Abstract
Abstract 976
Lenalidomide (LEN) is particularly effective on anemia of lower risk MDS with del 5q (List et al, NEJM, 2006). A compassionate program (ATU) of LEN in RBC transfusion dependent (TD) low and int 1 (lower) risk MDS with del 5q was opened by the French health agency between Jan and Sept 2007. The concern raised by EMEA that LEN may trigger progression to AML in some MDS with del 5q lead us to compare the outcome of our cohort to that of RBC transfusion dependent lower risk MDS with del 5q that never received LEN.
95 RBC -TD lower risk MDS pts with del 5q, diagnosed between 1988 and 2007 in GFM centers, received 10 mg of LEN/day, 3 weeks on, 1 week off. Median age was 70.4 years, median interval from diagnosis to LEN was 29 months. IPSS was low in 31% and intermediate-1 in 69% patients. Del 5q was isolated, with 1 additional and > 1 additional abn in 79%, 14%, and 6% patients, respectively. 60 (63%) pts achieved transfusion independence (TI). We compared the risk of progression to AML and survival from diagnosis of this cohort and of a historical cohort of 99 similar RBC TD lower risk MDS with del 5q deletion diagnosed between 1985 en 2005 in GFM centers and treated before LEN was available in France (part of those pts have been reported in Kelaidi,Leuk Res 2008). For this non randomized comparison, we used the propensity score method. This method can estimate unbiased treatment effects from observational studies based on a propensity score, ie re-create the exchangeability between two treatments groups. We determined a propensity score defined as a subject's probability of receiving LEN conditionally on his observed covariates. For this purpose, we modeled through multivariate logistic regression, in pts with RBC transfusion dependent lower risk MDS with del 5q the probability of receiving LEN conditionally on a set of baseline characteristics (including age, gender, WHO diagnosis, IPSS score, cytogenetics). The estimated propensity was then used to match 1:1 patients with similar propensity to receive LEN.
In the LEN cohort, with a median follow up of 18.5 months from onset of LEN, 6 (6.3%) pts had progressed to AML, after 30 to 67 weeks (median 45 weeks), including 2 pts who had achieved TI. At onset of LEN, 4 of them had an IPSS of 1, and 2 of 0.5. Two had isolated del 5q and 4 had one additional cytogenetic abn.
Baseline characteristics of the LEN cohort and the historical cohort treated without LEN were similar, except for age (median 73 years in the latter, vs 70.4, p= 0.03), and % of RARS (14% vs. 4%, p= 0.05). The propensity score was derived from a multivariate logistic model incorporating pt age at diagnosis, gender, WHO, IPSS and cytogenetics. Then, a matched-dataset was constituted between pts who received or not LEN. Seventy-one pts in each group could be matched, erasing differences in covariates between the two treatment groups.
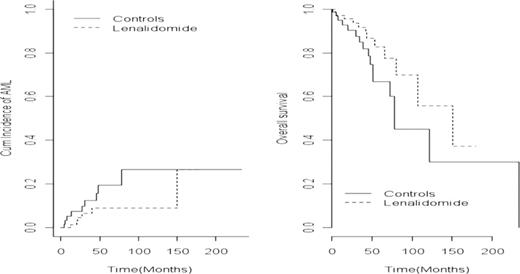
In those 71 matched pairs, the 4 year-cumulative incidence of AML from diagnosis was 8.9% in the 71 matched pts treated with LEN and 15.8% in the 71 matched pts who received no LEN (HR= 0.46, 95%CI: 0.16–1.35; p=0.14) (figure 1). Median overall survival was 150 months in the 71 pts treated with LEN vs 72.8 months in the 71 pts treated without LEN (HR= 0.54, 95%CI: 0.26–1.11; p= 0.10).
Using a propensity score methodology, we found the incidence of progression to AML from diagnosis, in the present cohort treated with LEN, not to be greater than that of a comparable historical cohort of RBC transfusion dependent lower risk MDS with del 5q treated without LEN. Likewise, no significant survival difference was found between the 2 groups.
Fenaux:CELGENE, JANSSEN CILAG, AMGEN, ROCHE, GSK, NOVARTIS, MERCK, CEPHALON: Honoraria, Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal