Abstract
Transcranial Doppler-detected high-intensity transient signals (HITS) during cardiopulmonary bypass (CPB) surgery have been associated with postoperative neurocognitive dysfunction, suggesting microemboli in the brain could be a contributing factor. HITS occur despite administration of unfractionated heparin (UFH). This study was done to determine whether antithrombin-heparin covalent complex (ATH), a more potent anticoagulant than heparin, can reduce HITS during CPB. In a pig CPB model, ATH, UFH, or UFH + antithrombin (AT) was intravenously administered to female Yorkshire pigs after sternotomy. Twenty minutes later, hypothermic CPB was initiated and continued for 1.25 hours, then normothermia was re-established for 45 minutes. Protamine sulfate was given to neutralize the anticoagulants, and pigs were allowed to recover. HITS were monitored using an arterial flow probe placed over the carotid artery. Compared with UFH (300 or 1000 U/kg), ATH reduced the number of HITS during CPB in a dose-dependent manner. AT (3 mg/kg) + UFH (300 U/kg) resulted in an intermediate HITS rate between UFH and ATH (2 mg/kg in terms of AT). Examination of brain sections for emboli formation confirmed that, similar to HITS, number of thrombi decreased in direct proportion to ATH dosage. These results support the hypotheses that the majority of HITS represent thromboemboli and that ATH reduces emboli formation during CPB.
Introduction
Many important advances in cardiac surgery were made in past decades including procedures such as cardiopulmonary bypass (CPB), coronary artery bypass grafting, and cardiac repair or replacement surgery.1,2 There is some evidence of adverse neurological effects associated with cardiac surgery, particularly with CPB. Neurocognitive dysfunction is a common complication of cardiac surgery.3-6 The etiology of neurocognitive dysfunction is controversial, but there is evidence suggesting that microemboli may be a contributing factor. Some studies have been performed using transcranial Doppler ultrasound to detect microemboli as high-intensity transient signals (HITS) during cardiac surgery.7,8 In these studies, HITS were associated with neurocognitive deficits, especially with respect to memory loss. Of the possible sources of microemboli, including air, thrombi, and fat from cellular or particulate matter promoted by the bypass pump, thromboemboli are thought to be an important contributor to the neurocognitive dysfunction that occurs after CPB.9,10
Currently, unfractionated heparin (UFH) is the standard agent used for anticoagulation during CPB. Although UFH provides sufficient anticoagulation to prevent clotting within the bypass circuit, clinical application of UFH is limited by its pharmacokinetic and biophysical properties. UFH has a short, dose-dependent intravenous half-life and an unpredictable anticoagulant effect, mainly due to variable nonspecific plasma and cell surface protein binding.11,12 UFH is also unable to inactivate surface-bound coagulation factors, such as fibrin-bound thrombin (protected from inactivation by the heparin/antithrombin [AT] complex),13,14 and may activate platelets.15 This inability to neutralize fibrin-bound thrombin makes UFH incapable of reducing fibrin-based thrombin generation leading to thromboemboli growth during CPB, since studies have shown that clot propagation is primarily due to the activity of clot-bound thrombin.13,16,17 In addition, high concentrations or repeated exposure of UFH can lead to bleeding and other complications.18,19
We have produced a covalently linked antithrombin-heparin (ATH) complex with superior anticoagulant activity compared with UFH, which has potential for therapeutic application without many of UFH's limitations. ATH has a high, rapid rate of direct (noncatalytic) thrombin inhibition and possesses a potent anti-factor (F) Xa indirect (catalytic) activity.20-22 This initial rapid rate of reactivity of ATH prevents the exponential increase in thrombin generation at early stages of clot formation. Not only does ATH inhibit thrombin and FXa more effectively than UFH, it also has a longer intravenous half-life, remaining in the circulation 6- to 8-fold longer than uncomplexed UFH.20 Thus, ATH would give a more controlled circulating concentration during CPB anticoagulation. The superior vascular bioavailability of ATH is a result of ATH's larger size20 and reduced binding to plasma and endothelial cell surface proteins,23 which are significant factors in the elimination of UFH from the circulation.24,25 Since, unlike noncovalent AT●heparin, ATH is able to neutralize fibrin-bound thrombin,26,27 this may be an important factor in reducing HITS during CPB. In vivo studies in rabbit venous28 and arterial27 thrombosis models have shown that ATH was able to reduce clot mass with diminished bleeding side effects compared with UFH. Thus, ATH has the unique ability to inhibit clot growth as well as prevent clot formation.
The purpose of this study was to examine the efficacy of ATH to prevent or reduce HITS and emboli prior to, during, or following CPB in a pig model. In addition, the efficacy of ATH was compared with the efficacy of equivalent doses of either UFH or UFH supplemented with transgenic AT.
Methods
Test anticoagulants
Heparin of various lots (injection sodium heparin from Organon Teknika), ATH of various lots (Henderson Research Center, and human recombinant AT of transgenic source (GTC Biotherapeutics) were used. The method for preparation of ATH was as described previously.20
The pig CPB model
A porcine CPB system was developed at our institution since the effects of anticoagulants in pig models have proven to be predictive of their efficacy in human thrombotic conditions.29 Thirty-seven female Yorkshire pigs (22-66 kg) were obtained from the University of Guelph Arkell Research Center and acclimatized for at least 1 week prior to experimentation. Pigs were housed at the Henderson Research Center Animal Facility, and animals had ad libitum access to autoclaved Purina Porcine Lab Diet (#5084). The animal room environment and photoperiod were controlled to target conditions of 20°C, 50% humidity, and 12 hour light/12 hour dark cycles. The protocol for this study was approved by the Animal Research Ethics Board of McMaster University (Hamilton, ON; Animal Utilization Protocol #00-05-15). All animal procedures followed the guidelines of the Canadian Council on Animal Care.
The timeline and procedures of the pig CPB model are shown in Figure 1. The CPB procedure was performed using a model 5000 heart-lung bypass pump machine from Sarns, which was fitted with an Affinity arterial filter (38-μm screen, 31% open area) from Medtronic. Standard polyethylene tubing was used throughout the circuit. Anesthesia was initiated by intramuscular injection of ketamine (20 mg/kg), acepromazine (0.2 mg/kg), and atropine (0.05 mg/kg) and maintained with a mixture of isofluorane (1-3%), oxygen (1.8 L/min), and nitrous oxide (1.2 L/min) delivered through a 9.5 F endotracheal tube using a positive pressure ventilator (Vapomatic, AM Bickford). The respiratory rate was adjusted to maintain arterial blood pH and pCO2 and pO2 in the physiologic range. During CPB, inhalation anesthesia was delivered through a membrane oxygenator (Affinity Brand, 38 μm pore membrane; Medtronic) and supplemented with 1-2 mL of intravenous sodium phenobarbital. The total anesthesia time was approximately 6 hours (1 hour of pre-CPB surgical manipulation, 2 hours of CPB, 3 hours of post-CPB recovery).
Pig cardiopulmonary bypass (CPB) model timeline. The arrows indicate the blood sampling times.
Pig cardiopulmonary bypass (CPB) model timeline. The arrows indicate the blood sampling times.
A 14-gauge intravenous cannula was inserted in the marginal auricular vein of the right ear for administration of drugs and fluids, and the femoral artery and both carotid arteries were exposed. A blood pressure transducer was connected to the right femoral artery, while Doppler ultrasound transducer probes were placed on both carotid arteries. “Pre-CPB” HITS data were collected, and a “baseline” activated clotting time (ACT) was measured using a Hemochron 801 machine (International Technidyne Corporation). A 5 mg/kg bolus of bretylium tosylate was administered intravenously to prevent cardiac arrhythmia, and the heart and great vessels were exposed through a median sternotomy. A pericardial cradle was then created, and hemostasis was secured.
The test anticoagulant drug was administered intravenously (approximately 50 minutes after taking the “baseline” ACT and more than 20 minutes after sternotomy). Five minutes later, a blood sample was taken for ACT. An ACT of at least 500 seconds was required before proceeding. If this ACT value was not achieved at the beginning of or at any time during CPB, supplemental anticoagulant was given at 25% of the initial dose until the ACT exceeded 500 seconds (supplementation of AT + heparin was with heparin only). In no case was anticoagulant supplemented over the course of CPB with more than half of the starting dose. The ascending aorta was cannulated and connected to the CPB circuit (for “partial bypass”), taking care to avoid air bubbles, and then the right auricle was cannulated to secure a venous line to the CPB circuit. CPB began approximately 20 minutes after injection of anticoagulant. Reduction of core body temperature to 28°C was initiated and maintained using the CPB circuit heater/cooler unit (the hypothermic state was reached about 20 minutes into CPB).
The CPB circuit was composed of the following components: an affinity integrated coronary vascular resistance membrane oxygenator with a heater/cooler unit, a venous reservoir (maintained at 800 mL with either Ringer's lactate solution containing 7.5% [44 mEq] sodium bicarbonate or reused cavity blood), an online arterial blood filter, a roller pump set for 3.5-4.6 L/min (60% of cardiac output), a 2-stage armored venous drainage catheter, and a return arterial cannula. Mean arterial pressure was maintained above 50 mmHg. A suction pump was also available, but it was turned off during the bypass to allow manual measurement of chest cavity bleeding. After periodic measurement of cavity blood, the blood was returned to the CPB system via the oxygenator reservoir. Supportive therapy was instituted if needed (epinephrine, dopamine, CaCl2, sodium bicarbonate, etc.).
After approximately 1.25 hours of hypothermic CPB, warm up of the pig was begun, and after a total CPB time of 2 hours, the venous CPB line was removed, and the remaining blood from the CPB circuit was infused. Decannulation took approximately 5 minutes, after which a “preprotamine” ACT was taken.
After 5 minutes, anticoagulation was reversed with protamine sulfate (Sabex) to reach the pre-CPB ACT value (dose calculated as 1 mg/100 units of heparin). When stabilization was achieved, the CPB arterial line was removed. Two chest tubes were placed into the pericardial cavity, connected to the chest drainage unit, and kept under negative pressure of 10 mL water. An ACT was then taken (protamine t0). After 3 hours post-CPB (post-protamine), animals were anticoagulated with heparin and then euthanized with sodium phenobarbital.
Selection of doses
The doses of anticoagulants were chosen to cover the maximum range that might be encountered in CPB. A heparin dose of 300 U/kg is the equivalent of the usual dose of heparin given to patients undergoing CPB. This dose of heparin yields an ACT over 450 seconds, which is the target ACT for most CPB cases. The higher heparin dose (1000 U/kg) was selected to determine whether supratherapeutic heparin administration would provide better reduction in HITS and/or microthrombi than the usual heparin doses.
Animal identification and treatment groups
A total of 37 female pigs, individually identified by numbered ear tags following arrival, were assigned to 8 groups. Pigs were bolus dosed with the concentrations of anticoagulants as specified in Table 1, and ranges of additional anticoagulant administered were also noted. Doses shown on the graphs in the figures are the initial doses (not final doses when supplementation was required).
Dosing chart for pig groups in cardiopulmonary bypass (CPB) model
| Group # . | Anticoagulant . | n . | Initial heparin mass equivalent (mg/kg) . | Initial heparin activity equivalent (U/kg) (range) . | Total heparin mass equivalent (mg/kg) . | Total heparin mass equivalent (U/kg) . | Total AT mass equivalent (mg/kg) . | Neutralizing protamine sulfate given (mg/kg) . |
|---|---|---|---|---|---|---|---|---|
| 1 | 300 U/kg UFH | 5 | 1.9 | 300 (300 - 456) | 2.6 | 421 | — | 0.52 |
| 2 | 1000 U/kg UFH | 5 | 6.3 | 1000 | 6.3 | 1000 | — | 1.94 |
| 3 | 1 mg/kg ATH | 3 | 0.4 | 225 | 0.6 | 393 | 2.0 | 1.18 |
| 4 | 2 mg/kg ATH | 6 | 0.6 | 385 | 0.8 | 512 | 2.7 | 1.06 |
| 5 | 3 mg/kg ATH | 5 | 1.1 | 677 | 1.1 | 707 | 3.6 | 1.59 |
| 6 | 6 mg/kg ATH | 4 | 1.9 | 1217 | 1.9 | 1217 | 6.0 | 1.29 |
| 7 | 3 mg/kg AT +300 U/kg UFH | 5 | 1.9 | 300 (300 - 375) | 2.2 | 345 | 3.0 | 1.06 |
| 8 | 6 mg/kg AT + 300 U/kg UFH | 4 | 1.9 | 300 | 2.7 | 420 | 6.0 | 1.05 |
| Group # . | Anticoagulant . | n . | Initial heparin mass equivalent (mg/kg) . | Initial heparin activity equivalent (U/kg) (range) . | Total heparin mass equivalent (mg/kg) . | Total heparin mass equivalent (U/kg) . | Total AT mass equivalent (mg/kg) . | Neutralizing protamine sulfate given (mg/kg) . |
|---|---|---|---|---|---|---|---|---|
| 1 | 300 U/kg UFH | 5 | 1.9 | 300 (300 - 456) | 2.6 | 421 | — | 0.52 |
| 2 | 1000 U/kg UFH | 5 | 6.3 | 1000 | 6.3 | 1000 | — | 1.94 |
| 3 | 1 mg/kg ATH | 3 | 0.4 | 225 | 0.6 | 393 | 2.0 | 1.18 |
| 4 | 2 mg/kg ATH | 6 | 0.6 | 385 | 0.8 | 512 | 2.7 | 1.06 |
| 5 | 3 mg/kg ATH | 5 | 1.1 | 677 | 1.1 | 707 | 3.6 | 1.59 |
| 6 | 6 mg/kg ATH | 4 | 1.9 | 1217 | 1.9 | 1217 | 6.0 | 1.29 |
| 7 | 3 mg/kg AT +300 U/kg UFH | 5 | 1.9 | 300 (300 - 375) | 2.2 | 345 | 3.0 | 1.06 |
| 8 | 6 mg/kg AT + 300 U/kg UFH | 4 | 1.9 | 300 | 2.7 | 420 | 6.0 | 1.05 |
UFH indicates unfractionated heparin; AT, antithrombin; and ATH, antithrombin-heparin covalent complex.
Doppler HITS
Transarterial ultrasound Doppler HITS were measured by placing 2 round 2 MHz probes (Spencer Technologies) liberally covered with Aquasonic 100 ultrasound transmission gel (Parker Labs) on each of the 2 carotid arteries. Care was taken to avoid air bubbles in the gel, and the probes were oriented at a 20° angle with respect to the artery. Adjustments were made to optimize the signal, which was sent to a computer in the TCD 2020 transcranial Doppler machine (Nicolet Vascular) for digitized storage and computer recognition of HITS.
Discrimination of microemboli from air bubbles and dislodged fat was investigated in a preliminary study, and distinctive characteristic patterns for each agent were seen. In this study, such a level of discrimination was not needed so that all HITS were counted.
HITS were integrated for segments of time represented by the blood sampling times shown on the timeline (Figure 1). These integrated values were then analyzed by 3 methods. Total HITS were summed for the study segments “Pre-CPB,“ “CPB,” and “Post-CPB.” Average HITS rates (normalized per hour) were determined for each study segment, and normalized HITS rates were determined for smaller sampling segments (to give a more dynamic picture of HITS response).
Blood loss measurement
Chest cavity blood was collected at specific time points, measured for volume, and returned to the CPB circulation.
Blood samples for coagulation analysis and reference
Blood samples were taken from the pig as indicated on the timeline (Figure 1) and as needed (2 mL EDTA [ethylenediaminetetraacetic acid] samples were taken for CBC, 5 mL 0.32% Na citrate plasma samples were taken for anticoagulant assay for thrombin-antithrombin [TAT] complex levels, 3 mL samples were taken for ACT [t0 set at the beginning of bypass], 1 mL samples in preheparinized syringes were taken for blood gas, pH, sodium, and potassium level analyses). Standard hematological testing (white blood cell, red blood cell, platelets, hematocrit, and hemoglobin levels) and TAT level analysis were done in the Clinical Chemistry Lab at the Henderson Hospital (Hamilton, ON). Chest blood volume was periodically measured as well as rectal temperature.
Tissue analysis for fibrin emboli
In order to determine if there was a relationship between anticoagulant dose and emboli number, segments from brains of ATH-treated pigs were embedded in paraffin, sectioned, and stained with MSB (martius/scarlet/blue) for fibrin.30 Fibrin thrombi in the microvasculature were quantified by microscopic observation. The total number of microthrombi in the sections was square-root transformed (in order to minimize impact from potential nonuniform variances between sections of different animals) and divided by the sectional area. In one set of intensive analyses, the total number of emboli from sections of the entire brain for all animals in the 300 U/kg UFH group were compared with those in the 3 mg/kg ATH group.
Statistical analysis
Data means and standard deviations (SDs) were calculated for graphical representation. Data were compared for significant differences by either analysis of variance followed by Bonferroni post-test or using 2-tailed Student t test between paired groups where appropriate. A P value of < .05 was considered significant.
Results
Treatment time course
Only healthy animals were included in the study. At all times, sufficient anticoagulation was achieved during bypass for all treatment groups, and all anticoagulant effects were neutralized with protamine sulfate postbypass. Hypothermia was maintained in all animals during CPB and was gradually returned to normothermia postbypass. For all treatment groups, during CPB there was approximately a 60% decrease (from t = 0) in the white blood cell count (a result of hemodilution), followed by a slow recovery to normal levels after CPB. Also, there was a slight decrease in hematocrit and K+ levels during CPB, again most likely due to hemodilution, followed by a gradual increase to normal levels post-CPB. There were no major fluctuations observed in the number of platelets and red blood cells, as well as levels of blood gases (PO2 and PCO2), Na+ levels, blood pH, and hemoglobin levels during the surgery. All parameters were within acceptable physiological ranges during and post-CPB for all treatment groups.
HITS during CPB
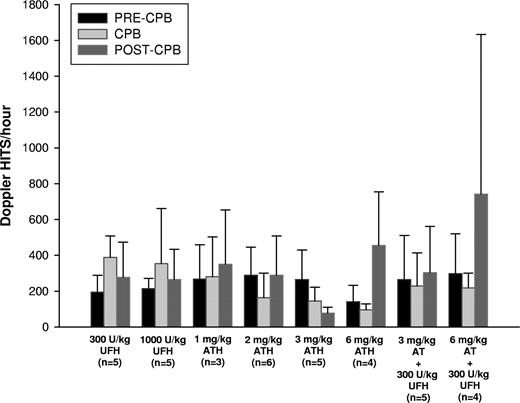
Poststernotomy, but pre-CPB, Doppler HITS occurred at a rate ranging from 53.3-700.0/h for the various experimental groups (Figure 2). Compared with pre-CPB, HITS increased for UFH during bypass by almost 50% regardless of dose. In marked contrast, a dose-dependent decrease in CPB HITS was seen with ATH at doses ranging from 1-6 mg/kg. Experiments with AT (3 mg/kg) + UFH (300 U/kg) resulted in an intermediate HITS rate between UFH and 2 mg/kg ATH. Doubling the AT dose did not significantly change the HITS rate. ATH at 3 mg/kg was the only treatment with a post-CPB HITS rate less than the rate pre-CPB value.
Average Doppler HITS/hour: before (pre-CPB), during (CPB), and after (post-CPB) hypothermic cardiopulmonary bypass (CPB). HITS indicate high-intensity transient signals; UFH, unfractionated heparin; ATH, antithrombin-heparin covalent complex; and AT, antithrombin. Results are mean ± SD.
Average Doppler HITS/hour: before (pre-CPB), during (CPB), and after (post-CPB) hypothermic cardiopulmonary bypass (CPB). HITS indicate high-intensity transient signals; UFH, unfractionated heparin; ATH, antithrombin-heparin covalent complex; and AT, antithrombin. Results are mean ± SD.
During bypass, HITS rate for the group of pigs administered 2 mg/kg ATH, 3 mg/kg ATH, or 6 mg/kg ATH were significantly lower than the group given 300 U/kg UFH (P = .0187, P = .0052, and P = .0023, respectively). Also, pigs given 6 mg/kg ATH had a significantly lower HITS rate during CPB than the group given 6 mg/kg AT + 300 U/kg UFH (P = .0351). Post-CPB, the group given 3 mg/kg ATH had a significantly lower HITS rate than those administered 1000 U/kg UFH (P = .0403).
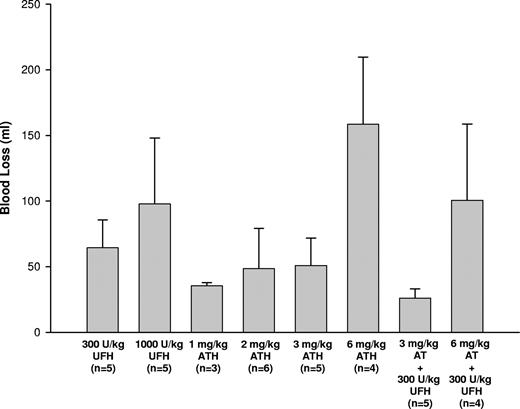
Blood loss during CPB
Overall, low bleeding levels were observed during bypass with the animals in this study (Figure 3). All treatment groups, except the 6 mg/kg ATH group, had comparable cumulative blood loss at the end of bypass surgery. The 6 mg/kg ATH group had significantly more blood loss compared with 300 U/kg UFH, 1 mg/kg ATH, 2 mg/kg ATH, 3 mg/kg ATH, and AT (3 mg/kg) + UFH (300 U/kg) (P < .05 for all comparisons). However, all tested anticoagulants showed clinically acceptable safety profiles during CPB.
Total blood loss from chest cavity during hypothermic cardiopulmonary bypass (CPB). UFH indicates unfractionated heparin; ATH, antithrombin-heparin covalent complex; and AT, antithrombin. Results are mean ± SD.
Total blood loss from chest cavity during hypothermic cardiopulmonary bypass (CPB). UFH indicates unfractionated heparin; ATH, antithrombin-heparin covalent complex; and AT, antithrombin. Results are mean ± SD.
Analysis of TAT levels during CPB
Since the 3 mg/kg ATH treatment group was able to decrease the HITS rate during CPB compared with the corresponding 300 U/kg UFH and 3 mg/kg AT + 300 U/kg UFH groups, we further examined the presence of thrombin generation markers during CPB (Figure 4). Examining the TAT production in each group during the bypass period showed a significant increase in TAT levels at 60 minutes compared with base (t = 0) (P < .05) but decreased to base levels at the end (120 minutes) for the 300 U/kg UFH group. Animals given 3 mg/kg AT + 300 U/kg UFH had a significant increase in TAT levels compared with base at 120 minutes (P < .05). However, at the end of bypass surgery, there were no differences in TAT production among all 3 groups.
Thrombin-antithrombin complex (TAT) levels during cardiopulmonary bypass (CPB). UFH indicates unfractionated heparin; ATH, antithrombin-heparin covalent complex; and AT, antithrombin. Results are mean ± SD.
Thrombin-antithrombin complex (TAT) levels during cardiopulmonary bypass (CPB). UFH indicates unfractionated heparin; ATH, antithrombin-heparin covalent complex; and AT, antithrombin. Results are mean ± SD.
Analysis of brain microemboli
In order to confirm if decrease in HITS due to ATH treatment indeed corresponded to a reduction in emboli, brain sections were stained for fibrin and microthrombi determined by microscopic examination (square root of emboli number per sectional area). An inverse correlation was clearly evident between ATH dose and brain emboli formation when combining all data sets (Figure 5A). Linear regression analysis of 1-3 mg/kg ATH dose versus the corresponding emboli data revealed a markedly negative slope (-2.7) and a significant linear correlation coefficient (r2 = 0.66). In comparison, dose versus HITS showed a similar decrease in signals with increasing ATH administered (Figure 2). Combined data gave a suggestion that the 3 mg/kg dose of ATH might have the highest efficacy (emboli) relative to risk (bleeding). Comprehensive analyses comparing total number of brain microemboli in the 300 U/kg UFH treatment with that of the potentially optimal ATH dosing of 3 mg/kg showed a significant decrease in brain emboli with ATH compared with UFH (P = .036) (Figure 5B).
Comparison of fibrin-emboli in porcine brain sections during hypothermic cardiopulmonary bypass (CPB). (A) Fibrin-emboli per area (given as the square root of fibrin thrombi for all brain sections divided by the total sectional area [in cm2]) and (B) total number of brain emboli. ATH, antithrombin-heparin covalent complex; and UFH, unfractionated heparin. Results are mean ± SD.
Comparison of fibrin-emboli in porcine brain sections during hypothermic cardiopulmonary bypass (CPB). (A) Fibrin-emboli per area (given as the square root of fibrin thrombi for all brain sections divided by the total sectional area [in cm2]) and (B) total number of brain emboli. ATH, antithrombin-heparin covalent complex; and UFH, unfractionated heparin. Results are mean ± SD.
Discussion
Heparin has been used as the primary anticoagulant in cardiac surgery, including CPB, for many decades. Advances in heparin administration and surgical innovations have decreased the morbidity and mortality rates of these cardiac patients.31,32 However, evidence suggests that microemboli formation still poses a problem during and after surgery despite heparin use.3-6 Transcranial Doppler monitoring has been used to detect microemboli as HITS,8 which coincide with alterations in neuropsychological function in some patients after surgery.33 In order to subdue thrombi formation during CPB, ongoing heparin administration is maintained as a standard protocol. However, apart from limitations of a short intravenous half-life and variable anticoagulant response,11,12 heparin's inability to inhibit clot-bound thrombin13,14 reduces its capacity for microthrombi prevention. Application of large heparin dosing (usually 300-400 U/kg) and additional boluses to maintain suitable ACT response during CPB can potentially lead to bleeding complications during and after surgery.18,34 We prepared a covalent ATH complex that exhibits increased plasma half-life,20,28 decreased nonselective plasma/endothelial surface protein binding,23 high catalytic inhibition of thrombin due to high activating pentasaccharide content,20,21,35 and rapid neutralization of fibrin-bound thrombin26,27 relative to heparin. These features suggested that ATH may be an improved medication for reduction of arterial HITS as a possible surrogate measure of emboli during CPB.
Since anticoagulants were injected well after sternotomy, it is likely that pre-CPB HITS reflect activation of the coagulation cascade as a result of tissue damage induced by sternotomy and the initial effects of drug on this background. Thus, sensitivity to any differences in effects from the different drugs is expected to be low during this period. ATH yielded a HITS rate during CPB that was reduced compared with prebypass values. Comparatively, UFH gave a HITS rate during CPB almost twice that seen pre-CPB, even for heparin doses as high as 1000 U/kg UFH (Figure 2). ATH at a dose of 3 mg/kg reduced the CPB HITS rate to about half the pre-CPB rate, while ATH at a dose of 6 mg/kg tended to reduce the CPB HITS rate even further. However, the decrease in pre-CPB HITS going from 3 to 6 mg/kg ATH was not statistically significant (P = .09). A close comparison of select UFH and ATH groups clearly emphasizes the contrast in efficacies. Table 1 shows the difference in heparin concentration (in units) when heparin alone is given for CPB compared with the heparin content in ATH. By comparison, with ATH at a dose of 1.1 mg heparin/kg, HITS/h (145.6 ± 34.5) was significantly lower (P = .0052) than that for 1.9 mg UFH/kg (387.9 ± 53.5). Thus, less heparin compound was given with the ATH treatment, but the anticoagulant effect was more pronounced.
Our results showed that groups given only UFH had HITS rates that were increased by almost 50% compared with pre-CPB levels, even for heparin doses as high as 1000 U/kg. Conversely, HITS rates were decreased during bypass in groups given ATH, and this reduction appeared to be dose-dependent. Interestingly, the 3 mg/kg ATH group had a HITS rate that was almost half the pre-CPB HITS rate (Figure 2). In fact, groups given ATH (at 2, 3, and 6 mg/kg) had significantly lower HITS rates during CPB than those given 300 U/kg UFH. Increased HITS rate during CPB in animals given UFH alone could be attributed to the inability of UFH to inhibit fibrin-bound thrombin.14 As a consequence, protection of thrombin bound to fibrin from fluid-phase inhibitor inactivation13 may allow for continuing platelet activation36 and enhanced coagulation.37 Consistent with this hypothesis, treatment with therapeutic levels of UFH has been associated with platelet activation.15 ATH was able to reduce the HITS rate during CPB compared with pre-CPB levels most likely due to its ability to inhibit fibrin-bound thrombin.26,27 Furthermore, ATH can decrease clot mass, as shown in studies involving rabbit venous28 and arterial27 thrombosis models, with minimal bleeding risk compared with UFH.27 The rapid inactivation rate with ATH is minimally affected by the presence of fibrin due to the covalent linking of heparin to AT, which would not allow for the formation of heparin●thrombin●fibrin ternary complexes.26
Bypass groups given UFH supplemented with AT had HITS rates that were at an intermediate level between groups given UFH and 2 mg/kg ATH. The HITS rate did not significantly change when supplementation with AT was doubled from 3 mg/kg to 6 mg/kg. Only the 6 mg/kg ATH group had a significantly lower HITS rate than groups given 300 U/kg UFH supplemented with 6 mg/kg AT. AT supplementation may have slightly augmented the inhibition rate of UFH but the HITS rate was unaffected, possibly due to the rate-limiting step of AT binding to heparin.38 Hence, doubling the AT concentration did not consequently decrease the HITS rate by a significant amount. Covalent linkage of heparin to AT in the ATH complex allows the AT moiety to be in a permanently activated state. This is evident since the AT cannot dissociate from heparin35 and the rate-limiting step of AT binding to heparin is eliminated. All ATH molecules have been shown to have at least one pentasaccharide sequence on the heparin chain to activate AT, and as many as 40% of the molecules possess 2 or more pentasaccharide sequences.21,39 In addition, ATH with one pentasaccharide sequence activating the covalently linked AT can bind to exogenous, free AT.21 In contrast, approximately 30% of commercially available heparin molecules have an AT-activating pentasaccharide sequences and only 1-3% have 2 or more pentasaccharides.40,41 Thus, all pentasaccharide sequences present on the heparin chain of ATH can potentially activate exogenous AT, resulting in high capacity for thrombin inhibition compared with UFH.
With any surgery involving the use of anticoagulants, there is an inherent risk of bleeding18 In this CPB study, little bleeding was observed during the experiments (Figure 3). Although there was a greater reduction in HITS rate for the 6 mg ATH/kg treatment group, this was accompanied by a slight increase in bleeding risk. Thus, ATH had greater efficacy than UFH but with marginal decrease in safety. Further analysis of the data showed that all tested anticoagulants had comparable safety profiles during CPB. In all cases, complete anticoagulation reversal was achieved by standard dosing of protamine sulfate.
We have demonstrated that ATH was able to reduce the HITS rate and reduce emboli formation during CPB. To determine the extent of corresponding thrombin generated in those receiving either 3 mg/kg ATH, 300 U/kg UFH, or 3 mg/kg AT supplemented with 300 U/kg UFH, TAT levels were measured as markers of thrombin inhibition. It is interesting to note that during the CPB period, the ATH group showed a flat TAT curve (Figure 4) indicating that ATH was able to inhibit thrombin (free and fibrin-bound thrombin)26,27 and possibly attenuate the propagation phase of thrombin formation. The UFH treatment group had a spike in TAT levels which peaked at 60 minutes followed by a decline, while the AT + UFH group showed a steady increase in TAT levels throughout the time course (Figure 4). Despite having significant systemic anticoagulation (prolonged ACT > 500 seconds throughout the entire surgical procedure), the heparin present in the UFH and AT + UFH groups was unable to inhibit the additional formation of thrombin (elevated TAT levels) during CPB.
The inability of heparin to assist inhibition of clot-bound thrombin allows for continued feedback initiation of coagulation and consumption of the endogenous AT (in generating TAT complexes).13,14 Addition of exogenous AT in the AT + UFH groups contributes another source of the inhibitor to give increased levels of TAT (especially accumulating at later time points) since thrombin generation is not being abated. In contrast, ATH inhibits the clot-bound thrombin, which would thus eliminate a major source of activation of the cascade leading to thrombin generation (thus, less thrombin generated and less TAT complexes formed). Summarily, the generally lower levels of circulating TAT complexes during CPB with ATH, relative to the corresponding UFH or AT + UFH treatment groups, was consistent with reduced HITS by ATH.
While the data support ATH as a better anticoagulant for reduction of HITS and TAT during CPB, with little bleeding risk, we attempted to confirm clinical relevance by determining the actual number of microemboli present in porcine brains. Our results indicate that fibrin-microemboli in pig brain sections decreased according to increasing amount of ATH administered (Figure 5). Moreover, this inverse proportionality for emboli versus ATH dose mirrored the trend observed for HITS. Close inspection of select data has even shown that many inordinately high or low HITS corresponded to similar trends for emboli in that animal. These results support the hypotheses that the majority of HITS may represent thromboemboli and that ATH reduces emboli formation. The enhanced reduction in expression of thromboemboli by ATH is again consistent with the fact that the covalent complex readily inhibits clot-bound thrombin compared with UFH,26,42 which would limit growth of fibrin accretion from surface thrombin activity.
This study showed that ATH was the only anticoagulant agent that reduced the HITS rate during CPB to below pre-CPB levels, and this reduction appeared to be dose-dependent. ATH has a more pronounced anticoagulant effect during CPB than UFH, given that less heparin mass is given in the ATH group compared with groups given UFH alone (Table 1). ATH also showed improved thrombin inhibition since less TAT was produced, indicating that less free thrombin was generated when ATH was used during CPB. Thus, covalently linking heparin and AT results in a product with greater in vivo activity compared with heparin alone. Finally, ATH dramatically reduces both CPB-induced HITS rate and microemboli, with comparable bleeding risk, suggesting that ATH may be a safer and more effective anticoagulant alternative for cardiac bypass surgery.
Future studies could assess the effect of ATH on post-CPB cognitive function in an animal model. Subsequently, protocols for human clinical trials may be developed to compare the effectiveness of ATH and UFH in preventing cognitive dysfunction post-CPB. Given that HITS were observed during surgical manipulations prior to the CPB, it may also be of value to assess the possibility for ATH reduction of HITS during initial injury. Recent work has suggested that surface-based anticoagulation may also inhibit thromboembolic complications induced by blood contacting biomaterials. ATH-coated catheters have been shown to have elevated anti-FXa activities/AT binding ratios and low fibrinogen uptake compared with heparin-coated catheters.43 Furthermore, ATH-coated central venous catheters remained patent for over 106 days in rabbits relative to 5-7 days for heparin-coated catheters,44 and ATH-coated catheters were superior at preventing clots in a robust acute jugular vein model.45 Thus, coating bypass circuitry with ATH might further enhance the systemic anticoagulation for elimination of microemboli formation. As demonstrated here, applying ATH treatment during CPB reduces HITS and ameliorates corresponding markers of coagulation. If CPB HITS and emboli are associated with persistent neurological effects, ATH treatment may have the potential for improved clinical care.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 USC section 1734.
Acknowledgments
This work was supported by operating grants from the Heart and Stroke Foundation of Ontario (T6208) and the Ontario Research and Development Challenge Fund in cooperation with Inflazyme, Inc. A.K.C.C. is supported by the Bayer Thrombosis and Hemostasis Research Grant.
Unfortunately, following submission of this manuscript, Dr Klement passed away. His dynamic and enthusiastic pursuit of new treatments and animal models were a cornerstone to the success of our work. Thus, we dedicate this manuscript to his memory.
Authorship
Contribution: P.K. conceived/designed the research, acquired, analyzed, and interpreted the data and made critical revision of the manuscript; L.R.B. acquired, analyzed, and interpreted the data, performed statistical analysis, and made critical revisions to the manuscript; P.L. acquired, analyzed, and interpreted the data; H.W. acquired the data; P.T. conceived/designed the research, acquired, analyzed, and interpreted the results; L.J.S. and N.H. acquired, analyzed, and interpreted the data, and performed statistical analysis; J.I.W. analyzed and interpreted the data and made critical revision of the manuscript; J.H. conceived/designed the research, analyzed and interpreted the data; N.P. analyzed and interpreted the data, performed statistical analysis, and drafted the manuscript; and A.K.C.C. conceived/designed the research, acquired, analyzed and interpreted the data, handled funding and supervision, made critical revisions of the manuscript.
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Correspondence: Anthony K. C. Chan, McMaster University, Department of Pediatrics, Division of Hematology/Oncology, Room 3N27, 1200 Main St West, Hamilton, ON, L8N 3Z5, Canada; e-mail: akchan@mcmaster.ca.



![Figure 5. Comparison of fibrin-emboli in porcine brain sections during hypothermic cardiopulmonary bypass (CPB). (A) Fibrin-emboli per area (given as the square root of fibrin thrombi for all brain sections divided by the total sectional area [in cm2]) and (B) total number of brain emboli. ATH, antithrombin-heparin covalent complex; and UFH, unfractionated heparin. Results are mean ± SD.](https://ash.silverchair-cdn.com/ash/content_public/journal/blood/116/25/10.1182_blood-2010-05-284448/4/m_zh89991061710005.jpeg?Expires=1767840176&Signature=l26EqDhw-GSVRViDJJCHJU5beSJTGEqyBhWtWC~ceci-ND8p9s5oNhBHo417g7DsZpo0A4h3O3dcqqVWub~7dcTLNtezOf7uE7-ouyQq1v3M1OYExgdzlwmGeAwFno6G5GMCkGkCJ9r9BHEOgsQr-JB1KhSCiJee7R9Ltd9rW~rmKIMrMhuEAAiXChiEI98wmX8a0wWJD40z-sjkWBcQGWgQjJsoLy29aI50-c7TdV1ymkf50PUWSXDzFL1tzQKyQrO7cA~FhiYeve4gElfhiHrXZKjKTcgt8VEoxxL0MfaYp2RQyb4YbTGJnMmP9hzFjmdOPSqfZmMEQy5hQyhLBA__&Key-Pair-Id=APKAIE5G5CRDK6RD3PGA)