Abstract
Abstract 3464
Monitoring hematopoietic chimerism following allogeneic hematopoietic stem cell transplantation (alloSCT) after non-myeloablative (NMA) conditioning is commonly used to document engraftment. While mixed chimerism (MC) is frequently observed after NMA alloSCT, it occurs only rarely after myeloablative (MA) alloSCT. Persistent mixed chimerism is generally considered a risk factor for both relapse and rejection of the donor graft, irrespective of the type of conditioning regimen. However, it is still unknown to what extent mixed chimerism quantitatively predicts for relapse and whether patients at high risk for relapse can accurately be identified by assaying chimerism in either blood, marrow, and/or T cells. Therefore, we prospectively evaluated the establishment of complete and mixed chimerism in blood, marrow, and CD3+ selected T cells at 3, 6 and 12 months following alloSCT to investigate the predictive value of mixed chimerism in either subset for relapse.
The study cohort included 152 recipients of an alloSCT, performed between October 2005 and December 2009 because of hematological malignancies (AML: n=61, ALL: n=25, NHL: n=18, Myeloma: n=15, CML: n=5, CLL: n=18, MDS: n=6, MPN: n=4). Median age was 50 years (range 17–67). Seventy-eight patients received a sibling donor transplant, 74 a transplant from a matched related donor. MA and NMA conditioning consisted of Cyclophosphamide/TBI 1200 cGy (n=45) and Fludarabine/TBI 200cGy (n=107), respectively. Chimerism tests were routinely performed in bone marrow (BM), peripheral blood (PB) and CD3 selected samples at 3, 6 and 12 months post transplant, using PCR and electrophoresis of variable number of tandem repeats or fluorescent in-situ hybridization by sex-chromosome specific probes. Complete (donor) chimerism (CC) was defined as >95% donor hematopoiesis, MC as ≤95% donor hematopoiesis. The cumulative incidence of disease recurrence/progression and progression free survival by chimerism status was evaluated as from 3, 6 and 12 months post transplant and adjusted for type of conditioning, donor type, patient/donor sexe and age.
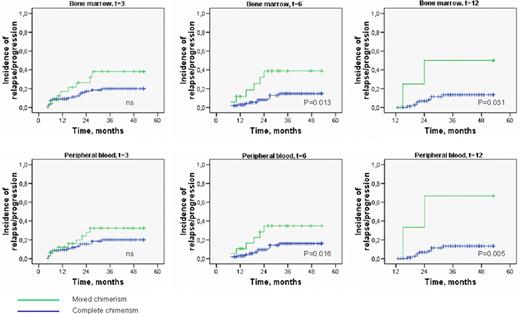
MC appeared very rare after MA conditioning, but was more frequently observed after NMA alloSCT with incidences of BM-MC of 28, 22 and 9% at the 3, 6 and 12 month timepoints, respectively. MC in BM as well as PB samples at 6 and 12 months post transplant was highly predictive for disease recurrence/progression, both after univariate and multivariate analyses (BM: hazard ratio (HR) at 6 months: 3.52 (1.30-9.53 95% confidence interval (CI)), p-value 0.013; at 12 months: 5.42 (1.17-25.13 95%CI), p-value 0.031). The probability to develop a relapse increased to 40% in time if MC was detected at 6 months following transplantation, as compared to 15% in the CC group. MC detected at 12 months resulted in a relapse incidence of ≥50% (Figure 1). Moreover, MC at these timepoints also predicted for decreased progression free survival (BM: HR at 6 months: 2.35 (1.04-5.27 95%CI), p-value 0.039; at 12 months: 9.36 (2.94-29.92 95%CI), p-value 0.000). Chimerism results in CD3+ selected T cell fractions did not show a significant association with relapse/progression or progression free survival.
These results show that patients with MC at 6 and 12 months post transplant in either BM or PB are at a 3 to 9 fold higher risk of disease recurrence/progression. T cell chimerism appeared not associated with relapse, which may be explained by a significant different and protracted pattern of kinetics after transplantation as compared to kinetics of PB and BM chimerism, thereby identifying different subgroups of patients. Collectively, this study highlights the need to rapidly establish complete donor chimerism both after MA and NMA alloSCT. The preferred medical intervention in patients with MC after NMA conditioning, however, remains to be established in a prospective study.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal