Abstract
Abstract 4574
CTCLs are generally incurable with conventional therapies. In particular, advanced mycosis fungoides (MF), Sézary syndrome (SS) and gamma delta varieties of CTCL have poor survival rates and are often refractory to traditional chemotherapy. Allogeneic SCT may provide a GVL effect and improve outcomes for these patients.
A retrospective analysis was performed at the University of Pennsylvania to identify all patients with CTCL who underwent allogeneic transplantation. 12 patients were identified who were transplanted between 2004 to 2010. A chart review was performed to obtain data about demographics, diagnosis, staging, treatment, transplantation and outcomes.
Median age at diagnosis was 49 yrs and M:F ratio was 5:7. Prior to transplantation, 4 had MF (stages IIB, IIIB, IVA1, IVB; 2 with nodal transformation), 4 had SS (one stage IVA1, three IVA2; 1 with nodal transformation), and 3 had gamma delta T-cell lymphoma (all T3b). Median time from diagnosis to transplantation was 3.3 yrs (range 0.5@02b97 yrs). Patients had received a median of 8 non-chemotherapy, and 2 chemotherapy-based treatment modalities before being transplanted. Only 3 patients were in complete remission (CR) at the time of conditioning and 9 had evidence of active disease. Reduced intensity conditioning (RIC) was used in 10 cases (Flu/Bu, Flu/Cy or Flu/Mel), and conventional myeloablative conditioning (Cy/TBI) was used in 2. GVHD prophylaxis consisted of calcineurin inhibitor and methotrexate in all patients.
The median follow up for all pts is 6.6 months (range 1.4 to 37.1 months) and 11.2 months for surviving patients. All patients engrafted with an ANC >500 a median 13 days after SCT. Median donor chimerism at day 100 after SCT in 10 evaluable pts was 97%. 7 of 12 patients developed acute GVHD, 4 of whom had grade 3 GVHD.
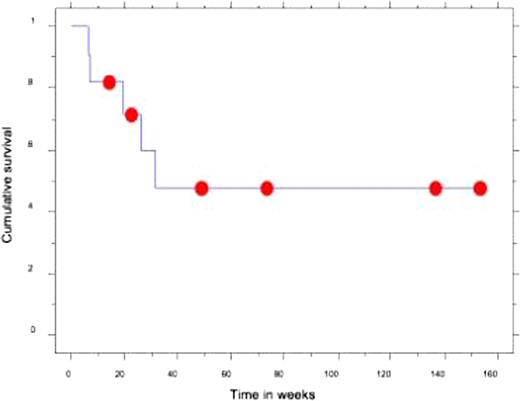
Two patients died within the first 100 days, from sepsis with active disease. At day 100, 7 of 10 evaluable patients were in CR, with an additional patient achieving CR shortly after; therefore transplant induced and maintained CR in 6 pts with active disease. 3 patients relapsed after achieving CR a median of 11.4 months (range 5.3–13.0 months) after SCT. 2 patients never achieved CR, and progressed within a month of transplantation. The median PFS for all pts was 31 wks, and 1 yr and 2 yr PFS were 48% and 32% without an obvious plateau. 2 year OS was 53% (Figure 1). Median OS is not reached.
6 patients have died from progression (5) and GVHD (1), 5 remain in CR and 1 is alive with active disease.
RIC SCT can provide long-term disease control in patients with advanced CTCL otherwise refractory to immunotherapy and chemotherapy. Given the limited TRM, consideration for earlier transplant should be given. Larger retrospective and ideally prospective studies will further define the role of allogeneic SCT in this disease.
Kaplan Maier plot showing overall survival in patients with CTCL undergoing allogeneic SCT.
Kaplan Maier plot showing overall survival in patients with CTCL undergoing allogeneic SCT.
Rook:Therakos: Speakers Bureau; HY Biopharma: Consultancy. Kim:TenX: Research Funding; Biocryst: Research Funding; Genmab: Research Funding; Glouchester: Research Funding; Celgene: Research Funding; Eisai: Consultancy.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal