Abstract
Abstract 3453
Individuals undergoing allogeneic transplantation receive multiple red blood cell transfusions both as part of the transplant procedure and as part of the pre-transplant care of the underlying disease. Therefore these patients may be at risk for complications of transfusional iron overload. Several studies have noted that individuals entering the transplant with baseline elevated serum ferritin values have decreased overall survival and higher rates of disease relapse. Whether the iron is a direct contributor to inferior outcomes or is a marker of more advanced disease (thereby requiring greater transfusions) is unclear. Little is known about the incidence and consequences of iron overload among long-term survivors of allogeneic transplantation.
Using Kaplan-Meier and Cox regression analyses, we performed a single center, retrospective cohort study of consecutive allogeneic transplants performed at Hackensack University Medical Center from January 2002 through June 30, 2009 to determine the association between serum ferritin (measured approximately 1 yr post allogeneic transplant) and overall survival.
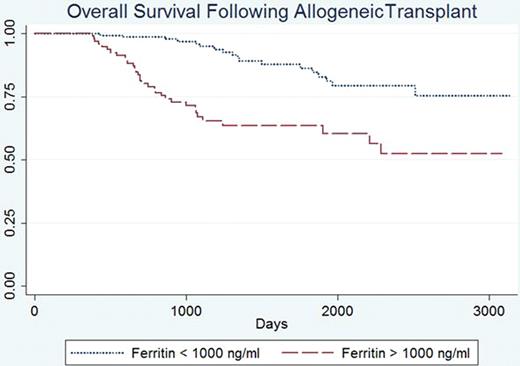
During the study time frame, 637 allogeneic transplants (Donor Lymphocyte Infusion procedures excluded) were performed at our center and 342 (54%) survived ≥ one year. Among 1-year survivors 240 (70%) had post-transplant serum ferritin values available for review, including 132 (55%) allogeneic sibling, 68 (28%) matched unrelated, and 40 (17%) mismatched unrelated donor transplants. The median post-transplant ferritin value among 1-year survivors of allogeneic transplant was 628 ng/ml (95% CI 17, 5010), with 93 (39%) above 1000 ng/ml and 40 (17%) above 2500 ng/ml. The median post-transplant ferritin levels varied by underlying hematologic disease (aplastic anemia = 1147, acute leukemia = 1067, MDS = 944, CLL = 297, CML = 219, lymphoma = 123, multiple myeloma = 90). The Kaplan-Meier projected 5-year survival rate was 76% for the cohort that had survived one year and had available ferritin values. Fifty late deaths have occurred; causes of late death were disease relapse (n=37, 74%), GVHD (n=7, 14%), infection (n=4, 8%), cardiac (n=1, 2%) and second malignancy (n=1, 2%). The 1-year post-transplant serum ferritin value was a significant predictor of long term survival. Using a cut-off ferritin value of 1000 ng/ml, the 5-year projected survivals were 85% (95 CI 75%-91%) and 64% (95% CI 52–73%) for the low and high ferritin cohorts respectively (Figure, log-rank p<0.001), with a hazard ratio of 3.5 (95% CI 2–6.4, p<0.001). Similarly a serum ferritin value >2500 ng/ml was associated with inferior survival (HR 2.97, p<0.001). Underlying hematologic disease also correlated with 5-year projected survival including 70%, 83%, and 89% for acute leukemia/MDS, lymphoma/myeloma/CLL, and aplastic anemia/CML groupings, respectively (log-rank p<0.01 for leukemia/MDS vs other groupings). Patients receiving bone marrow grafts did better than those receiving peripheral blood stem cells (HR = 2.2; p = 0.03). Age, gender, donor type (sibling, matched unrelated, mismatch unrelated) and intensity of regimen (ablative vs. non-myeloablative) were not predictive of inferior survival in univariate analysis. In the multivariate Cox-regression analysis, elevated post-transplant ferritin >1000 ng/ml (HR 3.3, 95%CI 1.6–6.1; p<0.001) and diagnosis of acute leukemia/MDS (HR 4.5, 95%CI 1.1–18.7; p=0.04) remained independent predictors of inferior survival, even when adjusted for age, gender, type of graft, donor type, and intensity of conditioning regimen. Relapse deaths (25% vs. 9%; p<0.001) and GVHD deaths (6% vs 0.6%; p=0.03) were more common in the high ferritin cohort.
Among patients who have survived one-year following allogeneic transplantation, a post-transplant serum ferritin value greater than 1000 ng/ml is a predictor of inferior long-term outcomes. To our knowledge this is the first report on the importance of late monitoring of serum ferritin, but it is in agreement with prior studies suggesting a pre-transplant ferritin value is a predictor of outcomes. Prospective studies attempting to modify outcomes by reducing post-transplant iron overload states are needed.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal