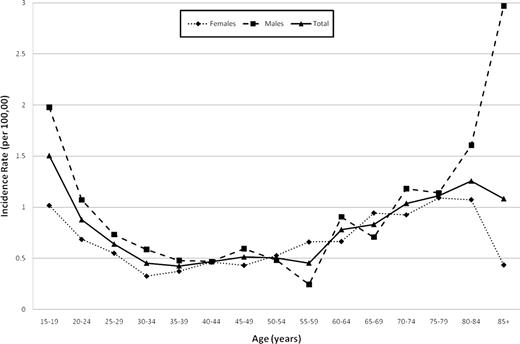
We thank Juliusson and colleagues for their interest in our recent publication1 and agree that it provides a valuable complement to existing data. We acknowledge that Figure 2 in our article is incorrect and thank them for their vigilance. A revised figure is shown below as Figure 1 to this letter, and an erratum is published in this issue of Blood.2 The total incidence line on the original figure was correct; unfortunately, however, the male and female lines had been incorrectly plotted. We would like to apologize to readers for any inconvenience. The error relates solely to this figure and does not affect any other part of the article.
Age-specific incidence of adults with acute lymphoblastic leukemia (ALL) in the North East of England by sex.
Age-specific incidence of adults with acute lymphoblastic leukemia (ALL) in the North East of England by sex.
The differential incidence of ALL in adults over the age of 80 years is intriguing and is now clearly visible in our revised figure, which confirms the study by Juliusson et al. We have previously reported differences in the incidence of lymphoid and myeloid malignancies by sex.3 The reasons for these differences are likely to be numerous and complex; they include prior occupational exposures, lifestyles choices, and competing mortalities. The strong relationship between age and outcome in adult ALL has been well established within both the trial and registry settings.1,4,5 The data presented by the Swedish Registry confirm previous observations. It is clear that outcome in this age group will be strongly related not only to the patients' fitness to receive intensive treatment but also to their willingness to undergo such therapy.
We have previously commented extensively on our findings that the incidence of t(9,22)(q34;q11.2)/BCR-ABL1–positive adult ALL is lower in the United Kingdom compared with many other countries.1,6 Hence, we are not surprised at the data from the Swedish Registry show a slightly higher incidence of t(9;22) adult ALL in Sweden. However, we believe that the more important pieces of data show the clear emergence of a plateau in the incidence of t(9;22). This is in complete agreement with both our data and that from Germany.1,7 Thus, in relation to the increased incidence of ALL in males over the age of 80 years, we can at least conclude that the rise is not due to t(9;22) ALL. Indeed, among 7 males patients over 80 years old with successful cytogenetics, only one had a t(9;22).
Authorship
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Correspondence: Dr Anthony V. Moorman, Leukaemia Research Cytogenetics Group, Northern Institute for Cancer Research, Level 5, Sir James Spence Institute, Royal Victoria Infirmary, Queen Victoria Rd, Newcastle upon Tyne, NE1 4LP, United Kingdom; e-mail: anthony.moorman@ncl.ac.uk.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal