with a transient drop in platelet counts.27 It is currently not clear whether the activation of metalloproteinases is mechanistically linked to the thrombocytopenia, but the data reported here clearly exclude a role of ADAM10 or ADAM17 in this process. Our data indicate that at least 3 different proteases could serve as target structures to “therapeutically” induce GPVI down-regulation, most likely without inducing thrombocytopenia.
In summary, we could demonstrate, for the first time, that GPVI can be differentially regulated in vitro by ADAM10 and ADAM17, depending on the shedding-inducing conditions. Furthermore, we provide evidence for the existence of a third GPVI cleaving enzyme in platelets that has the capacity to efficiently mediate the antibody-induced “therapeutic” GPVI down-regulation in vivo. These findings may serve as a basis for the development of safe anti-GPVI agents for the prophylaxis and treatment of ischemic and inflammatory disease states.
An Inside Blood analysis of this article appears at the front of this issue.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is herebymarked “advertisement” in accordance with 18 USC section 1734.
Acknowledgments
We thank Dr Radek Skoda for kindly providing the PF4-Cre mice and Birgit Midloch and Steffi Hartmann for excellent technical assistance.
D.S. was supported by a grant of the German Excellence Initiative to the Graduate School of Life Sciences, University of Würzburg, Würzburg, Germany. This work was supported by the Deutsche Forschungsgemeinschaft (Sonderforschungsbereich 688 to B.N.) and the Rudolf Virchow Center. The work of A.C., J.S., and S.R.J. was supported by the Deutsche Forschungsgemeinschaft, Bonn, Germany, and the Cluster of Excellence “Inflammation at Interfaces.”
Authorship
Contributions: M. Bender performed experiments, analyzed data, and contributed to the writing of the manuscript; S.H., D.S., A.C., M. Bösl, and A.B. performed experiments and analyzed data; J.S. and S.R.-J. analyzed data and contributed to the writing of the manuscript; and B.N. planned the project, analyzed data, and contributed to the writing of the manuscript.
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Correspondence: Bernhard Nieswandt, Chair of Vascular Medicine, Rudolf Virchow Center, DFG Research Center for Experimental Biomedicine, University Clinic Würzburg, Josef-Schneider-Str 2, 97080 Würzburg, Germany; e-mail: bernhard.nieswandt@virchow.uni-wuerzburg.de.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal